Orthopaedic Insights - Cleveland Clinic
Fall 2012Orthopaedic InsightsA Physician Newsletter fromthe Department of Orthopaedic SurgeryIn This Issue:3 Combining 3D10 Patient-Specific20 Dual QuestionnaireInstrumentation in TKRfor Adolescents with LegProblemsPlanning Software withTransfer Device for ImplantPlacement12 3D Templating Helps6 iPad App TakesHospital-Acquired IllnessAfter Joint Arthroplasty25 Cleveland Clinic Updates16 The High Stakes26 Residency Update 2012Guesswork Outof Concussion Care8 Diabetic AnkleFractures: AggressiveTreatment NeededCorrect Radioulnar Defects14 Stratifying Risk ofof Pelvic Ring Injuries18 Partial ResurfacingImplant for HumeralBone Loss22 Vigilant Managementof EnchondromaThe Netter Collection
2Orthopaedic InsightsFor referrals, please call 216.445.0096 or 800.223.2273, ext.50096Dear Colleague,Welcome to the Fall 2012 issue of Orthopaedic Insights from Cleveland Clinic’s Departmentof Orthopaedic Surgery. We bring you this newsletter twice yearly to update you on clinicaland research initiatives we hope will spark interactions about how we can jointly advanceorthopaedic care for patients around the nation and beyond.U.S. News &World ReportCleveland Clinic’s OrthopaedicProgram is ranked No. 3 inthe nation in U.S. News &World Report’s “America’sBest Hospitals” survey — thetop-ranked program in Ohio.Advancing care in that way involves a certain measure of leadership, and I am pleased thatthe contributions to this issue demonstrate leadership across a wide swath of orthopaedicpractice. On pages 3 and 12 we spotlight some leading-edge work we are doing with threedimensional preoperative planning software — in one case in conjunction with a transferdevice to improve glenoid guide pin placement, and in the other case to enhance the precision of radioulnar deformity correction. On page 6 we share Cleveland Clinic’s pioneering useof iPad technology to change the trajectory of concussion care in sports medicine — alongwith our hopes to deploy the technology for broader use across the country. And on page 25we announce our unique collaboration with Elsevier to update the Musculoskeletal Systemvolume of the iconic Netter Collection of Medical Illustrations.These are just a few of the examples of diverse leadership in research, education and clinicalpractice you will find in these pages. I believe this ethic of leadership was an important factorin Cleveland Clinic’s ranking as one of the top 3 orthopaedic programs in the nation in U.S.News & World Report’s “America’s Best Hospitals” survey in 2012. This recognition is anhonor we remain committed to living up to in the year ahead.While on the topic of leadership, I am proud to recognize two of our department membersfor recently taking on crucial leadership roles within the Cleveland Clinic health system. In2011, Brian Donley, MD, was appointed President of Cleveland Clinic’s Lutheran Hospital;and earlier this year Mark Froimson, MD, was named President of Cleveland Clinic’s EuclidHospital. Although our department has a bit less of their time for their clinical expertise(in foot and ankle reconstruction in Dr. Donley’s case, and in arthroplasty in Dr. Froimson’scase), our loss is more than made up for by our health system’s tremendous gain fromtheir demonstrated leadership and vision.My colleagues and I are mindful that an essential component of leadership is good listening,so I invite you to share with us your comments, questions and ideas in response to anythingyou see here. Look for our authors’ contact information at the end of their articles, and feelfree to contact me with your thoughts as well. Enjoy the issue.Richard D. Parker, MDChairman, Department of Orthopaedic SurgeryProfessor, Cleveland Clinic Lerner College of Medicine216.444.2992 parkerr@ccf.org
Visit clevelandclinic.org/orthoFALL2012Combining 3D Planning Software with Use of aTransfer Device to Improve Glenoid Guide Pin PositioningBy Joseph Iannotti, MD, PhD; Justin Baker, PhD; Eric Rodriguez, BS; John Brems, MD; Eric Ricchetti, MD;Mena Miseha, MD; and Jason Bryan, MSInaccurate or improperly placed implants shorten implantsurvival and decrease performance, putting patients at riskfor suboptimal outcomes. Technologies such as patientspecific instruments and computer-guided surgery seek toimprove the accuracy of implant placement.We recently tested this approach for surgical navigationto significantly improve glenoid implant placement andcompared the results with standard-of-care surgical methodsin pathologic patient bone models. We share an overviewof our results here.At Cleveland Clinic, we have developed an alternativeapproach to these two technologies that incorporatesthe information derived from a three-dimensional (3D),software-generated