Review Of Applications Of Microneedling In Dermatology.
Himmelfarb Health Sciences Library, The George Washington UniversityHealth Sciences Research CommonsDermatology Faculty PublicationsDermatology1-1-2017Review of Applications of Microneedling inDermatology.Christopher IriarteGeorge Washington UniversityOlabola AwosikaGeorge Washington UniversityMonica Rengifo-PardoGeorge Washington UniversityAlison EhrlichGeorge Washington UniversityFollow this and additional works at: http://hsrc.himmelfarb.gwu.edu/smhs derm facpubsPart of the Dermatology Commons, and the Skin and Connective Tissue Diseases CommonsAPA CitationIriarte, C., Awosika, O., Rengifo-Pardo, M., & Ehrlich, A. (2017). Review of Applications of Microneedling in Dermatology. ClinicalCosmetic and Investigational Dermatology, 10 (). http://dx.doi.org/10.2147/CCID.S142450This Journal Article is brought to you for free and open access by the Dermatology at Health Sciences Research Commons. It has been accepted forinclusion in Dermatology Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, pleasecontact hsrc@gwu.edu.
Clinical, Cosmetic and Investigational DermatologyDovepressopen access to scientific and medical researchREVIEWOpen Access Full Text ArticleReview of applications of microneedlingin dermatologyThis article was published in the following Dove Press journal:Clinical, Cosmetic and Investigational Dermatology8 August 2017Number of times this article has been viewedChristopher Iriarte 1Olabola Awosika 2Monica Rengifo-Pardo 1,2Alison Ehrlich 1,21George Washington UniversitySchool of Medicine and HealthSciences, Washington, DC, USA;2Department of Dermatology, TheGeorge Washington Medical FacultyAssociates, Washington, DC, USAAbstract: Microneedling (MN) is a novel therapeutic modality in dermatology. Throughphysical trauma from needle penetration, MN induces a wound healing cascade with minimaldamage to the epidermis. This allows for enhancement in the absorption of mainstay topicaltherapies across the thick stratum corneum. MN has become increasingly utilized over the lastseveral years as it is a relatively simple procedure that is cost-effective, well tolerated, and offersboth cosmetic and therapeutic benefits. The ability to treat localized areas of disease has led tonumerous studies gauging its potential in focal diseases of inflammation, dyschromia, and photodamage. This review discusses the principles and evidence behind the expanding applicationsof MN. It has shown promising results as an adjuvant therapy for enhanced drug delivery in thetreatment of atrophic scars, alopecia, actinic keratoses, and disorders of pigmentation such asmelasma. The efficacy in treatment of vitiligo remains limited. Overall, the procedure has fewadverse sequelae compared to other therapies, is highly efficacious, and is a viable resurfacingoption for skin of color. Future research is needed to determine the frequency, interval, andspecific device settings that foster optimal results. Additionally, large controlled trials are neededto shed light on the utility of MN as an evidence-based regimen for the treatment of variousdermatologic conditions.Keywords: microneedling, scars, acne, alopecia, hyperpigmentation, actinic keratosisIntroductionCorrespondence: Alison EhrlichDepartment of Dermatology, TheGeorge Washington University MedicalFaculty Associates, 2150 PennsylvaniaAvenue NW, Suite 2B-430, Washington,DC 20037, USATel 1 202 741 2625Email aehrlich@mfa.gwu.eduMicroneedling (MN), also known as collagen induction therapy, is a process involvingrepetitive puncturing of the skin with sterilized microneedles. Its original conceptioncan be traced back to 1995, when Orentreich and Orentreich developed the concept of“subcision”, or using hypodermic needles to induce wound healing in depressed cutaneousscars.1 In 2006, Dr. Desmond Fernandes developed the first MN product which became themodern-day Dermaroller (Dermaroller Deutschland GmbH, Wolfenbuettel, Germany).2MN offers a relatively low cost and minimally invasive tool