Nutrition Journal BioMed
Nutrition JournalBioMed CentralOpen AccessReviewNutritional therapies for mental disordersShaheen E Lakhan* and Karen F VieiraAddress: Global Neuroscience Initiative Foundation, Los Angeles, CA, USAEmail: Shaheen E Lakhan* - slakhan@gnif.org; Karen F Vieira - kvieira@gnif.org* Corresponding authorPublished: 21 January 2008Nutrition Journal 2008, 7:2doi:10.1186/1475-2891-7-2Received: 28 July 2007Accepted: 21 January 2008This article is available from: http://www.nutritionj.com/content/7/1/2 2008 Lakhan and Vieira; licensee BioMed Central Ltd.This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.AbstractAccording to the Diagnostic and Statistical Manual of Mental Disorders, 4 out of the 10 leadingcauses of disability in the US and other developed countries are mental disorders. Majordepression, bipolar disorder, schizophrenia, and obsessive compulsive disorder (OCD) are amongthe most common mental disorders that currently plague numerous countries and have varyingincidence rates from 26 percent in America to 4 percent in China. Though some of this differencemay be attributable to the manner in which individual healthcare providers diagnose mentaldisorders, this noticeable distribution can be also explained by studies which show that a lack ofcertain dietary nutrients contribute to the development of mental disorders. Notably, essentialvitamins, minerals, and omega-3 fatty acids are often deficient in the general population in Americaand other developed countries; and are exceptionally deficient in patients suffering from mentaldisorders. Studies have shown that daily supplements of vital nutrients often effectively reducepatients' symptoms. Supplements that contain amino acids also reduce symptoms, because they areconverted to neurotransmitters that alleviate depression and other mental disorders. Based onemerging scientific evidence, this form of nutritional supplement treatment may be appropriate forcontrolling major depression, bipolar disorder, schizophrenia and anxiety disorders, eatingdisorders, attention deficit disorder/attention deficit hyperactivity disorder (ADD/ADHD),addiction, and autism. The aim of this manuscript is to emphasize which dietary supplements canaid the treatment of the four most common mental disorders currently affecting America and otherdeveloped countries: major depression, bipolar disorder, schizophrenia, and obsessive compulsivedisorder (OCD).Most antidepressants and other prescription drugs cause severe side effects, which usuallydiscourage patients from taking their medications. Such noncompliant patients who have mentaldisorders are at a higher risk for committing suicide or being institutionalized. One way forpsychiatrists to overcome this noncompliance is to educate themselves about alternative orcomplementary nutritional treatments. Although in the cases of certain nutrients, further researchneeds to be done to determine the best recommended doses of most nutritional supplements,psychiatrists can recommend doses of dietary supplements based on previous and currentefficacious studies and then adjust the doses based on the results obtained.IntroductionCurrently, approximately 1 in 4 adult Americans havebeen diagnosed with a mental disorder, which translatesinto about 58 million affected people [1]. Though thePage 1 of 8(page number not for citation purposes)
Nutrition Journal 2008, 7:2incidence of mental disorders is higher in America than inother countries, a World Health Organization study of 14countries reported a worldwide prevalence of mental disorders between 4.3 percent and 26.4 percent [2]. In addition, mental disorders are among the leading causes fordisability in the US as well as other countries. Commonmental health disorders include mood disorders, anxietydisorders such as post-traumatic stress disorder (PTSD),panic disorders, eating disorders, attention deficit disorder/attention deficit hyperactivity disorder (ADD/ADHD), and autism. However, the four most commonmental disorders that cause disabilities are major depression, bipolar disorder, schizophrenia, and obsessive compulsive disorder (OCD) [3,4].Typically, most of these disorders are treated with prescription drugs, but many of these prescribed drugs causeunwanted side effects. For