preoperative plan for arthroplastyprocedures into a patient-specific bone model that thencontains the information needed to execute the surgicalplan. In our unique approach, a reusable and adjustabletool is placed over the guide wire and the anatomicmodel to record the orientation from the software andthen transfer it to the surgical site (Figure 1).OUR STUDY DESIGNWe tested this new technology using a preclinical surgicalmodel that we have validated to reflect clinically relevantpathology and surgical exposure. Each of nine pathologicscapula models was shrouded to allow exposure of only thatportion of the glenoid typically seen at the time of surgery.Three surgeons of varying surgical experience in shoulderarthroplasty placed a guide pin in each of the specimensusing one of three methods:continued on next pageMark leg contact point on patientPrint model from softwareand set device on model.Drive pin, remove device, compare trajectoryTransfer to patientFigure 1. Overview of how the guide pinlocation and trajectory information fromthe 3D preoperative planning software istransferred to the patient using the transferdevice. The information is output fromthe software by printing a 3D model of thepatient’s bone. The transfer device is seton the model and loaded with the correctleg lengths, after which it is ready fortransferring the exact location and trajectoryfrom the model to the patient/sawbone.3
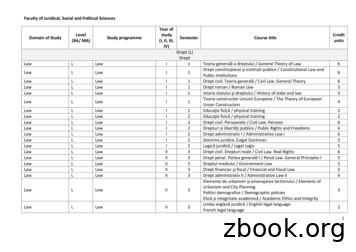
4Orthopaedic InsightsFor referrals, please call 216.445.0096 or 800.223.2273, ext.50096This preclinical trial provides evidence andjustification for a randomized clinical trial ofthis new technology, which we have begun. Standard-of-care instrumentation alone(standard method [SM]) Standard-of-care instrumentation plus use of the3D preoperative planning software (SM 3D) Use of the software-smart surrogate-adjustableinstrument technology (experimental method [EM])Additionally, compared with the SM approach, the SM 3Dapproach was associated with a 70 percent lower risk of deviation of version angle by more than 10 (P .005) and with anaverage improvement in inclination angle by 3.3 ( 1.3 ) (P .013). There was also an improvement of 0.4 mm ( 0.2 mm) inimplant placement with SM 3D relative to SM alone (P .042).All scapula models underwent CT scanning after pinplacement, and the results are reported as the deviationCompared with the SM approach, the software-smartsurrogate-adjustable instrument technology (EM; n 89)improved guide pin version by 8.2 ( 0.9 ) (P .001),improved inclination by 11.4 ( 1.2 ) (P .001), and improvedimplant placement distance by 1.7 mm ( 0.2 mm) (P .001).Moreover, the EM approach significantly increased theaccuracy of implant placement compared with the SM 3Dmethod in terms of version, inclination and distance(P .001) (Figure 2).(in millimeters or degrees) from the desired pin position.RESULTS: EXPERIMENTAL APPROACHOUTPERFORMS BOTH STANDARD METHODSCompared with standard surgical care alone (SM; n 54),standard surgical care plus the 3D planning software(SM 3D; n 54) improved guide pin version deviation by anaverage of 4.5 ( 1 standard deviation) (P .001).The table details the average absolute deviation fromimplant placement plan for each of the three methods.Table. Average Absolute Deviation from Plan for Implant PlacementVersion*Inclination*Distance*Experimental method (EM)(software-smart surrogate-adjustable instrument technology)3.1 2.6 2.8 2.1 1.2 0.7 mmStandard method plus 3D planning (SM 3D)6.7 5.9 9.3 5.6 2.4 1.3 mm11.1 7.3 10.7 5.8 2.9 1.6 mmStandard method (SM)*Mean standard deviation
Visit clevelandclinic.org/orthoFALL2012Figure 2. Scatter plots showing (left) the deviation in version and inclination of the actual implanted pin from the planned pin location with eachof the three methods, and (right) the deviation in distance between the various methods and the planned pin location. Note that in each panel theexperimental method (EM) cluster is tighter and more centered around no deviation.CONCLUSIONS AND NEXT STEPSOur novel concept for the transfer of preoperative data toa surgical site using software-smart surrogate-adjustableinstrumentation showed substantial improvement in theaccuracy of glenoid guide pin placement compared with standard methods. This surgical method can be applied to otherarthroplasty applications. Our preclinical study provides abasis for performing a clinical trial in shoulder arthroplastyto determine the ability of this novel technology to improvesurgical outcomes. The development of this new technology,together with the data from this preclinical trial, providesevidence and justification for a randomized clinical trial.We have started this clinical study.This method of surgical planning