for the treatment ofmultiple cosmetic and dermatologic conditions.3 The basis of MN relies on physicaltrauma. It has been proposed that the trauma generated by needle penetration in theskin induces regeneration of the dermis.4 The needles penetrate the stratum corneumand create small holes known as micro-conduits with minimal damage to the epidermis.This sequentially leads to the generation of growth factors which stimulate the production of collagen and elastin in the papillary layer of the dermis.3 The natural woundhealing cascade is induced as platelets and neutrophils are recruited to release growthfactors such as TGF-alpha, TGF-beta, and platelet-derived growth factor (PDGF).2This ultimately results in the deposition of collagen by fibroblasts.289submit your manuscript www.dovepress.comClinical, Cosmetic and Investigational Dermatology 2017:10 289–298Dovepress 2017 Iriarte et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the workyou hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. Forpermission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms i.org/10.2147/CCID.S142450
DovepressIriarte et alA variety of MN products have been developed to treatscarring and wrinkles, enable skin rejuvenation, and improveskin appearance.5 Clinical trials over the last several yearshave shed light on the applications of MN beyond cosmeticindications, including actinic keratoses (AK), disorders ofpigmentation, hyperhidrosis, and striae.6 Additionally, therole of MN in the treatment of hair pathology has become arecent field of focus as it is thought to stimulate stem cells inthe dermal papilla, increase blood flow to hair follicles, andrecruit growth factors and signaling pathways which inducehair restoration.7 MN is also postulated to induce normalwound healing, specifically by breaking collagen strands inthe superficial dermis and inducing collagen synthesis immediately under the epidermis.8 This mechanism is the guidingprinciple behind the application of MN in the treatment ofscars of various etiologies.This review of the literature is focused on exploring theexpanding indications of MN. In addition, this review willhighlight the efficacy and adverse effect prolife of MN incomparison with more common treatment modalities usedfor various indications in dermatology.MethodsThe studies selected for this review were gathered by searching the PubMed, MEDLINE, Cochrane databases, and electronic journals of dermatology. The search terms used forthis review included “microneedling”, “collagen induction”,“reviews”, and “trials”. Only articles published in Englishwere considered for inclusion in this review. Articles wereobtained in all circumstances and references were checked foradditional information when considered applicable. Availablestudies involving human subjects were included in the review.Additionally, only studies regarding manual MN techniqueswere considered for inclusion. Priority was given to controlled clinical trials, both prospective and retrospective, witha minimum of ten patients as the sample size. Uncontrolledclinical trials were included so long as a statement was maderegarding the study’s experimental design and limitations.Smaller case series with less than ten patients were includedif they were the only available data for specific indicationssuch as alopecia areata (AA) or verruca plantaris.Types of MNCurrently, there are many mechanical MN devices registeredwith the US Food and Drug Administration (FDA), with themajority being a variation of either the Dermaroller or theDermapen (Dermapen, Salt Lake City, UT, USA). The Dermaroller is a hand-held device with a cylindrical roller of 24290submit your manuscript www.dovepress.comDovepresscircular arrays.6,9 Each array is equipped with eight medicalgrade solid steel microneedles, totaling to 192 needles on oneDermaroller device.6,9 The device is used in a multi-directionalfashion (vertically, horizontally, and diagonally) directly overthe skin. Medical models include the CIT 8 and MF 8 ,which