example, lithium is usually prescribed for bipolar disorder, but the high-doses of lithiumthat are normally prescribed causes side effects thatinclude: a dulled personality, reduced emotions, memoryloss, tremors, or weight gain [5,6]. These side effects canbe so severe and unpleasant that many patients becomenoncompliant and, in cases of severe drug toxicity, the situation can become life threatening.Researchers have observed that the prevalence of mentalhealth disorders has increased in developed countries incorrelation with the deterioration of the Western diet [7].Previous research has shown nutritional deficiencies thatcorrelate with some mental disorders [8,9]. The mostcommon nutritional deficiencies seen in mental disorderpatients are of omega-3 fatty acids, B vitamins, minerals,and amino acids that are precursors to neurotransmitters[10-16]. Compelling population studies link high fishconsumption to a low incidence of mental disorders; thislower incidence rate has proven to be a direct result ofomega-3 fatty acid intake [10,17,18]. One to two grams ofomega-3 fatty acids taken daily is the generally accepteddose for healthy individuals, but for patients with mentaldisorders, up to 9.6 g has been shown to be safe and efficacious [19-21]. Western diets are usually also lacking infruits and vegetables, which further contributes to vitaminand mineral deficiencies.This article will focus on the nutritional deficiencies thatare associated with mental disorders and will outline howdietary supplements can be implemented in the treatmentof several disorders (see Table 1 for an overview). Themental disorders and treatments covered in this review donot include the broad and complex range of disorders, buthowever focuses on the four most common disorders inorder to emphasize the alternative or complementarynutritional options that health care providers can recommend to their jor DepressionMajor depression is a disorder that presents with symptoms such as decreased mood, increased sadness and anxiety, a loss of appetite, and a loss of interest in pleasurableactivities, to name a few [22]. If this disorder is not properly treated it can become disabling or fatal. Patients whoare suffering from major depression have a high risk forcommitting suicide so they are usually treated with psychotherapy and/or antidepressants [23]. Depression hasfor some time now been known to be associated with deficiencies in neurotransmitters such as serotonin,dopamine, noradrenaline, and GABA [22-27]. As reportedin several studies, the amino acids tryptophan, tyrosine,phenylalanine, and methionine are often helpful in treating many mood disorders, including depression [28-33].Tryptophan is a precursor to serotonin and is usually converted to serotonin when taken alone on an empty stomach. Therefore, tryptophan can induce sleep andtranquility and in cases of serotonin deficiencies, restoreserotonin levels leading to diminished depression[15,31].Tyrosine is not an essential amino acid, because it can bemade from the amino acid phenylalanine. Tyrosine andsometimes its precursor phenylalanine are converted intodopamine and norepinephrine [34]. Dietary supplementsthat contain tyrosine and/or phenylalanine lead to alertness and arousal. Methionine combines with ATP to produce S-adenosylmethionine (SAM), which facilitates theproduction of neurotransmitters in the brain [35-38].Currently, more studies involving these neurochemicalsare needed which exhibit the daily supplemental dosesthat should be consumed in order to achieve antidepressant effects.Since the consumption of omega-3 fatty acids from fishand other sources has declined in most populations, theincidence of major depression has increased [10]. Severalmechanisms of action may explain how eicosapentaenoicacid (EPA) which the body converts into docosahexaenoicacid (DHA), the two omega-3 fatty acids found in fish oil,elicit antidepressant effects in humans. Most of the proposed mechanisms involve neurotransmitters and, ofcourse, some have more supporting data than others. Forexample, antidepressant effects may be due to EPA beingconverted into prostaglandins, leukotrienes, and otherchemicals the brain needs. Other theories state that EPAand DHA affect signal transduction in brain cells by activating peroxisomal proliferator-activated receptors(PPARs), inhibiting G-proteins and protein kinase C, aswell as calcium, sodium, and potassium ion channels. Nomatter which mechanism(s) prove to be true, epidemiological data and clinical studies already show that omega3 fatty acids can effectively treat depression [39]. Consuming omega-3 fatty acid dietary supplements that containPage 2 of 8(page number not for citation purposes)
