Specialty Requirements By Category Microbiology Categories .
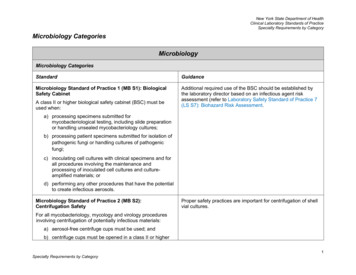
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiology CategoriesMicrobiologyMicrobiology CategoriesStandardGuidanceMicrobiology Standard of Practice 1 (MB S1): BiologicalSafety CabinetAdditional required use of the BSC should be established bythe laboratory director based on an infectious agent riskassessment (refer to Laboratory Safety Standard of Practice 7(LS S7): Biohazard Risk Assessment.A class II or higher biological safety cabinet (BSC) must beused when:a) processing specimens submitted formycobacteriological testing, including slide preparationor handling unsealed mycobacteriology cultures;b) processing patient specimens submitted for isolation ofpathogenic fungi or handling cultures of pathogenicfungi;c) inoculating cell cultures with clinical specimens and forall procedures involving the maintenance andprocessing of inoculated cell cultures and cultureamplified materials; ord) performing any other procedures that have the potentialto create infectious aerosols.Microbiology Standard of Practice 2 (MB S2):Centrifugation SafetyProper safety practices are important for centrifugation of shellvial cultures.For all mycobacteriology, mycology and virology proceduresinvolving centrifugation of potentially infectious materials:a) aerosol-free centrifuge cups must be used; andb) centrifuge cups must be opened in a class II or higherSpecialty Requirements by Category1
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology CategoriesStandardGuidancebiological safety cabinet (BSC).Microbiology Standard of Practice 3 (MB S3): QualityControl Stock CulturesThe laboratory must have quality control procedures for allstocks cultures to minimize contamination or alteration ofrelevant characteristics.Microbiology Standard of Practice 4 (MB S4): MicrobialGrowth MediumMaintenance of stock cultures should be standardized in amanner that minimizes the opportunity for contamination oralteration of relevant characteristics. Stock cultures shouldconsist of low-passage material rather than laboratory-adaptedhigh passage material.Validated patient isolates, proficiency testing specimens, orcommercially prepared controls may be used unless otherwiserequired by manufacturer.Media may be tested concurrent with initial use provided QCresults are reviewed prior to release of patient results.Each lot or shipment of commercially prepared or in-houseprepared media must be tested:a) on-site for growth, selectivity, and/or inhibition andbiochemical responses; orb) by criteria established by the manufacturer or thelaboratory in absence of manufacturer instructions.Quality control (QC) checks for sterility, growth,selectivity and/or inhibition and biochemical responsesneed not be retested by the laboratory provided that:i.for each shipment or lot of media, the laboratoryhas documentation on the media label, packageinsert, technical manual, or other document, thatthe manufacturer’s or in-house QC practicesconform to specifications; andSpecialty Requirements by Category2
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology CategoriesStandardii.Guidancethe laboratory documents receipt and conditionof each shipment or lot of media, and notifies themedia manufacturer or in-house preparer of:- cracked Petri dishes;- unequal filling of plates;- cracked media in plates;- hemolysis;- freezing;- excessive number of bubbles; or- contamination.Microbiology Standard of Practice 5 (MB S5): ExpirationDate Prepared In-HouseThe expiration date for each batch of in-house preparedmicrobiological media must not exceed eight (8) weeks fromthe preparation date for plated and non-screw cap tubed mediaand six (6) months from the preparation date for screw captubed media.Microbiology Standard of Practice 6 (MB S6): ReportsIn addition to the requirements in Reporting Standard ofPractice 2, test reports must include:a) the test method;b) qualifiers for viral cultures that are incomplete oruninterpretable or when isolate identification isSpecialty Requirements by Categorya) Examples of assay methodology include culture, EIA, PCR,etc. Specific test systems are not required to be listed on atest report.3