consist of needle heights of 500 µm and 1,500 µm,respectively.6 Various models have also been developed foruse in the home, including the Beauty Mouse (DermarollerDeutschland GmbH) which consists of 480 needles to use onlarger skin surfaces.5 The Dermapen is a spring-loaded MNdevice which acts as an electrically powered pen, deliveringstamp-like motions across the skin.10 Several commercialvariations of this device exist based on the same principles.Other devices use additional technology to build uponthe applications of mechanical MN. Indications for thesenewer modalities include superficial scars, hyperhidrosis, andwrinkles.6 These MN modalities include fractional radiofrequency microneedling (FRFM), DermaFrac (Genesis Biosystems, Lewisville, TX, USA), light emitting diode (LED)MN devices, and MN delivery systems.6 FRFM is differentiated from manual MN due to the method of each insulatedneedle releasing a radiofrequency current from the needletip producing changes in dermal structural components.6,11In DermaFrac treatment, MN is combined with microdermabrasion, LED light, and simultaneous serum infusion intothe dermis.6 LED MN rollers combine solely LED light andMN. MN delivery systems are a method of transdermal drugadministration in which solid microneedles pierce the skinfollowed by topical drug application. Alternatively, drugscan be delivered directly into the dermis through hollowneedles.12 Of note, in 2011, Fluzone Intradermal influenzavirus vaccine (Sanofi Pasteur, Swiftwater, PA, USA) becamethe first and only microneedle-based product approved by theFDA for this process.13,14 It is recommended that the use ofMN to enhance absorption of topical agents be performedwith caution as non-sterilized drugs may contain particlesthat penetrate the skin to varying degrees and contribute tofurther complications, such as infection due to the permeationof pathogenic microbes.12Applications of MNThe sections that follow will provide an overview of theclinical trials in dermatology that have been performedwith manual MN, as well as several case series. Specificinformation regarding study design, treatment intervals,MN devices used, and comparative efficacy can be found inthe accompanying tables. These tables summarize the majorstudies covered in this review for each respective indicationClinical, Cosmetic and Investigational Dermatology 2017:10
Dovepressthat follows. Each section concludes with our summary ofthe current state of the literature and future areas for researchspecific to each indication.ScarsSeveral studies show efficacy of MN for scar treatment(Table 1). In a pilot study, El-Domyati et al quantified thehistological changes induced by MN in ten patients withatrophic facial scars from acne.15 Skin biopsies were obtainedat baseline and post-treatment with Dermaroller. Therewas a statistically significant increase in the production ofcollagen types I, III, and VII and a decrease in total elastinby the end of treatment (p 0.05). All patients reportedmild pain and edema at the treatment site which resolvedwithin 24 hours. Otherwise, no adverse effects were noted.Patients collectively reported a 51%–60% improvement inscar appearance, 40%–50% improvement in skin texture,and 80%–85% overall satisfaction (p 0.001) following sixtreatment sessions over the course of 3 months.15In a cohort study, Majid relied on clinical outcomes ratherthan histologic changes to assess improvement of atrophicfacial scars in response to MN therapy.16 Thirty-seven patientswere offered Dermaroller treatments and followed over thecourse of 2 months. Over 80% of the patients assessed theirresponse to treatment as “excellent” on a 10-point scale.Of the patients who completed the study, 94.4% graded thereduction in the severity of their scars by at least one objective grade. No adverse effects were noted.16A clinical trial by Garg and Baveja assessed the efficacyof combination therapy using subcision, MN, and 15% trichloroacetic acid peel in the management of 50 patients withatrophic acne