Nutrition Journal 2008, 7:2http://www.nutritionj.com/content/7/1/2Table 1: Summary of proposed causes and treatments for common mental health disordersMental DisorderProposed CauseTreatmentReferencesMajor DepressionSerotonin cyTyrosine[15][32][30][36]GABA deficiencyOmega-3 deficiencyFolate/Vitamin B deficiencyGABAOmega-3sFolate/Vitamin BMagnesium deficiencySAM deficiencyBipolar DisorderSchizophreniaObsessive CompulsiveDisorderType of StudyMagnesiumSAM[29][39][9][13][14][37]Human pilot clinical trialDouble-blind, placebo controlledDouble-blind, placebo controlledRandomized within or betweensubjectsClinical trialClinical trialRandomized controlled trialClinical trialCases studiesDouble-blind, placebo controlledExcess acetylcholinereceptorsExcess vanadiumVitamin B/Folate deficiencyLithium orotate & taurine[50]Clinical trialVitamin CVitamin B/FolateL-Tryptophan deficiencyCholine deficiencyOmega-3 [72][73][21][48][74][75]Double-blind, placebo controlledHuman pilot clinical trialClinical trialClinical trialDouble-blind, placebo controlledDouble-blind, placebo controlledClinical trialClinical trialDouble-blind, placebo e controlled trialDouble-blind, placebo controlledHuman pilot open-label trialClinical trialDouble-blind, placebo controlledRandomized, placebo controlledOpen-label clinical trial[69][70]Randomized, double-blind trialDouble-blind, placebo controlledImpaired serotonin synthesis TryptophanGlycine deficiencyGlycineOmega-3 deficienciesOmega-3sSt. John's wort deficiencySt John's wort1.5 to 2 g of EPA per day have been shown to stimulatemood elevation in depressed patients. However, doses ofomega-3 higher than 3 g do not present better effects thanplacebos and may not be suitable for some patients, suchas those taking anti-clotting drugs [40].In addition to omega-3 fatty acids, vitamin B (e.g., folate),and magnesium deficiencies have been linked to depression [9,13,14]. Randomized, controlled trials that involvefolate and B12 suggest that patients treated with 0.8 mg offolic acid/day or 0.4 mg of vitamin B12/day will exhibitdecreased depression symptoms [9]. In addition, theresults of several case studies where patients were treatedwith 125 to 300 mg of magnesium (as glycinate or taurinate) with each meal and at bedtime led to rapid recoveryfrom major depression in less than seven days for most ofthe patients [14].Bipolar DisorderA patient suffering from major depression may alsopresent symptoms such as recurring episodes of debilitat-ing depression, uncontrollable mania, hypomania, or amixed state (a manic and depressive episode) which isclinically diagnosed as bipolar disorder [41]. Some biochemical abnormalities in people with bipolar disorderinclude oversensitivity to acetylcholine, excess vanadium,vitamin B deficiencies, a taurine deficiency, anemia,omega-3 fatty acid deficiencies, and vitamin C deficiency.Bipolar patients tend to have excess acetylcholine receptors, which is a major cause of depression and mania[42,43]. Bipolar patients also produce elevated levels ofvanadium, which causes mania, depression, and melancholy [44,45]. However, vitamin C has been shown toprotect the body from the damage caused by excess vanadium. A double-blind, placebo controlled study thatinvolved controlling elevated vanadium levels showedthat a single 3 g dose of vitamin C decreases manic symptoms in comparison to placebo [45].Taurine is an amino acid made in the liver from cysteinethat is known to play a role in the brain by eliciting aPage 3 of 8(page number not for citation purposes)