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology CategoriesStandardGuidanceconsidered presumptive, i.e., an isolate is not confirmedby a specific viral identification system; andc) a recommendation for follow-up testing, if appropriate.Microbiology Standard of Practice 7 (MB S7): LaboratoryResponse NetworkIn addition to the requirements for Test Procedure ContentStandard of Practice 1, the laboratory must have a section inthe standard operating procedure describing policies andpractices related to their activities as a Laboratory ResponseNetwork (LRN) sentinel laboratory, if applicable, including:a) maintaining updated guidelines and protocols related tothe testing, identification and reporting of select andemerging infectious agents including informationregarding special handling and safety practices to beemployed;b) providing staff with information regarding the biosafetylevel(s) (BSL) recommended for the microbiologicaltesting being performed and identifying the highest BSLavailable for each category of microbiological testing;c) identifying the LRN reference laboratory for their facilityand contact information for individual(s) to be contactedif a select agent is suspected; andd) distribution of information to health care providersregarding specimen collection and submissioninstructions that should be followed when infection witha select agent or other infectious agent requiring specialSpecialty Requirements by CategoryLaboratories holding a New York State clinical laboratorypermit in either Bacteriology or Virology are currentlyconsidered LRN sentinel laboratories, unless designated as anLRN reference laboratory.Information regarding laboratory testing for select andemerging infectious agents is available to all laboratories on theAmerican Society of Microbiology website.The Wadsworth Center may define the levels of testing (e.g.,rule out only) and identification (e.g., presumptive only) and thereporting pathway for a particular agent. The WadsworthCenter’s LRN distributes this information as needed to sentinellaboratories by e-mail or e-fax to the laboratory director andposts these announcements on the HCS.New York State and New York City LRN reference laboratorycontacts and other LRN information is available on theWadsworth Center LRN website. The Wadsworth Center LRNprogram staff can be contacted at:LRNexec@health.state.ny.us.Biosafety levels and associated recommendations andpractices are described in the CDC publication “Biosafety inMicrobiological and Biomedical Laboratories” (BMBL) and onthe CDC website at: https://www.cdc.gov/labs/BMBL.html.Laboratories must comply with infectious disease reporting4
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology CategoriesStandardhandling is suspected.Microbiology Standard of Practice 8 (MB S8): Select AgentInventoryThe laboratory must ensure that all samples and theirderivatives suspected or confirmed to contain select agents areaccounted for until laboratory findings establish the absence ofa select agent. If a select agent is confirmed, documentation ofits transfer including record of appropriate packing and shippingor destruction within seven (7) days must be completed.Specialty Requirements by CategoryGuidancerequirements as outlined in the Public Health ReportingStandards of Practice 1 and 2.A list of select agents (Biological Diseases/Agents List) can befound at the federal Centers for Disease Control andPrevention website at: http://www.selectagents.gov.Laboratories must comply with pertinent items of the SelectAgent Rule (e.g., disposal/transfer of select agents)Inventory and tracking documentation should include theidentity of all individuals accessing such materials, as well ascompletion of APHIS/CDC forms 3 (Report of Theft, Loss orRelease of Select Agents or Toxins) and 4 (Report ofIdentification of a Select Agent or Toxin) for organisms andtoxins isolated from clinical specimen. Additional information isavailable at: http://www.selectagents.gov.5
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiology Nucleic Acid (MNA) Amplification AssayMicrobiologyMicrobiology Nucleic Acid (MNA) Amplification AssayStandardGuidanceMicrobiology Nucleic Acid Amplification Assay Standardof Practice 1 (MNA S1): Quality Control Samples forLaboratory Developed TestsThis standard applies to controls to be used with laboratorydeveloped tests (LDTs).Each assay protocol for all laboratory developed tests (LDTs)for MNAA assays and modified FDA approved assays mustmeet the requirements in Quality Control Standard of Practice2, 3 and 4 to define the acceptable detection range for allcontrols and each run must include at least:a) one (1) control capable of detecting amplificationinhibition