vulgaris scars.17 The patients were treated for atotal of six sessions with scar grading done at baseline and 1month after treatment. Complete remission was demonstratedin all patients with Grade 2 scars and 22.7% of patients withGrade 3 scars. Additionally, of the 16 patients with Grade 4scars at baseline, ten patients improved to Grade 2 and theremaining six improved to Grade 3. Overall, 100% of patientshad objective improvement in scars by at least 1 grade.Adverse events other than transient erythema and edemaincluded acne eruptions, post-inflammatory hyperpigmentation (PIH) resolving after 5 months of topical treatment (withcombination of tretinoin, hydroquinone, and mometasone),and cervical lymphadenopathy lasting 3 weeks.17Several studies have also compared the efficacy of laserand MN treatments. Cachafeiro et al compared 1,340 nm nonablative fractional erbium laser and Dr. Roller (VydenceMedical, São Carlos, São Paulo, Brazil) for the treatment ofClinical, Cosmetic and Investigational Dermatology 2017:10Microneedling: review of the literature46 patients with facial atrophic acne scars.18 These patientswere randomized to one of the two groups and received threetreatment sessions monthly regardless of assignment. Bothgroups demonstrated improvement at 2 and 6 months posttreatment, with no statistically significant difference betweenthem (p 0.264). While efficacy was similar, the adverseevent profile varied. The MN group experienced erythema foran average of 1 day compared to the laser group, for whichthe erythema lasted an average of 3 days. Additionally, 13.6%of the patients in the laser group experienced PIH while noneof the patients in the MN group did.18Another emerging field of study in MN is its applicabilityin the treatment of scars in various ethnic groups. One clinicaltrial by Dogra et al evaluated the utility of MN for treatingatrophic acne scars in Asian populations.19 On an objective scale of 18 points, patients’ assessments of their scarsdecreased from 11.73 to 6.5 following five MN treatments,indicating significant improvement. In a study with patientsof darker pigmented skin, the use of MN combined with glycolic acid peels for the treatment of acne scars was assessedin 30 Indian patients with atrophic box type and rolling scarswith PIH.20 Patients were assigned to receive treatment withMN only or with MN and 35% glycolic acid peels. Therewas significant improvement in skin texture, scarring, anda reduction in PIH in the group treated with the combinedapproach when compared to MN alone (p 0.001).20MN has also been used to enhance treatment of hypertrophic surgical scars by increasing drug delivery of topicalagents to the dermis.21 Aust et al demonstrated MN to bean effective alternative for burn patients with hypertrophicscars.22 In this study, 16 patients with post-burn scarringwere treated with MN after 4 weeks of preparation withtopical vitamin A and C to maximize collagen production.Each patient reported satisfaction with scar appearance onan objective visual analog scale (VAS) from 1 to 10, with10 indicating the most satisfaction. Prior to treatment, theaverage VAS score was 4.5. This score increased to 8.5 following one to four sessions of MN treatment with continuedapplication of topical vitamin A and C twice daily. Histologicanalysis of 3 mm punch biopsies at 1 year demonstrated anincrease in collagen and elastin deposition both quantitatively and qualitatively using van Gieson and hematoxylinand eosin stains.Studies with various-sized MN devices that evaluate thefrequency and interval between treatments for optimal effects,would be an appropriate next step in further elaborating on theefficacy of MN. Many of the aforementioned studies demonstrated that MN had comparable efficacy to laser treatmentssubmit your manuscript www.dovepress.comDovepress291
