2 Decreased Pain Early Mobilization And Early Return To-PDF Free Download
pain”, “more pain” and “the most pain possible”. Slightly older children can also say how much they are hurting by rating their pain on a 0-10 (or 0-100) scale. Zero is no pain and 10 (or 100) is the worst possible pain. What a child is doing Often children show their pain by crying, making a “pain” face, or by holding or rubbing .
Short-term pain, such as when you suffer a sprained ankle, is called 'acute' pain. Long-term pain, such as back pain that persists for months or years, is called 'chronic' pain. Pain that comes and goes, like a headache, is called 'recurrent' pain. It is not unusual to have more than one sort of pain or to have pain in several places
General discussions of pain often refer simply to three types: 1) Acute (brief that subsides as healing takes place) 2) Cancer 3) Chronic non-malignant pain - "persistent pain" Classification of pain by inferred pathology: 1) Nociceptive Pain 2) Neuropathic Pain (McCaffery & Pasero, 1999) Nociceptive Pain A. Somatic Pain B. Visceral Pain
Knee Pain 1 Knee Pain 2 Knee Pain 3 Knee Pain 4 Knee Pain 5 Lateral Knee Pain Medial Knee Pain Patella Pain 1 Patella Pain 2 Shin Splint. 7 Section 6 Ankle/Foot Big Toe 89 . For additional support, wrap another tape around the last finger joint. Step 3. No stretch is applied during application. 30 Step 1 Step 2 Finger Pain. 31 Requires;
based recommendations for management of postopera-tive pain. The target audience is all clinicians who manage postoperative pain. Management of chronic pain, acute nonsurgical pain, dental pain, trauma pain, and periprocedural (nonsurgical) pain are outside the scope of this guideline. Evidence Rev
severe pain. Treatment of acute pain When assessing a patient with acute pain, the nurse should consider: The patient's report of pain or observation of pain (such as the number on a 1 to 10 scale). The patient's functional ability. The patient's level of consciousness. The site of pain and the cause.
AR 500-5, Army Mobilization, Army mobilization is a complex activity. To understand how the Army mobilizes, an individual requires knowledge of the authorities for mobilization, the process actors and the sequence of activities necessary to bring a unit or Soldier onto active duty. b. HQDA EX
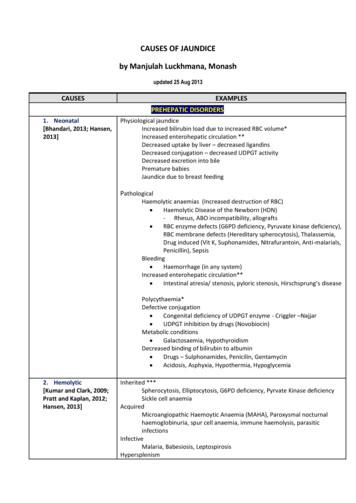
1. Neonatal [Bhandari, 2013; Hansen, 2013] Physiological jaundice Increased bilirubin load due to increased RBC volume* Increased enterohepatic circulation ** Decreased uptake by liver – decreased ligandins Decreased conjugation – decreased UDPGT activity Decreased excretion into bile Premature babies Jaundice due to breast feeding Pathological
the adjusted death rate (Figure 5.1.a) decreased by 29%. The unadjusted death rate for the dialysis population decreased by 27%, while the adjusted death rate decreased by 29%. The unadjusted death rate for the transplant population decreased by 2%, while the adjusted death rate decreased by 40%. Differences between the unadjusted and adjusted
Overview of Essentials of Pain Management 1. Assess pain intensity on a 0 ‐10 scale in which 0 no pain at all and 10 the worst pain imaginable. Determine if the pain is mild (1‐4), moderate (5‐6), or severe (7‐10). 3. Assess the character of the patient’s pain and determine whether it is nociceptive, neuropathic, or both.
chronic pain. Musculoskeletal pain, particularly related to joints and the back, is the most common type of chronic . pain. 2,8. This systematic review thus focuses on five of the most common causes of musculoskeletal pain: chronic low back pain, chronic neck pain, osteoarthritis, fibromyalgia and chronic tension headache. Rationale for This .