Nutrition Journal 2008, 7:2http://www.nutritionj.com/content/7/1/2calming effect. A deficiency of this amino acid mayincrease a bipolar patient's manic episodes. In addition,eighty percent of bipolar sufferers have some vitamin Bdeficiencies (often accompanied by anemia) [46]. Thecombination of essential vitamin supplements with thebody's natural supply of lithium reduces depressive andmanic symptoms of patients suffering from bipolar disorder [47].Another well-known factor for mental disorders is thatcells within the brain require omega-3 oils in order to beable to transmit signals that enable proper thinking,moods, and emotions. However, omega-3 oils are oftenpresent at very low levels in most Americans and bipolarsufferers [48]. Numerous clinical trials, including doubleblind, placebo controlled studies have been performedwhich show that 1 to 2 grams of omega-3 fatty acids in theform of EPA added to one's daily intake decreases manic/depressive symptoms better than placebo (See Table 1).Prescription lithium is in the form of lithium carbonate,and doses can be as high as 180 mg. It is these high dosesthat are responsible for most of lithium's adverse sideeffects. Some of the more common side effects include adulled personality, reduced emotions, memory loss, tremors, or weight gain [5,6]. Another form of lithium calledlithium orotate, is preferred because the orotate ioncrosses the blood-brain barrier more easily than the carbonate ion of lithium carbonate. Therefore, lithium orotate can be used in much lower doses (e.g. 5 mg) withremarkable results and no side effects [49,50]. Clinical trials involving 150 mg daily doses of lithium orotateadministered 4 to 5 times a week, showed a reduction ofmanic and depressive symptoms in bipolar patients [50].In addition, lithium orotate is available without a prescription, unlike lithium carbonate, which is considered aprescription drug by the Food and Drug Administration(FDA). Studies have also shown that the amino acidderivative, taurine, as an alternative to lithium, blocks theeffects of excess acetylcholine that contributes to bipolardisorder [51].Numerous studies for bipolar disorder have been published that list specific lifestyle changes as well as amountsof dietary supplements that can be used to treat this disorder. A summary of these results is listed in Table 2.SchizophreniaSchizophrenia is a mental disorder that disrupts a person'snormal perception of reality. Schizophrenic patients usually suffer from hallucinations, paranoia, delusions, andspeech/thinking impairments. These symptoms are typically presented during adolescence [52]. Disturbances inamino acid metabolism have been implicated in thepathophysiology of schizophrenia. Specifically, animpaired synthesis of serotonin in the central nervous system has been found in schizophrenic patients [53]. Highdoses (30 g) of glycine have been shown to reduce themore subtle symptoms of schizophrenia, such as socialwithdrawal, emotional flatness, and apathy, which do notrespond to most of the existing medications [54-56]. Anopen-label clinical trial performed in 1996 revealed that60 g of glycine per day (0.8 g/kg) could be given to schizophrenic patients without producing adverse side effectsand that this dose led to a two-fold increase in cerebrospinal fluid (CSF) glycine levels [55]. A second clinical studytreated patients with the same dosage divided into 3 dosesTable 2: List of possible causes and treatments for bipolar disorder including specific doses as well as supplementary informationMentalDisorderProposed CauseTreatmentReferencesBipolar DisorderFood allergiesCaffeineAvoid foods that elicit an allergic responseAvoid coffee and other caffeinatedbeveragesAvoid alkalizing agents like bicarbonates100–200 milligrams/day300–600 mcirograms/day1–3 grams taken as divided doses200 micrograms/day10–30 grams of phosphatidyl form individed doses500–1000 milligrams/dayInitially 500 milligrams/day; can increase to3–4 grams/day50–200 milligrams taken as divided doses800 milligrams3–6 milligrams at 9 pm100 milligrams with food[76, 77][78]Inhibition of lithium from alkalizing agentsVitamin B6 deficiencyVitamin B12 deficiencyVitamin C deficiencyFolate deficiencyCholine deficiencyOmega-3 or -6 deficiencyPhenylalanine deficiencyTryptophan deficiencyS-Adenosyl-L-Methionine (SAM) deficiencyMelatonin deficiencyPhosphatidylserine deficiency[79][72, 80][71, 81–83][84–86][9, 13, 71, 82, 83, 87, 88][73, 89][10, 11, 21, 39, 74, 75, 90–94][95, 96][97–100][101–103][104–106][107]Page 4 of 8(page number not for citation purposes)