by patient specimens unless the LDTapproved by the Department exempts the requirement;b) for qualitative single target assays, a negative controland a low range positive control that assess the entireassay, including specimen preparation/extraction(except for sequence based assays);c) for qualitative multi-target assays at least one (1)specific target positive control;d) for quantitative assays, a negative control and at leasttwo (2) positive controls that assess the linear range ofthe assay including one (1) control within two (2) logs ofthe lower limit of quantitation (LLOQ) and one (1)control in the upper half of the linear range includingspecimen preparation/extraction; ande) additional negative controls in laboratories thatSpecialty Requirements by CategoryInformation on Departmental approval of LDTs is available cal-labs/obtainpermit/test-approval.Negative controls including template-free mastermix controlsnot only serve to identify technical and/or reagent issues butalso help identify amplicon contamination. The negativecontrols may include a reagent processing control that servesas both a template-free mastermix reagent control as well as aprocessing/extraction negative control.For laboratories preparing mastermix to be used on multipleinstruments, the template-free mastermix control should beutilized for each run of each instrument.a) Inhibition controls may be excluded if there are sufficientdata showing that the inhibition rate is less than one (1)percent for a specimen type for the assay. It is possible toextend inhibition data to other analytes when applying thesame extraction procedure and specimen matrix andutilizing the same amplification methodology.a) Inhibition controls are not required if the run includesisolates only and not patient specimens.b, c)A low-range positive is defined as having a value of not6
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology Nucleic Acid (MNA) Amplification AssayStandardmanipulate amplicon but do not use separate rooms forpre- and post-amplification processes.Guidancemore than ten (10) fold above the assay detection limit.b, c)For multiplex assays, a low range control is required foreach target. These may be run on a rotating basis and mayinclude pools of three (3) to four (4) targets.d) Processes that involve manipulation of amplicon includeconventional PCR and nucleic acid sequencing.d) It is recommended that the number of negative controlsequal at least two (2) percent of the patient specimen testnumber and that these are interspersed randomlythroughout patient specimens (e.g. two (2) per 96-wellplate).Microbiology Nucleic Acid Amplification Assay Standardof Practice 2 (MNA S2): Quality Control Samples forSequencing AssaysEach sequencing assay must include a:a) negative amplification control;b) negative sequencing control;c) positive sequencing control; andd) positive amplification and inhibition controls whentesting primary specimens for the detection oridentification of an infectious agent, unless anindividualized quality control plan (IQCP), performedaccording to Quality Control Standards of Practice 2, 3and 4 is approved by the Department as a laboratorySpecialty Requirements by CategoryInformation on Departmental approval of LDTs is available cal-labs/obtainpermit/test-approval.Laboratories using a core facility do not need to providenegative and positive sequencing amplification controls if theassay performed by the core facility includes negative andpositive sequencing controls.a, b)The negative amplification control may also be used as thenegative sequencing control.c) Purified plasmid that is supplied with a commerciallyavailable kit may be used as a positive sequencing control.Previously tested and well characterized PCR product ofthe target from clinical samples can also be used as7