292submit your manuscript % TCA peel andsubcision /DermarollerNFEL 1340 nm /Dr. RollerDermaroller35% glycolic acidpeels /Dermaroller MF8Topical vitamins Aand C /- MedicalRoll-CITEl-Domyatiet al, 201515Majid, 200916Garg andBajeva, 201417Dogra et al,201419Sharad,2011201.0 mm1.5 mm1.5 mm2.0 mm1.5 mm1.5 mm1.5 mmNeedledepthAtrophicacne scarswith PIHHypertrophicburn scarsAtrophicacne scarsAtrophicacne scarsAtrophicacne scarsAtrophicfacial scarsAtrophicacne scarsType ofscarUncontrolled,prospective cohortstudyProspective RCTUncontrolled,prospective studyUncontrolled,prospective clinicaltrialUncontrolled,prospective clinicaltrialEvaluator-blinded,prospective RCTProspective clinicalstudyStudy design16303646503710No ofpatients(N)1–4 (4 weeks)5 (6 weeks)5 (4 weeks)3 (4 weeks)6 (2 weeks)4 (4 weeks)6 (2 weeks)No of sessions(interval)Increase in the mean of collagen types I, III, and VII, as well as newlysynthesized collagen at the end of treatment (p 0.05). There was a decreasein total elastin production. Patients reported an 80%-85% overall satisfaction(p 0.01).Per Goodman and Baron’s42 facial scar scale, 94% of patients had a reductionin scar severity by at least 1 grade. Over 80% of patients assessed theirresponse to treatment as “excellent”.Per Goodman and Baron’s42 facial scar scale, 63% with Grade 4 improved toGrade 2 and 38% improved to Grade 3. 23% with Grade 3 had full remissionand 68% improved to Grade 2. 100% of Grade 2 had full remission.Both groups demonstrated improvement in the degree of their acne scars,with no statistically significant difference found between the groups(p 0.264).Significant decrease in mean acne scar assessment score from 11.73 atbaseline to 6.5 after 5 sessions (p 0.05). Photographic improvement of 50%75% in majority of patients.There was 31% improvement in the MN alone group vs. 62% improvementin the MN with glycolic acid peels group in regards to skin texture and scarappearance (p 0.001).Reported satisfaction with scar on VAS increased from 4.5 to 8.5 followingtreatment. Histologic analysis at 1 year showed increase in collagen andelastin deposition.ResultsNotes: Dermaroller and Dermaroller MF8 ; Dermaroller Deutschland GmbH, Wolfenbuettel, Germany. Dr. Roller ; Vydence Medical, São Carlos, São Paulo, Brazil. Medical Roll-CIT ; Vivida, Cape Town, South Africa.Abbreviations: MN, microneedling; N, sample size; TCA, trichloroacetic acid; NFEL, non-ablative fractional erbium laser; RCT, randomized controlled trial; PIH, post-inflammatory hyperpigmentation; VAS, visual analog scale (gradedfrom 1 to 10).Aust et al,201022Cachafeiroet al, 201618Adjunctivetherapy /- MNtherapyReferenceTable 1 Scars treated with microneedling therapyIriarte et alDovepressClinical, Cosmetic and Investigational Dermatology 2017:10
DovepressMicroneedling: review of the literaturefor atrophic facial scars. However, MN is generally bettertolerated with fewer long-term adverse sequelae.23 Scar typeappears to be a factor affecting clinical response to MN, asicepick scars and deep-seated atrophic scars responded lessideally to treatment.15AlopeciaMN has been proposed as a mechanism for adjuvant hairregrowth in alopecia. The efficacy of MN in both androgenetic alopecia (AGA) and AA has been highlighted over thelast 5 years (Table 2).AGADhurat et al found that combination treatment of MN withminoxidil was statistically superior to minoxidil alone in thetreatment of 100 male patients with AGA.24 Over 12 weeks,Dermaroller treatment combined with 5% minoxidil lotionwas administered to half of the participants, with 80%showing moderately or greatly increased hair regrowth perthe investigators. Of the same subset, 82% of the patientsreported subjective improvement greater than 50% in theirhair growth. In the arm receiving 5% minoxidil alone, only4.5% of patients reported greater than 50% improvement. Bythe end of the study, mean change in hair count was significantly greater for the MN group (91.4 vs. 22.2, p 0.039).Additionally, the initiation of new hair growth was firstnoticeable at 6 weeks in the MN group compared to 10 weeksin the minoxidil alone group. No adverse effects were notedby any of the participants.24Dhurat and Mathapati then published a follow-up caseseries