and guide pin placementis applicable to other surgical procedures and anatomic sites.ABOUT THE AUTHORSDr. Iannotti is Chairman of Cleveland Clinic’s Orthopaedic& Rheumatologic Institute and a member of the Departmentsof Orthopaedic Surgery and Biomedical Engineering. He canbe contacted at iannotj@ccf.org. Dr. Brems and Dr. Ricchettiare surgeons in the Department of Orthopaedic Surgery, andMr. Rodriguez is a research associate in the Department ofOrthopaedic Surgery.Dr. Baker is a product development engineer at CustomOrthopaedic Solutions, Cleveland, and was formerly apostdoctoral research fellow at Cleveland Clinic.Dr. Miseha, formerly a resident in orthopaedic surgery atCleveland Clinic, is currently a fellow on the shoulder andelbow service at Harvard School of Medicine.Mr. Bryan is an employee of ImageIQ, Cleveland, and wasformerly a member of the research staff at Cleveland Clinic’sLerner Research Institute.5
6Orthopaedic InsightsFor referrals, please call 216.445.0096 or 800.223.2273, ext.50096Cleveland Clinic iPad App Takes the GuessworkOut of Sports-Related Concussion AssessmentBy Jay L. Alberts, PhD, and Richard Figler, MDThe management of concussion in young athletes toooften follows a scenario like this:An athlete sustains a blow to the head in a Friday nightgame. He’s taken out of the game but “shakes it off” withoutgoing to the emergency room. He’s assessed for concussionby an on-site athletic trainer, but not in a well-documentedway. What documentation there is rarely makes it to theelectronic medical record. A few days later, the athlete’smother is troubled that he’s “still not quite right,” so theygo to a physician who must piece together conflictingrecollections of what happened. The physician puts theathlete through a battery of tests three days after the injury.Without baseline data, it’s difficult to know the extent andfocus of the patient’s impairment or how much recovery hastaken place. Management is hampered by this uncertainty,and the patient’s family grows dissatisfied, bouncing fromone provider to another. Even worse, the athlete may becleared prematurely because even though his functionaltest scores may look good, there is no way to know if he hasfully returned to normal function.Cleveland Clinic has a vision of how to change this model ofsports concussion care, and we are extending the benefits ofthis vision to nearly 12,000 young athletes in Northeast Ohio.The vision centers on our proprietary concussion application(app) for the Apple iPad 2, a collaboration among our Concussion Center, Department of Biomedical Engineering and Center for Sports Health. We believe it can change the trajectory ofconcussion care by enabling objective, affordable, point-of-careassessment of the multiple symptoms associated with concussion and providing this information to clinicians in a meaningful manner on a device that allows for interaction with the data.WHY AN iPAD APP?When we began exploring a software-based model to monitor concussions, we knew that measurement of motion andacceleration would be key. When the iPad 2 came along, with abuilt-in gyroscope and accelerometer, it fit the bill.The Cleveland Clinic Concussion (C3) app works by collectingposition and time-series data, along with linear and angularacceleration data, to assess balance and concussion symptomswhile an athlete performs clinical balance tests with an iPadattached to the waist (see photo). The app analyzes data toprovide objective and specific measures of cognitive and motorfunction as well as balance and postural stability. Validationstudies have shown that the app measures balance and postural stability with an accuracy equivalent to that of the systemconsidered the gold standard for such testing (but which is expensive, large and nonportable). The concussion-related factorsassessed by the app include: Information processingReaction time (both choice and simple)Working memoryDynamic visual acuityPostural stabilityVisual memoryINTO THE CLINIC AND ONTO THE FIELDAfter the validation studies, we systematically evaluated the C3app for use in the performance of a clinical balance test oftenused in concussion: the Balance Error Scoring System (BESS).During BESS testing, subjects stand on varying surfaces and invarying postures to allow assessment of their processing of visual information, somatosensory (tactile) information and vestibular information from the inner ear. Whereas the traditionalBESS test depends on a clinician’s subjective judgment, ourstudy showed that the C3 app enables highly objective, quantitative BESS scoring that is also more sensitive than scoringby clinical observation alone, allowing greater discriminationbetween various concussive conditions. This study is in press.