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology Nucleic Acid (MNA) Amplification AssayStandarddeveloped test (LDT).Guidancesequencing controls.d) Positive amplification controls and inhibition controls arenot necessary when performing sequencing on clinicalisolates.d) Positive amplification and inhibition controls may be omittedwhen testing primary specimens for genotyping assays forprognostic purposes.Microbiology Nucleic Acid Amplification Assay Standardof Practice 3 (MNA S3): Reports for Laboratory DevelopedSequence-based AssaysIn addition to the requirements in Reporting Standard ofPractice 2, reports must include disclaimers on all infectiousagent-based sequencing tests from primary specimens thathave no amplification or genotype results.Microbiology Nucleic Acid Amplification Assay Standardof Practice 4 (MNA S4): Task Separation for FDA-ApprovedClosed System Amplification TestFor a closed system amplification test (CSAT), the laboratorymust:a) handle, process, and store clinical specimens, reagentsand supplies in a manner that prevents exposure toamplicon, plasmids, and culture-amplified materials;andSpecialty Requirements by CategoryPositive amplification and inhibition controls may be omittedwhen testing primary specimens for genotyping assays forprognostic purposes. For assays that lack positive amplificationand inhibition controls, a disclaimer on the report is needed todocument that the result may be due to the following: infectiousagent was below the limit of detection in the sample, mutationswere present in the genome, or inhibitors were present in thesample that prevented amplification.A CSAT refers to an assay in which all steps, including postamplification steps, are performed and contained within aclosed system. A closed system is defined as an instrument inwhich the patient specimen is directly added to the test unit,device, or cartridge, and then the testing process is initiatedwith no additional external manipulation or addition of reagentsunless approval is received by the Department.CSAT instrumentation should be segregated from areas inwhich specimens are routinely processed in order to avoidcross-contamination.8
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMicrobiology Nucleic Acid (MNA) Amplification AssayStandardb) locate the instrument in an area free of open ampliconsystems.Specialty Requirements by CategoryGuidanceAn individual performing CSAT may return to pre-amplificationareas since the closed systems do not release amplicon intothe environment provided that assay and discard proceduresare followed.9
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by rdGuidanceLaboratories that perform testing for Chlamydia culture must follow applicable Virology Culture standards.Bacteriology Standard of Practice 1 (BT S1): ReagentQuality ControlUnless an Individualized Quality Control Plan (IQCP) isestablished according to Quality Control Standards of PracticeS2, S3 and S4, the laboratory must check positive andnegative reactivity with control organisms as follows:a) each day of use for beta-lactamase and all stains otherthan Gram stain;b) each week of use for Gram stain; andc) every six (6) months for antisera.Bacteriology Standard of Practice 2 (BT S2): Urine CultureInoculating LoopsVerification of calibration of non-disposable urine cultureinoculating loops must be performed monthly or done asspecified in manufacturer instructions.Bacteriology Standard of Practice 3 (BT S3): AnaerobicContainersThe environmental conditions of anaerobic bags, jars, andglove boxes must be monitored and documented each day ofuse.Specialty Requirements by Categoryc) Polyvalent antisera should be tested with at least one (1)organism from each polyvalent group.Verification of calibration may be performed using a blue-dyemethodology or by using a calibrated drill bit. Verification ofnon-disposable loops used in automated instruments can beperformed during manufacturer provided preventativemaintenance.An oxygen sensitive indicator such as methylene blue,resazurine, or a control culture of Clostridium novyi B should beplaced in anaerobic jars or chambers to ensure anaerobicconditions are met.10
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by cteriology Standard of Practice 4 (BT S4): Aerobic BloodCulturesSubcultures need not be done on blood cultures if the bottlesare monitored for five (5) days.Macroscopically negative aerobic blood cultures must besubcultured before discarding.Antimicrobial susceptibility Testing: Disk diffusion and minimal inhibitory concentrationBacteriology Standard 5 (BT S5): Defining AntibioticPanelsIn addition to the requirements for Test Procedure ContentStandard of Practice 1, the standard operating procedure mustdefine antibiotic panels appropriate to the specimen source andorganism isolated.Guidelines should be established for the number and type ofantibiotics tested and/or reported for organisms isolated fromdifferent sources. It is recommended that, in a hospital setting,the laboratory periodically reviews the most current formularyestablished by the pharmacy and/or the Infection ControlCommittee.Disk