Pain Self-Management Strategies If you have chronic pain, this guide can help you manage your pain. Richard Wanlass, Ph.D. & Debra Fishman, Psy.D. UC Davis Medical Center, Department of Physical Medicine & Rehabilitation, 060411 . This project was partially funded by a grant . from the Robert Wood Johnson Foundation.File Size: 852KBPage Count: 16Explore furtherChronic Pain Self-Management - Veterans Affairswww.mentalhealth.va.govChronic Pain Self-Management Resourcesdepts.washington.eduPain Management - NHS Ayrshire and Arranwww.nhsaaa.netPAIN MANAGEMENT BEST PRACTICES - HHS.govwww.hhs.govSeven Practical Tips for Coping with Physical Pain .www.psychologytoday.comRecommended to you b
Your Role in Managing Your Pain Self-Management Programs Online Resources Recommended Apps Support Groups Pain Clinics Pain Management Books General Books on Pain Pathophysiology or How Pain Persists Books on Living with Pain from a Personal Perspective Healthy Living Mental Health Mind-Body Strategies for
pain Quality of pain important in differentiating OA or medical origin Location Anterior Jointline Radiating Aggravating activities Pain with weight bearing vs. rest Pain going up or down stairs or a slope Morning pain Start up pain do you sleep with a pillow between yo
Pain Assessment Questionnaire Name: _ INFORMATION ABOUT YOUR PAIN PROBLEM 1. What is your main reason for coming to the pain clinic today? _ 2. How long have you been in pain? _ 3. Briefly describe how your pain started? _ 4. Do you have any of the follo
11 Definitions Chronic pain: Pain that persists beyond normal tissue healing time, which is assumed to be 3 months. Noncancer pain: All pain outside of cancer pain and pain at end of life. Chronic opioid therapy: Daily or near-daily use of opioids for at least 90 days, often indefinitely. Physical dependence: A state of adaptation manifested by a
Acute pain management has seen many changes in the assessment and the available therapies. Acute pain is being identified as a problem in many patient populations. Beyond postoperative, traumatic and obstetric causes of pain, patients experience acute on-chronic pain, acute cancer pain or acute pain from medical conditions.
2.5 To carry out clinical research in the area of post-operative pain management. 2.6 To assist with Nursing Education with respect to acute pain management. 2.7 To develop protocols for the various methods of pain relief. 3. METHODS OF PAIN RELIEF The Acute Pain Service has a broad approach to postoperative pain relief and includes many
Measured pain level and catastrophizing Early (0-15 min) Mid (15-30 min) Late (30-35 min) Higher early catastrophizing increased pain Higher early pain did NOT increase catastrophizing J Pain. 2010 Sep;11(9):876-84 Khan Am J Surg 2011, Edwards 2006, Lewis 2012 Catastrophizing Worsens Pain
Decreased heart rate Decreased blood pressure Slowed breath rate Decreased need for oxygen Increased blood flow Reduced muscle tension Decreased incidence of headaches and muscle pain Fewer emotional responses such as anger, crying, anxiety, apprehension, and f
ute to the stroke unit effect. Early mobilization, in its many guises, is one component of care proposed to contribute to the survival and recovery benefits of stroke unit care.1 This topical review provides an overview of the current evidence, research, and practice recommendations for early mobiliza-tion after stroke.
Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: Results of the pain in emergency medicine initiative (PEMI) multicenter study. Journal of Pain. 2007;8:460-466. Silka PA, Roth MM, Morena G, Merrill L, Geiderman JM. Pain scores improve analgesic administration patterns for trauma patients in the emergency department.