Visit clevelandclinic.org/orthoNext came a preliminary field study using the C3 app to gatherbaseline postural stability and functional data from 120Cleveland-area high school and college athletes. The aim wasto provide a benchmark to compare against if any of themlater sustained concussion. Twelve of these athletes sufferedconcussions during the season studied. We have learned fromthese 12 cases that concussion appears to leave a distinct“fingerprint” in different individuals in terms of the functionsmost affected. For instance, some individuals have substantialimpairment in dynamic visual acuity while others have none,and some individuals suffer major balance impairments whilebalance is unaffected in others. We are also examining the rateof recovery of these affected functions over time to see how thatfits into the broader concussive fingerprint. A manuscript onthis study is in development.FALL2012Figure. “Performance polygon” plot for a subject who sustained a headinjury on May 10, 2012 (see text for details on polygon tool). (CAP cognitive assessment profile; SRT simple reaction time; CRT choicereaction time; VOR vestibular ocular reflex; BESS Balance ErrorScoring System)‘PERFORMANCE POLYGON’ GUIDES CLINICAL MANAGEMENTCURRENT AND NEXT STEPSOur studies of functional return following concussion arefacilitated by a method of data visualization we call the “performance polygon.” It plots an individual’s scores in nine performance domains (Figure) on the first post-concussion iPadassessment and periodically thereafter to allow easy visualmonitoring of recovery to baseline levels (outer trace in Figure)over time. Depicting all domains in a single view makes therelative impairments in — and rates of recovery of — variousdomains readily apparent. This is valuable to clinicians for pinpointing the functional domains of concern and guiding themost appropriate therapy, and it helps patients easily understand what the treatment priorities are and why.In 2012, Cleveland Clinic has used the C3 app to complete baseline functional assessments for nearly 6,000 young athletes whoplay contact sports (e.g., football, men’s and women’s soccer) atthe more than 50 high schools and colleges across NortheastOhio that have Cleveland Clinic certified athletic trainers. Weare using these baseline data to realize our vision for optimalcare should any of these athletes sustain a head injury. We arealso making the C3 app available for post-injury assessmentamong an additional 6,000 young athletes who are managed byour trainers but who play noncontact sports or have not yet beenscheduled for baseline assessment.The clinical utility of this polygon tool underscores the importance of obtaining the athlete’s baseline assessment as well asassessments immediately after the injury and then frequentlythereafter to monitor recovery.Equally important is complete documentation of what happened at the time of injury, which the C3 app enables by providing the athletic trainer with a comprehensive questionnairethat elicits essential information about the incident and initialsymptoms, which may later be valuable to a treating physician.It does so systematically, using drop-down menus and numericcoding to allow direct integration into the electronic medicalrecord. The data are also integrated into Cleveland Clinic’sKnowledge Program interactive clinical database, which promotes management using our Concussion Carepath, an onlineevidence-based protocol designed to reduce variability of careacross the health system and improve patient outcomes.Our next aim is to explore broader deployment of the app,together with our Concussion Carepath, for coordinated useby schools and hospitals across the country. Together thesehighly transferable tools have the potential to take much of theguesswork out of concussion assessment and care, allowingphysicians to make safer return-to-play decisions.ABOUT THE AUTHORSDr. Alberts is Director of the Cleveland Clinic Concussion Center.He also holds an endowed chair in the Center for NeurologicalRestoration and the Department of Biomedical Engineering.He can be reached at 216.445.3222 or albertj@ccf.org.Dr. Figler is a primary care sports medicine specialist in the Centerfor Sports Health within the Department of Orthopaedic Surgery.His specialty interests include pediatric and adolescent sportsinjuries and sports-related concussions. He can be reached at440.519.6800 or figlerr@ccf.org.7