diffusion methods (Standards 6-9)Bacteriology Standard of Practice 6 (BT S6): Media QualityControl for Disk Diffusion MethodsEach batch of media used for antimicrobial susceptibility testingmust be verified with the appropriate reference organismsstrains before, or concurrent with, initial use.Bacteriology Standard of Practice 7 (BT S7): AntibioticQuality Control for Disk Diffusion MethodsEach new lot of antimicrobial disks must be verified with theappropriate reference organisms before, or concurrent with,initial use.Specialty Requirements by CategoryIf performed concurrently with patient testing, quality control(QC) results must be reviewed prior to release of patientresults.If performed concurrently with patient testing, quality control(QC) results must be reviewed prior to release of patientresults.11
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by cteriology Standard of Practice 8 (BT S8): AntibioticDisk DistributionGenerally, no more than twelve (12) disks should be distributedon a one hundred and fifty (150) mm petri plate and no morethan five (5) disks on a one hundred (100) mm plate. ForHaemophilus species, Neisseria gonorrhoeae, andStreptococcus species (including Streptococcus pneumoniae),no more than nine (9) disks per one hundred and fifty (150) mmplate and no more than four (4) disks per one hundred (100)mm plate should be used.Antibiotic disks must be evenly distributed over the cultureplate not less than fifteen (15) mm from the outer edge of theplate and no closer than twenty-four (24) mm from center tocenter except when specifically directed otherwise by themanufacturer’s directions.Bacteriology Standard of Practice 9 (BT S9): Disk DiffusionQuality Control Frequency, Assessment and RecordingFor antimicrobial susceptibility disk diffusion testing, thelaboratory must:a) use the appropriate control organism(s) each day oftesting; andb) record zone sizes for each antimicrobial quality controltest; orc) meet the requirements of Quality Control Standard ofPractice 2, 3 and 4; andd) document that quality control results are withinestablished zone diameter ranges.Specialty Requirements by Categoryb) Zone sizes may be measured using a ruler, sliding calipers,templates, or other appropriate measurement devices.d) The laboratory may establish zone diameter ranges usingrelevant references.12
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by nimal inhibitory concentration methods (MIC) (standards 10-11)Bacteriology Standard of Practice 10 (BT S10): ReagentQuality Control for Minimum Inhibitory ConcentrationMethodsEach batch of materials and reagents used for minimuminhibitory concentration (MIC) antimicrobial susceptibility testingmust be verified with the appropriate reference organismsbefore, or concurrent with, initial use.Bacteriology Standard of Practice 11 (BT S11): MinimumInhibitory Concentration Quality Control Frequency,Assessment and RecordingFor minimum inhibitory concentration (MIC) antimicrobialsusceptibility testing, the laboratory must:a) use the appropriate control organism(s) each day oftesting; andb) record the MIC values for each antimicrobial qualitycontrol test; orc) meet the requirements of Quality Control Standard ofPractice 2, 3, and 4; andd) document that quality control results are withinestablished MIC ranges.Specialty Requirements by Categoryd) The established MIC range is the acceptable interpretivecriteria for that drug-microorganism combination used forquality control.13
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by gyStandardGuidanceMycobacteriology Standard of Practice 1 (TB S1):Specimen CentrifugationSpecimens must be centrifuged for a minimum of fifteen (15)minutes at greater than or equal to 3,000 x g.Mycobacteriology Standard of Practice 2 (TB S2): CrossContaminationBatch staining with jars or dishes should not be utilized. Thisdoes not apply to automated staining systems.The laboratory must design procedures that minimize thepossibility of cross-contamination including, but not limited to:a) opening and manipulating only one (1) patient specimenat a time in a biological safety cabinet (BSC); andb) excluding positive control organisms from the BSCwhile patient specimens are being processed.Mycobacteriology Standard of Practice 3 (TB S3): StainingQuality ControlFor mycobacteriological staining, a positive and negativecontrol must be run with each new shipment or lot of stain andeach time of use or meet the requirements of Quality ControlStandards of Practice 2, 3 and 4.Mycobacteriology Standard of Practice 4 (TB S4):Fluorochrome StainsCarbol fuchsin is the preferred stain for confirmation in newlydiagnosed patients.Laboratories using fluorochrome staining must confirm positiveSpecialty Requirements by Category14