ancillary pain generators3. Acupuncture (AC) has been used as an alternative to more traditional treatments for musculoskeletal pain, because it inactivates the neural loop of the trigger point (pain-contraction-pain), reducing pain, and reduces muscular over-contraction. Acupuncture stimulates points on the body via the insertion of needles to
Pain Management Injection Therapies for Low Back Pain Structured Abstract Objectives. Low back pain is common and injections with corticosteroids are a frequently used treatment option. This report reviews the current evidence on effectiveness and harms of epidural, facet joint, and sacroiliac corticosteroid injections for low back pain conditions.File Size: 1MB
pain, neck and back pain, fibromyalgia, arthritis pain, burn pain, postoperative pain) 2. Integration of approaches: cognitive behavioral treatments, combined behavioral and drug treatments; economic benefits of integrating treatment 3. Stages of behavioral change and their effect on readiness to adopt self-management
ical, biomechanical and psychosocial contributors to pain in sport. consIderAtIons About p AIn A fundamental shift in the understanding of pain in sport is warranted. Pain is not synonymous with sport injury, that is, injury may occur without pain, and pain may develop or persist indepen
ABCs of Pain Management Recommended by the Agency for Health Care Policy and Research (AHCPR), USA A-Ask about pain regularly.Assess pain systematically. B-Believe the patient and family in their reports of pain and what relieves it. C-Choose pain control options appropriate for the patient, family, and setting. D-Deliver
Pain assessment is key to determining the degree and duration of pain treatment but should not replace the adage of treating predict- able pain Perioperative pain extends beyond 24 hours and should be managed accordingly Practice preventive (preemptive) pain management – initiat
Pain in Palliative Care Pain Pain is one of the most common symptoms in palliative care. Pain can also be a much feared symptom which can contribute to its intensity. The aim of palliative care is to allow patients to be pain free or
Oct 15, 2005 · Pain Neuroscience Education: Teaching People About Pain 2017 Property of Adriaan Louw –not to be copied without permission 4 Representation Pain mechanisms Onion skins Beliefs/fears/threats Biomechanics Pathoanatomy Evolutionary Biology Louw A, Butler DS. Chronic Pain. In: S.B. B, Manske R, eds. Clinical
2 Sleep and Pain: Questions of Directionality Historically it has been assumed that sleep disturbance was secondary to pain. The current view is that insomnia is typically co- morbid with pain. A growing body of data suggests that insomnia can lead to or worsen pain. Emerging data also suggest that improving sleep may improve co-morbid pain.
pain was only on movement, but now is present even at rest. On movement pain is about a 7 -9. At rest, pain is about a 5. The pain is on the front and the side of the shoulder. It bothers the patient at night when she is sleeping. She is having great difficulty with mobility due to the shoulder pain. Walking with crutches or
with pain. the creatures cause pain by being born, and live by inflicting pain, and in pain they mostly die. in the most complex of all the creatures, man, yet another quality appears, which we call reason, whereby he is enabled to foresee his own pain which henceforth is preceded with acute mental suffering, and to foresee
1. Learn how to use the PDMP to address pain management for various patient populations and pain types; 2. Understand the basic nature of pain for different patient populations and how to manage their pain using the PDMP as a clinical tool; and 3. Discuss different ways of treating patient pain that do not involve the immediate use of opioids.
1. Determine patient's pain score assessment using standard pain scale. a. Less than 4 years old: Observational scale (e.g. Faces, Legs, Arms, Cry, Consolablity [FLACC] or Children's Hospital of Eastern Ontario Pain Scale (CHEOPS) b. 4-12 years old: Self-report scale (e.g. Wong Baker Faces, Faces Pain Scale [FPS], Faces Pain Scale Revised .
Complex regional pain syndrome (CRPS) is a chronic pain condition characterized by spontaneous and evoked regional pain, usually beginning in a distal extremity, that is dispro - portionate in magnitude or duration to the typical course of pain after similar tissue trauma. 1 CRPS is distinguished from other chronic pain conditions
Complex regional pain syndrome is an uncommon form of chronic pain that usually affects an arm or a leg. Complex regional pain syndrome typically develops after an injury, surgery, stroke or heart attack, but the pain is out of proportion to the severity of the initial injury. The cause of complex regional pain syndrome isn't clearly understood.
Shoulder Pain: Effectiveness of Microcurrent Treatment Subtitle: Effectiveness of Pro-Sport Microcurrent Electro-Therapy for Pain in a Single Outpatient Visit with Patients Exhibiting Shoulder pain and/or symptoms consistent with Shoulder Pain: PRO-SPORT Open-Label Shoulder Pain Study Thomas Lenahan, D.C. Tammy Lahutsky, Avazzia Inc.
The International Association for Study of Pain (IASP) defines acute neck pain as lasting less than 7 days, subacute neck pain lasting between 7 days and 3 months, and chronic neck pain lasting 3 months and longer. 9,10. Pathophysiology . Neck pain pathophysiology is a complex combination of mechanical and chemical processes,
Identify trauma patients who are candidates for pharmacologic pain management ! Describe the age appropriate pain scale to assess the pain level of traumatic patient ! Explain the narcotic analgesics used to relieve moderate to severe pain in the trauma patient ! Identify the serious adverse effects of pain medication !