8Orthopaedic InsightsFor referrals, please call 216.445.0096 or 800.223.2273, ext.50096Aggressive Surgical Treatment of DiabeticAnkle Fractures Minimizes ComplicationsBy Mark Berkowitz, MDDiabetic patients with ankle fractures represent a distinctpatient subset characterized by multiple comorbidities, greatersurgical pitfalls and a well-accepted increased rate of complications. Nevertheless, successful treatment of ankle fracturein the diabetic patient is attainable by adopting an aggressive,multifaceted treatment approach that addresses the majorcauses of failure.AN INCREASINGLY COMPLEX PROBLEMDiabetic patients possess a long list of characteristics thatcan complicate ankle fracture treatment. Increased prevalences of peripheral vascular and coronary artery disease,obesity and peripheral neuropathy all contribute to a higherincidence of malunion and problems with wound healing.Charcot neuroarthropathy can exist at the time of ankle fracture or develop during treatment. In either case, profounddeformity and loss of fixation after ORIF commonly result.The challenges are even greater in the increasing number ofdiabetics who undergo gastric bypass surgery or kidneypancreas transplantation. Gastric bypass patients often haveprofound osteopenia that contributes to more comminutedinjury patterns and more difficult fixation. Transplant patientsrequire powerful immunosuppressive medications that increase the risk of infectious complications after surgery.RISK REDUCTION, NOT RISK ELIMINATIONThere is no way to completely eliminate the risk of seriouscomplications in the diabetic patient with a fractured ankle.Although nonoperative treatment may appear attractive inthe diabetic patient with multiple comorbidities, even nonsurgical treatment can be extremely problematic. Lackof protective sensation and inability to avoid weight bearingcan result in loss of reduction and skin breakdown withcast treatment, particularly in unstable fractures.Unstable ankle fractures are best treated surgically, even inthe complex diabetic population. Achieving a stable anatomicreduction facilitates union, simplifies cast changes and radiographic monitoring, and gives the patient the best possiblechance to return to an acceptable level of function. However, anumber of technique alterations should be considered in thediabetic patient to minimize the risk of complication.PREOPERATIVE MANAGEMENTPreoperative management is the first consideration. Anklefracture surgery should be delayed in the diabetic patient toallow for preoperative medical optimization and resolutionof swelling. The soft-tissue envelope should be as quiescentas possible before surgical treatment proceeds. Fracture blisters, if present, should be re-epithelialized, and skin wrinklesshould be present. A delay of two weeks is not atypical forankle fracture in a diabetic patient. This approach mirrorsthe one routinely used in treating pilon and calcaneusfractures in the nondiabetic population.However, a delay before surgery is feasible only if a successfuland well-done closed reduction and splinting is performed.While mild residual talar subluxation after closed reduction may be well tolerated in the young, healthy, nondiabeticpatient, a suboptimal reduction can lead to severe soft-tissuebreakdown in the diabetic patient. Thus, the goal of closedreduction in the diabetic patient must be near-anatomicreduction of the talus beneath the tibia.Post-reduction splinting must also be performed to an exactingstandard. The splint must be molded appropriately to maintainthe reduced talus within the mortise. The splint should bewell padded over the malleoli but not so padded that a reduction cannot be maintained. Bulky Jones cotton, while usefulas postoperative cast padding, is not ideal for maintaininga closed reduction, as it inhibits proper molding of the plaster.AN AGGRESSIVE SURGICAL APPROACHAt Cleveland Clinic, we have adopted an aggressive surgical approach to the diabetic ankle fracture. This may seemcounterintuitive in the medically complex, at-risk diabeticpatient. But precisely because these patients possess so manyrisk factors for failure, internal fixation must be employed ina manner aggressive enough to counter these risks.The goal of surgical treatment is to maximize ankle stability (Figure 1). To this end, posterior malleolar fractures areroutinely reduced and stabilized with posterior buttress platingthrough a posterolateral approach. Applying the fibular plateto the posterior or posterolateral surface of the fibula usingthis same posterolateral incision further enhances construct