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by ceresults in newly diagnosed patients by:a) carbol fuchsin stain; orb) independent evaluation by a second person.Mycobacteriology Standard of Practice 5 (TB S5):Reporting Smear ResultsIn addition to report requirements in Reporting Standard ofPractice 2, reports of all smear stain results must:a) be communicated to the ordering physician or otherauthorized person within thirty (30) hours of the receiptof the specimen; anda) Reporting time should be periodically monitored to ensurecompliance.b) indicate that culture is being performed.Mycobacteriology Standard of Practice 6 (TB S6):Laboratories testing only Smears - Specimen Submissionand Result NotificationLaboratories testing only smears must:a) refer all specimens for culture to a laboratory holding avalid New York State clinical laboratory permit in thecategory of Mycobacteriology; andb) notify the reference laboratory if the specimen beingsent is the first smear positive specimen from thepatient.Specialty Requirements by Categoryb) This notification is essential so that the reference laboratorycan comply with Mycobacteriology Sustaining Standard ofPractice 13 (TB S13).b) The patient smear history can be reviewed in the laboratoryinformation system of the referring laboratory.15
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by ceMycobacteriology Standard of Practice 7 (TB S7):Retention of Stained SlidesFluorochrome slides will fade with time, so they should beretained in the dark. The slides may be restained with a carbolfuchsin method if necessary.Stained slides of direct smears from primary specimens mustbe retained until the final culture report has been issuedaccording to Document and Specimen Retention Standard ofPractice 10.Mycobacteriology Standard of Practice 8 (TB S8): NucleicAcid AmplificationNucleic acid amplification testing for M. tuberculosis complexmust be performed on all primary respiratory specimens thattest smear positive and are from patients who have not beenpreviously diagnosed with tuberculosis.Non-amplified nucleic acid assays do not satisfy this standard.Specimens from patients with a known history of nontuberculous Mycobacteria (NTM) infection and without clinicalsuspicion of tuberculosis (e.g., cystic fibrosis patients) do notneed nucleic acid amplification testing performed.If the laboratory does not have the capability to perform nucleicacid amplification testing, an additional respiratory specimenmust be immediately sent to a laboratory holding a valid NewYork State clinical laboratory permit in the category ofMycobacteriology to perform nucleic acid amplification.Mycobacteriology Standard of Practice 9 (TB S9): MediaFor all specimens other than blood, at least one (1) solid andone (1) liquid medium must be inoculated for culturing acid fastbacilli (AFB).Specialty Requirements by Category16
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by ceMycobacteriology Standard of Practice 10 (TBS 10):Culture PurityTo ensure that positive liquid cultures are not contaminated, thelaboratory must perform:a) acid fast staining microscopy; andb) plating on enriched, non-selective culture media (e.g.,Chocolate agar).Mycobacteriology Standard of Practice 11 (TBS 11):Retention of IsolatesMultiple isolates may be requested from the same patient forpublic health investigation.Laboratories must save all original and subsequent M.tuberculosis complex isolates for twelve (12) months accordingto Document and Specimen Retention Standard of Practice 10.Isolates may be retained on appropriate media and stored at-70 to -80 degrees Celsius.Mycobacteriology Standard of Practice 12 (TB S12):Identifying M. avium complex and M. gordonaeDetection of M. avium complex and M. gordonae bybiochemical methods must be confirmed by another method.Mycobacteriology Standard of Practice 13 (TB S13):Submission of Isolates to a Public Health LaboratoryLaboratories must submit to either the Wadsworth Center orthe New York City (NYC) Public Health Laboratory:Specialty Requirements by CategoryIsolates recovered from patients residing in New York City(NYC) should be submitted to the NYC Public HealthLaboratory; isolates from patients residing outside of NYCshould be submitted to the Wadsworth Center. Refer to thelatest version of the Laboratory Reporting and Specimen17