Nutrition Journal 2008, 7:2within 1 week. This form of glycine treatment led to aneight-fold increase in CSF glycine levels [56].The most consistent correlation found in one study thatinvolved the ecological analysis of schizophrenia and dietconcluded that increased consumption of refined sugarresults in an overall decreased state of mind for schizophrenic patients, as measured by both the number of daysspent in the hospital and poor social functioning [57].That study also concluded that the dietary predictors ofthe outcome of schizophrenia and prevalence of depression are similar to those that predict illnesses such as coronary heart disease and D [67]. Therefore, it is clear that nutrients whichincrease serotonin levels will reduce the symptoms ofOCD. As discussed earlier, the amino acid tryptophan is aprecursor to serotonin, and tryptophan supplements(which are better than 5-Hydroxytryptophan) willincrease serotonin levels and treat OCD [68].A Danish study showed that better prognoses for schizophrenic patients strongly correlate with living in a countrywhere there is a high consumption of omega-3 fatty acids[58]. Eicosapentaenoic acid (EPA), which is found inomega-3 fish oils, has been shown to help depressivepatients and can also be used to treat schizophrenia[41,42,59]. Furthermore, studies suggest that supplements such as the commercially available VegEPA capsule,when taken on a daily basis, helps healthy individuals andschizophrenic patients maintain a balanced mood andimproves blood circulation [59-65].A commercially available supplement called Amoryn hasrecently proven to help patients suffering from depression, anxiety, and OCD [69,70]. The main ingredient inAmoryn, St. John's wort, has been shown to help OCDpatients better deal with their recurring thoughts andcompulsions. Two double-blind, placebo-controlledstudies were recently performed that compared the affectsof a 900 mg daily dose of St. John's wort extract to 20 mgdaily doses of Paroxetine (Paxil) or Fluoxetine; which areboth SSRIs used to treat OCD. In comparison to patientstaking Paxil, those who took the St. John's wort supplement showed a 57% decrease in OCD symptoms andwere 47% less likely to exhibit side effects [69]. In comparison to patients taking Fluoxetine, consumption of theSt. John's wort extract reduced 48% of OCD patient'ssymptoms [70]. These results clearly depict how the usenutritional supplements can be effective treatments formental disorders.The VegEPA capsule contains:Conclusion 280 milligrams of EPA from marine omega-3 fish oil 100 milligrams of organic virgin evening primroseomega-6 oil 1 milligram of the anti-oxidant vitamin E An outer capsule made out of fish gelatineFor schizophrenic patients, docosahexaenoic acid (DHA)supplements inhibit the effects of EPA supplements so itis recommended that the patient only takes the EPA supplement, which the body will convert into the amountDHA it needs [59-65]. Double-blind, placebo controlledstudies, randomized, placebo controlled studies, andopen-label clinical studies have all shown that approximately 2 g of EPA taken daily in addition to one's existingmedication effectively decreases symptoms in schizophrenic patients [59,60,65].Obsessive-Compulsive DisorderObsessive compulsive disorder (OCD) is an anxiety disorder that causes recurring stressful thoughts or obsessionsthat are followed by compulsions, which are repeated inan uncontrollable manner as a means of repressing thestressful thought [66]. It is well documented that selectiveserotonin reuptake inhibitors (SSRIs) help patients withHere we have shown just a few of the many documentednutritional therapies that can be utilized when treatingmental disorders. Many of these studies were done in the1970s and 1980s, but were soon discontinued becausethey were underfunded. Nutritional therapies have nowbecome a long-forgotten method of treatment, becausethey were of no interest to pharmaceutical companies thatcould not patent or own them. Instead, the companiesthat funded most clinical research spent their dollarsinvestigating synthetic drugs they could patent and sell;these drugs however usually caused adverse side effects.There is tremendous resistance to using supplements astreatments from clinicians, mostly due to their