Visit clevelandclinic.org/orthoAFALLBC2012DFigure 1. (A, B) Injury radiographs showing ankle fracture in a diabetic patient with a history of gastric bypass surgery and kidney-pancreas transplantation on immunosuppressive medications. (C, D) Aggressive and comprehensive internal fixation was performed, including placement of a posterolateralfibular locking plate, posterior and medial buttress plates and a supplementary syndesmotic screw.Figure 2. (A) Severesupination-adductionfracture dislocation in a61-year-old diabeticfemale with a history ofCharcot neuroarthropathyon the contralateral side.(B) Successful stabilizationwith a transarticularscrew and an Ilizarovexternal fixator.continued on next pageAB9
10Orthopaedic Insightsstability. Anatomically contoured fibular locking plates provideanother means of increasing stability, particularly when osteopenia is severe.Liberal placement of supplementary syndesmotic-type screwsfrom the fibula into the tibia is also recommended in thediabetic patient. These screws significantly enhance stabilityby engaging the relatively strong cortices of the tibia. They especially merit consideration in cases of deltoid ligament rupture.Another helpful technique modification is the use of a tension band wire construct for the medial malleolus fracture.From the standpoint of fragment size, tension band wiring isparticularly useful in stabilizing a small anterior colliculusfracture. And because the stability of tension band wiring is notas dependent on bone quality, it is equally useful for osteopenicor comminuted medial malleolus fractures.SPECIAL CIRCUMSTANCESThe diabetic ankle fracture in the setting of severe peripheralneuropathy or early Charcot neuroarthropathy requires anequally aggressive but different approach. Patients with theseconditions are often identified by their lack of pain and lackof protective sensation. At Cleveland Clinic, these patientshave been successfully treated using a combination of percutaneous transarticular screws and fine-wire external fixation.For referrals, please call 216.445.0096 or 800.223.2273, ext.50096Percutaneous transarticular screw placement provides afast, simple and minimally invasive means of stabilizingeven an extremely unstable ankle fracture. Any joint damagecaused by the screws has little consequence, as a result of theperipheral neuropathy. The screws are generally removed atthree months, before initiation of weight bearing. In patientswith severe osteopenia or Charcot changes, additional stability is achieved using an Ilizarov external fixator, either inaddition to transarticular screws or as stand-alone fixation.Although more complex and time-consuming to apply, finewire fixation provides tremendous stability and encouragesadherence to restrictions against weight bearing (Figure 2).CONCLUSION: Success is attainableAnkle fractures in diabetic patients are becoming morecommon and problematic, not less. The good news is thatsuccessful treatment is still attainable using an aggressiveapproach that anticipates and addresses potential complications.ABOUT THE AUTHORDr. Berkowitz is a staff surgeon in the Department ofOrthopaedic Surgery specializing in foot and ankle andlower extremity trauma surgery. He can be contactedat 216.444.7607 or berkowm@ccf.org.Patient-Specific Instrumentation Promisesa Better Surgical Fit in Total Knee ReplacementBy Trevor G. Murray, MD, and Alison Klika, MSThe number of total knee replacements (TKRs) performedannually in the United States doubled from 1999 to 2008 andis projected to rise by an additional 600 percent by 2030.Consistent with this trend, the volume of TKR proceduresperformed at Cleveland Clinic has risen 30 percent over thelast five years. These increases are attributable to an expansionof indications to younger and more active patients as wellas to the burgeoning population of aging baby boomers. Thesepatients are demanding more from their joint replacementsthan ever before.THE QUEST TO SATISFY PATIENT DEMANDSThe rising expectations of today’s TKR patients have spurredthe pursuit of improvements in the design, delivery andexecution of TKR. A recent technological focus is patientspecific positioning guides, which are custom guides made tomatch an individual patient’s anatomy, potentially allowingthe surgeon to more efficiently and accurately perform TKR.Most of the major orthopaedic implant manufacturers offerversions of this technology, all of which are based on themechanical axis. CT or MRI scanning with or without a longleg radiograph is used to build the custom cutting blocks.Many facilities within the Cleveland Clinic health systemare equipped with the imaging protocols required by thedevice manufacturers to facilitate production of these guides,enabling patients to be accommodated with minimalinconvenience.