of four men with AGA unresponsive to conventionaltreatments. Combination therapy was administered to participants with their prior treatment regimen (either topicalminoxidil or oral finasteride) and Dermaroller over a courseof 6 months.25 All four patients had moderately or greatlyincreased hair regrowth and reported subjective increases inhair thickness after 1 month of treatment.25AAMN has been proposed as a viable alternative to conventionaltreatment for AA as well. The mainstay of therapy for AAis currently intralesional corticosteroids, such as kenalog(ILK). However, the collagen induction offered by MN isthought to counter steroid-induced atrophy as well as causeless pain than injection.26Chandrashekar et al analyzed outcomes from treatingresistant AA with MN and topical corticosteroids.26 Twoadult patients with AA recalcitrant to ILK, topical steroids,and minoxidil 5% lotion received topical triamcinoloneapplied before and after Dermaroller. Both patients gradedTable 2 Alopecia treated with microneedling therapyReferenceAdjunctivetherapy /MN therapyNeedledepthType ofalopeciaStudy designNo ofpatients(N)No ofsessions(interval)ResultsDhurat et al,2013245% topicalminoxidil /Dermaroller1.5 mmAGAProspective,evaluator-blindedRCT10012 (1 week)Dhurat andMathapati,2015255% topicalminoxidil andoral finasteride /- Dermaroller1.5 mmAGACase series44 (1 week) then11 (2 weeks)Chandrashekaret al, 2014260.1% topical TAC /- Dermaroller1.5 mmAACase series23 (3 weeks)Mean hair counts weresignificantly greater in MN minoxidil group comparedto minoxidil alone group(91.4 vs. 22.2, p 0.039). 82%in combination group reportedgreater than 50% improvementvs. 4.5% in minoxidil group.100% showed 2 or 3 responseson a 7-point standardized scalefor hair growth. Findings weresustained at final follow-up. 75%had subjective improvement inhair growth 75%.100% graded hair regrowth as“excellent” at 3-week follow-upwith no recurrence of AA at12 weeks.Notes: Dermaroller ; Dermaroller Deutschland GmbH, Wolfenbuettel, Germany.Abbreviations: MN, microneedling; N, sample size; AGA, androgenetic alopecia; RCT, randomized controlled trial; TAC, triamcinolone; AA, alopecia areata.Clinical, Cosmetic and Investigational Dermatology 2017:10submit your manuscript www.dovepress.comDovepress293
DovepressIriarte et alhair regrowth as “excellent” and had no recurrence at3-month follow-up. The ability to assess for commonadverse effects of steroid treatment such as atrophy, scarring, and increased susceptibility to infection were limitedin this study.While these clinical studies show promising data for theefficacy of MN in the treatment of alopecia, these resultsare limited by relatively small sample sizes. Additionally, itis unclear if similar results are reproducible in women withhair disorders. Further investigations of combination therapywith minoxidil and finasteride, including MN frequency,needle size, and duration of treatment are needed to see ifthese results are reproducible in both genders and sustainedover longer periods of time.Pigmentary disordersSeveral studies have proposed MN as an alternative to conventional treatment in disorders of pigmentation affectingdarker skin types, including melasma, vitiligo, and periorbitalhyperpigmentation (Table 3).MelasmaThe enhanced transdermal drug absorption seen with MN hasachieved better results than skin lightening agents alone inthe treatment of melasma.27–29 Budamakuntla et al observedenhanced results of MN followed by topical tranexamic acidin comparison to tranexamic acid microinjections in treating moderate to severe melasma in 60 patients.30 After threetreatment sessions (at 0, 4, and 8 weeks), the patients werefollowed for 3 months. There was 35.72% improvement in themean Melasma Area and Severity Index (MASI) score in themicroinjection group (p 0.01) compared to 44.41% in theMN group (p 0.001). Notably, only 26% of patients in themicroinjection group achieved 50% improvement comparedto 41% in the MN group. Neither group experienced majorside