New York State Department of HealthClinical Laboratory Standards of PracticeSpecialty Requirements by CategoryMicrobiologyMycobacteriologyStandarda) all initial isolates of Mycobacterium tuberculosiscomplex from newly diagnosed patients by the nextbusiness day of a positive identification of M.tuberculosis complex; andb) all M. tuberculosis complex isolates presenting achange in susceptibility pattern. The initial isolate andthe subsequent isolate demonstrating an alteredsusceptibility pattern must both be submitted.Mycobacteriology Standard of Practice 14 (TB S14):Referral of Positive Isolates for Susceptibility TestingIf susceptibility is not performed in-house, the initial positive M.tuberculosis complex culture on a newly diagnosed patientmust be referred by the next business day for susceptibilitytesting to a laboratory holding a valid New York State clinicallaboratory permit in the category of Mycobacteriology.Specialty Requirements by CategoryGuidanceSubmission Requirements for Communicable Diseasesavailable at http://www.wadsworth.org/regulatory/clep/laws.a) To expedite genotype testing, an aliquot of at least one (1)ml of the primary broth medium should be sent rather thanwaiting for a mature subculture on a slant.b) A change in drug susceptibility may be identified by thehealth care provider or through the patient’s history.Whenever possible, the initial positive culture (i.e., equal to orgreater t
Microbiology Categories. Microbiology . Microbiology Categories Standard . Guidance; Microbiology Standard of Practice 1 (MB S1): Biological . Additional required use of the BSC should be established by the laboratory director
An Introduction to Clinical Microbiology Susan M. Poutanen, MD, MPH, FRCPC . Objectives 1. To provide an introduction to a typical microbiology laboratory 2. To address specific microbiology laboratory test issues as they apply to public health. Department of Microbiology Who we are Shared microbiology service between TML (UHN & MDS) and MSH
Industrial microbiology Medical and pharmaceutical microbiology Rumen microbiology Space microbiology 1.2 Definitions Milk and milk products occupy a more significant role in the human food profiles. The study of microorganisms that are associated with milk and milk products in all aspects is defined as "Dairy Microbiology". 1.2 .
Title: Clinical Microbiology Users Handbook QP Ref: LH-MIC-GEN-G-001v1 Author: Jennifer Challoner & Alex Duggan Authorised by: Microbiology Specialty board Created Date:23rd April 2020 Disposal date: 22nd April 2050 Page 1 of 75 9693 Microbiology Laboratory Handbook Microbiology Laboratory North Tyneside General Hospital Rake Lane North Shields Tyne & Wear NE29 8NH This SOP supersedes all .
GENERAL MICROBIOLOGY Requirements in this section apply to ALL of the subsections in the microbiology laboratory (bacteriology, mycobacter iology , mycology , par asitology , molecular microbiology , and virology). When the microbiology depar tment is inspected by a team, each member of the t
For most BCBSAZ members, specialty copay tiers (A, B, C, or D) apply. Tier Description A Specialty Medications, Low Cost Share B Specialty Medications, Moderate Cost Share C Specialty Medications, Moderately High Cost Share D Specialty Medications, Highest Cost Share Plans may include specialty medications at varying cost share tiers. Questions?
General Microbiology Manual _ Abdelraouf A. Elmanama Ph. D Microbiology 7 Introduction Welcome to the microbiology laboratory. The goal of the laboratory is to expose students to the wide variety of lives in the microbial world. Although the study of microbiology includes
Microbiology H Core 4 3 30 70 100 4 MBH- 204 Food Microbiology H Core 4 3 30 70 100 4 MBS- 205 Bioinformatics S Core 2 2 15 35 50 2 Practical MBP- 206 Microbial Genetics, Molecular Biology Pract 4 4 30 70 100 4 MBP- 207 Environmental Microbiology and Food Microbiology Pract 4 4 30 70 100 4
Classical approach to management is a set of homogeneous ideas on the management of organizations that evolved in the late 19 th century and early 20 century. This perspective emerges from the industrial revolution and centers on theories of efficiency. As at the end of the 19th century, when factory production became pervasive and large scale organizations raised, people have been looking for .