Visit clevelandclinic.org/orthoFALL2012GOALS OF TKR CAN BE ELUSIVEThe goals for arthroplasty are to reduce pain and restorefunction by way of a well-placed, durable TKR. Many laboratoryinvestigations, finite element studies and clinical outcometrials have demonstrated that appropriate alignment is criticalto achieving these objectives. Traditional cutting guides aidin the placement of components, but studies have shown thatthere is room for improvement. Navigation systems were developed with the hope of improving accuracy and reproducibilityof TKR, although literature reports have been conflictingand emphasize concerns about increased cost, time in theoperating room (OR) and complications.PROPOSED BENEFITS OF A PATIENT-SPECIFIC APPROACHPatient-specific cutting guides (see Figure for example)offer several potential benefits, including reduced OR time,increased efficiency in case preparation, decreased bloodloss and improved outcomes secondary to improvedcomponent alignment.This technology takes the “navigation” portion of the procedure, and all the time that it requires, out of the OR. The planis established preoperatively and can quickly be implementedat the time of surgery. The custom guides pin onto the distalfemur and proximal tibia without violating either canal. Thetheoretical advantages of this approach include reduced bloodloss, which in turn should reduce transfusion requirementsand ultimately decrease infection rates.Customization allows the operation to be performed withfewer tools and trays, resulting in decreased turnover time andimproved OR efficiency. Although the use of patient-specificguides does increase up-front costs to the hospital, it has beensuggested that these costs may be offset by the reductions inOR time and by lower revision rates as a result o
2 ORTHOPAEDIC INSIGHTS For referrals, please call 216.445.0096 or 800.223.2273, ext.50096 Dear Colleague, Welcome to the Fall 2012 issue of Orthopaedic Insights from Cleveland Clinic’s Department of Orthopaedic Surgery. We bring y
Clinic County Clinic Name Clinic Address Clinic City Clinic Zip Participant County Participant Gender Enrollment Status Fax Received Date BLACK HAWK CHRIST, MEREDITH - IAM 1015 S HACKETT RD WATERLOO 50701 BLACK HAWK Female Unreachable 4/21/2014
4,994 Alamosa VA Clinic 24,091 Aurora VA Clinic 1,430 Burlington VA Clinic 17,685 Denver VA Clinic: 63,884 Golden VA Clinic: 2,311 IDES 15,372 Jewell VA Clinic 4,343 La Junta VA Clinic 1,580 Lamar VA Clinic 172,745 PFC Floyd K. Lindstrom VA Clinic 66,385 PFC James Dunn VA Clinic 583,038 Rocky Mountain Regional VA Medical Center 874 Salida VA .
Veterans Review and Veterans Review and Appeal Board “Your right to be heard” ORTHOPAEDIC HANDBOOK Prepared by: Stanish Orthopaedic Inc. Professor of Orthopaedic Surgery, Dalhousie University Director, Orthopaedic and Sport Medicine Clinic of Nova Scotia Hali
Consultant Paediatric Orthopaedic Surgeon Maidstone and Tunbridge Wells NHS Trust Kent, UK Deborah Eastwood Consultant Paediatric Orthopaedic Surgeon Great Ormond Street Hospital for Children and Royal National Orthopaedic Hospital Middlesex UK David Evans Consultant Hand Surgeon The Hand Clinic Berks, UK Mark Falworth Consultant Orthopaedic .
for Brain Health in Las Vegas, Cleveland Clinic Canada, Sheikh Khalifa Medical City and Cleveland Clinic Abu Dhabi. In 2016, Cleveland Clinic was ranked the No. 2 hospital in America in U.S. News & World Report’s “Best Hospitals” survey. The survey ranks Cleveland Clinic among the nat
fracture clinic held Monday-Friday at RAH and IRH Emergency referral of all orthopaedic cases should be made to the orthopaedic FY2 at RAH and the on call orthopaedic registrar at IRH. Paediatric fractures requiring emergency orthopaedic discussion and assessment should be discussed with senior doctors. .
Cleveland Clinic Case Study page 4 The Clinic's New People Strategy In the spring of 2008, with these disappointing HCAHPS and Gallup survey results in hand, the Clinic's executive leadership team approved a new "people strategy" designed to make the Clinic a "great place to
Abrasive water jet machining (AWJM) process is one of the most recent developed non-traditional machining processes used for machining of composite materials. In AWJM process, machining of work piece material takes place when a high speed water jet mixed with abrasives impinges on it. This process is suitable for heat sensitive materials especially composites because it produces almost no heat .