effects, but some reported mild discomfort, burningsensation, and erythema.30In a pilot study, the use of depigmentation serum containing 4-butylresorcinol and sophora-alpha (prenylatedflavonoids from the roots of Sophora flavescens) alone wascompared to the combination treatment of depigmentationserum and MN (MN serum) in 20 female patients (Fitzpatrick Skin Type III–IV) with melasma.27 In the MN serumgroup, baseline mean MASI score decreased by 9.9 points(p 0.001) compared to a 7.1 point decrease (p 0.05) inthe serum only group 2 months post-treatment. Results wereconfirmed by the significant increase in brightness of patients294submit your manuscript www.dovepress.comDovepressreceiving combination treatment in comparison to the groupreceiving serum alone (17.4% vs. 11.2%; p 0.05).27MN combination therapy also has favorable results inmelasma when combined with daily sunscreen use. In aretrospective analysis of 22 cases of recalcitrant melasma(unresponsive to topical bleaches and sunscreen), MN wasadministered followed by night time application of a depigmentation formula (0.05% tretinoin 4% hydroquinone 1% fluocinonide acetonide) and daily tinted sunscreen (SPF60) 24 hours after initial skin needling.31 The procedure wasrepeated 30 days after the first treatment. All 22 patientsreported satisfaction with results at 2 month follow-up. Photographic analysis at 24-month follow-up in eleven patientsdemonstrated continued maintenance of skin lighteningobserved at the 2-month visit.31VitiligoThe efficacy of MN in combination treatment for vitiligoremains unclear. Stanimirovic et al investigated repigmentation of patients with resistant bilateral symmetrical vitiligoby comparing treatment with narrowband ultraviolet B andtopical 0.005% latanoprost solution with and without Dermaroller.32 Seventeen patients in each group had repigmentation(37.8% of treated lesions) and only 8.8% of repigmentinglesions had greater than 50% repigmentation. However, therewas no statistically significant difference in repigmentationbetween groups.32Periorbital melanosisMN therapy has been successful in the treatment of periorbital hyperpigmentation. One male patient demonstrated75%–90% improvement with DermaFrac treatment (combination of MN and active ingredients, including kojic acidor anti-aging serum containing myristoyl pentapeptide 17[SymPeptide], acetyl octapeptide-3 [SNAP 8], palmitoylpentapeptide-4 [Matrixyl], acetyl hexapeptide-8 [Argirilene]and tripeptide [Syn-ake]) after 12 sessions.33 The patient alsoreported 7 out of 10 improvement on the Patient’s GlobalAssessment scale in his pigmentation.Kontochristopoulos et al also explored the use of MNin periorbital hyperpigmentation by treating 13 femalepatients with MN followed by 10% trichloroacetic acidpeels.34 Almost all patients (92.3%) demonstrated significant improvement (“fair or better”) according to patientglobal assessments. Transient side effects includingmild discomfort, edema, and erythema were commonlyobserved.34Clinical, Cosmetic and Investigational Dermatology 2017:10
CIT 8TM:0.5 mmDermaroller C8:0.13 mm1.5 mm2.0 mm1.5 mm0.25 mm0–2.5 mmDepigmentation serum* /- DermarollerCIT 8 in office andDermaroller C8 at homeTA /- DermarollerMS4Depigmentationformula** /Dr. RollerNB-UVB latanoprost /DermarollerAnti-aging serum*** /DermaFracTCA peels /Automatic MNFabbrocini et al,201127Lima, 201531Stanimirovic et al,201632Sahni and Kassir,201333Kontochristopouloset al, 201634Clinical, Cosmetic and Investigational Dermatology 2017:10Periorbital melanosisPeriorbital melanosisVitiligoMelasmaModerate to severemelasmaMelasmaDisorder ofpigmentationUncontrolled,prospective studyCase reportSplit-body,prospectivecontrolled e,controlled trialStudy design13125226020No ofpatients (N)11 session of MN latanoprost,9 sessions of NBUVB (3 times perweek)12 (2 weeks)2 (4 weeks)3 (4 weeks)1 in office, 60 athome (daily)No of sessions(interval)Per physician global assessment, there was 50%75% improvement after 4 sittings and 75%-90%improvement after 12 sittings.92.3% had fair, good, or excellent response onphysician and patient global assessments. Therewas no recurrence at 4 months.36% improvement in MASI score in TA alone vs.44% improvement in MASI score in TA MN.More patients in TA MN had greater than 50%improvement than TA alone (41% vs. 26%).100% demonstrated “good to very good”results and reported subjective satisfactionwith treatment. 