lack ofknowledge on the subject. Others rather use prescriptiondrugs that the drug companies and the FDA researches,monitors and recalls if necessary. However, for somepatients, prescription drugs do not have the efficacy ofnutritional supplements and they sometimes have farmore dangerous side effects. So for clinicians to avoidthese supplement therapies because of a lack of knowledge and unwillingness to use treatments not backed bydrug companies and the FDA, they are compromisingtheir patients' recovery due to their own laziness or selfishness.Clinical studies that show the ability of a prescriptiondrug to effectively treat mental disorders will often arguePage 5 of 8(page number not for citation purposes)
Nutrition Journal 2008, 7:2http://www.nutritionj.com/content/7/1/2that supplements as treatments, when unmonitored, aremore risky than prescription drugs and may ineffectivelytreat a patient's symptoms. For example one study listedseveral methods of treatment, none of which include natural compounds, for OCD patients that include: megadoses of SSRIs, intravenous chlomipramine, oralmorphine, deep brain stimulation, and functional neurosurgery [67]. Most of these treatments are invasive orunnatural and will inevitably cause severe side effects tothe patient, whose symptoms will probably still reoccurover time. Another example of the literature scaring clinicians away from supplement therapies is an article thatwarns patients about the dangers of consuming highamounts of omega-3 fatty acids. This manuscript involvesa patient who was taking approximately 10 times morethan the recommended dose of omega-3 supplements[40]. Numerous studies have shown that up 2 grams ofEPA (omega-3 fatty acid) taken daily is sufficient fordecreasing symptoms of several mental health disorderswith no side effects. This publication with a megadose ofomega-3 fatty acids stresses the importance of monitoringthe consumption of supplements as well as prescribeddrugs, preferably through regular consultations with alicensed health care professional.treatment, nutritional therapy should be supervised anddoses should be adjusted as necessary to achieve optimalresults.Proper medical diagnosis and a clear description of allpossible treatment options should always be the first planof action when treating mental disorders. However, thefinal decision on whether or not to try nutritional supplements as a treatment must be based on the patient preferences. Now with consumers becoming more interested innatural and holistic therapies, nutritional therapies havebeen well-received, and some studies are again underwayin these areas. New well-designed clinical studies arebeing published daily on the positive effects of nutritionaland supplement therapies on all types of disorders anddiseases. It will take some time for clinicians to becomeeducated on all the options available, but this is an important task that should not be ignored.SAM: S-adenosylmethionineThose with influence in this field should continue toexamine natural treatments on the scientific level in orderto increase the availability of grant money for this type ofresearch. This will lead to a surge of researchers who willsubmit proposals for grants enabling laboratories to further investigate the hypothesis that proper nutrition contributes to better mental health.Psychiatrists treating patients with mental disordersshould be aware of available nutritional therapies, appropriate doses, and possible side effects in order to providealternative and complementary treatments for theirpatients. This may reduce the number of noncompliantpatients suffering from mental disorders that choose notto take their prescribed medications. As with any form ofAbbreviationsADD: attention deficit disorderADHD: attention deficit hyperactivity disorderCSF: cerebrospinal fluidDHA: docosahexaenoic acidEPA: eicosapentaenoic acidFDA: Food and Drug AdministrationGABA: gamma-aminobutyric acidOCD: obsessive-compulsive disorderPPARs: peroxisomal proliferator-activated receptorsPTSD: post-traumatic stress disorderSSRI: selective serotonin reuptake inhibitorsReferences1.2.3.4.5.6.7.8.9.10.Kessler RC, Chiu WT, Demler O, Walters EE: Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders inthe National Comorbidity Survey Replication (NCS-R).Archives of General Psychiatry 2005, 62(6):617-627.