50% of patients maintained skinlightening at 1-year follow-up.Equal repigmentation observed in pairedexperimental and control lesions in 77% oflesions.Mean MASI score improvement of 9.9 in serum MN (p 0.001) vs. improvement from 7.1 inserum alone (p 0.05).ResultsNotes: *Depigmentation serum: 4-butylresorcinol and sophora-alpha (prenylated flavonoids from the roots of Sophora flavescens). **Depigmentation formula: 0.05% tretinoin, 4% hydroquinone, and 1% fluocinonide and sunscreen SPF60. ***Anti-aging serum: myristoyl pentapeptide 17 (SymPeptide), acetyl octapeptide-3 (SNAP 8), palmitoyl pentapeptide-4 (Matrixyl), acetyl hexapeptide-8 (Argirilene) and tripeptide (Syn-ake
This review of the literature is focused on exploring the expanding indications of MN. In addition, this review will highlight the efficacy and adverse effect prolife of MN in comparison with more common treatment modalities used for various indications in dermatology. Methods The studies selected
SkinPen Precision is an automated, non-surgical microneedling device designed for use by licensed healthcare practitioners or individuals directed by practitioners. The device incorporates a sterile microneedle cartridge and BioSheath for single use only. SkinPen Precision Handpiece Model #100 SkinPen Precision Charger Base Model #101
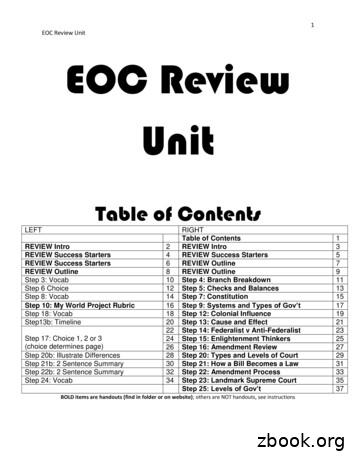
1 EOC Review Unit EOC Review Unit Table of Contents LEFT RIGHT Table of Contents 1 REVIEW Intro 2 REVIEW Intro 3 REVIEW Success Starters 4 REVIEW Success Starters 5 REVIEW Success Starters 6 REVIEW Outline 7 REVIEW Outline 8 REVIEW Outline 9 Step 3: Vocab 10 Step 4: Branch Breakdown 11 Step 6 Choice 12 Step 5: Checks and Balances 13 Step 8: Vocab 14 Step 7: Constitution 15
the public–private partnership law review the real estate law review the real estate m&a and private equity review the renewable energy law review the restructuring review the securities litigation review the shareholder rights and activism review the shipping law review the sports law review the tax disputes and litigation review
the product regulation and liability review the shipping law review the acquisition and leveraged finance review the privacy, data protection and cybersecurity law review the public-private partnership law review the transport finance law review the securities litigation review the lending and secured finance review the international trade law .
2. Left 4 Dead 2 Review 3. Bayonetta Review 4. New Super Mario Bros Wii Review 5. F1 2009 Review 6. Gyromancer Review 7. King's Bounty: Armored Princess Review 8. Crane Simulator 2009 Review 9. Resident Evil: The Darkside Chronicles Review 10. Jambo! Safari Review List based on traffic for Eurogamer articles dated 17th - 23rd November.
Keywords: review genres, academic review genres, review article, critical evaluative review, mixed-mode review, bibliographic review 1. Introduction Review genres are normally written texts or part texts that can provide suitable places for expression of personal ideas, attitudes, and evaluations.
Products Selected for Review Krill Oil and Algal Oil Supplements Also Tested for Omega-3s Alphabetical list of fish oil, krill oil, and algal oil supplement brands in report Advocare review Natural Factors review Solgar review CardioStat (Amerifit) review Nature Made review Source Naturals review Carlson
Advanced Engineering Mathematics 1. First-order ODEs 25 Problems of Section 1.3. The differential equation becomes Advanced Engineering Mathematics 1. First-order ODEs 26 1.4 Exact differential equations Now we want to consider a DE as That is, M(x,y)dx N(x,y)dy 0. The solving principle can be