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V,Lepine JP, Angermeyer MC, Bernert S, de Girolamo G, Morosini P,Polidori G, Kikkawa T, Kawakami N, Ono Y, Takeshima T, Uda H,Karam EG, Fayyad JA, Karam AN, Mneimneh ZN, Medina-Mora ME,Borges G, Lara C, de Graaf R, Ormel J, Gureje O, Shen Y, Huang Y,Zhang M, Alonso J, Haro JM, Vilagut G, Bromet EJ, Gluzman S, WebbC, Kessler RC, Merikangas KR, Anthony JC, Von Korff MR, Wang PS,Brugha TS, Aguilar-Gaxiola S, Lee S, Heeringa S, Pennell BE, ZaslavskyAM, Ustun TB, Chatterji S, WHO World Mental Health Survey Consortium: Prevalence, severity, and unmet need for treatmentof mental disorders in the World Health OrganizationWorld Mental Health Surveys. JAMA 2004, 291(21):2581-2590.Murray CJL, Lopez AD: The Global Burden Of Disease. WorldHealth Organization 1996:270.American Psychiatric A: Diagnostic and Statistical Manual ofMental Disorders. Fourth edition, text revision Washington DC 2000.Waring WS: Management of lithium toxicity. Toxicol Rev 2006,25(4):221-230.Vieta E, Rosa AR: Evolving trends in the long-term treatmentof bipolar disorder. World J Biol Psychiatry 2007, 8(1):4-11.Young SN: Clinical nutrition: 3. The fuzzy boundary betweennutrition and psycopharmacology. CMAJ 2002, 166(2):205-209.Wurtman R, O'Rourke D, Wurtman JJ: Nutrient imbalances indepressive disorders. Possible brain mechanisms. Ann N YAcad Sci 1989, 575:75-82.Young SN: Folate and depression–a neglected problem. J Psychiatry Neurosci 2007, 32(2):80-82.Hibbeln JR: Fish consumption and major depression. The Lancet1998, 351(9110):1213.Page 6 of 8(page number not for citation purposes)
Nutrition Journal 2008, .27.28.29.30.31.32.33.34.35.36.Rudin DO: The major psychoses and neuroses as omega-3essential fatty acid deficiency syndrome: substrate pellagra.Biol Psychiatry 1981, 16(9):837-850.Rudin DO: The dominant diseases of modernized societies asomega-3 essential fatty acid deficiency syndrome: substrateberiberi. Med Hypotheses 1982, 8(1):17-47.Bell IR, Edman JS, Morrow FD, Marby DW, Mirages S, Perrone G,Kayne HL, Cole JO: B complex vitamin patterns in geriatricand young adult inpatients with major depression. J Am GeriatrSoc 1991, 39(3):252-257.Eby GA, Eby KL: Rapid recovery from major depression usingmagnesium treatment. Med Hypotheses 2006, 67(2):362-370.Buist R: The therapeutic predictability of tryptophan andtyrosine in the treatment of depression. Int J Clin Nutr Rev 1983,3:1-3.Chouinard G, Young SN, Annable L: A controlled clinical trial ofL-tryptophan in acute mania. Biol Psychiatry 1985, 20(5):546-547.Reis LC, Hibbeln JR: Cultural symbolism of fish and the psychotropic properties of omega-3 fatty acids. Prostaglandins LeukotEssent Fatty Acids 2006, 75(4–5):227-236.Tanskanen A, Hibbeln JR, Hintikka J, Haatainen K, Honkalampi K, Viinamaki H: Fish consumption, depression, and suicidality in ageneral population. Arch Gen Psychiatry 2001, 58(5):512-513.von Schacky C: A review of omega-3 ethyl esters for cardiovascular prevention and treatment of increased blood triglyceride levels. Vasc Health Risk Manag 2006, 2(3):251-262.Eritsland J: Safety considerations of polyunsaturated fattyacids. Am J Clin Nutr 2000, 71(1 Suppl):197S-201S.Stoll AL, Severus WE, Freeman MP, Rueter S, Zboyan HA, DiamondE, Cress KK, Marangell LB: Omega 3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial.Arch Gen Psychiatry 1999, 56(5):407-412.National Institute of Mental Health: Depression. National Institute ofMental Health, National Institutes of Health 2000. US Department ofHealth and Human Services, Bethesda (MD) [Reprinted September2002].Rush AJ: The varied clinical
Bipolar Disorder Excess acetylcholine receptors Lithium orotate & taurine [50] Clinical trial Excess vanadium Vitamin C [45] Double-blind, placebo controlled Vitamin B/Folate deficiency Vitamin B/Folate [47] [71] Human pilot clinical trial Clinical trial
The Nutrition Care Process is defined in four steps: 1. Nutrition Assessment 2. Nutrition Diagnosis 3. Nutrition Intervention 4. Nutrition Monitoring & Evaluation The first component of the “Nutrition Assessment” is a screening of residents for those at risk for nutrition problems and is a candidate for further intervention. One of the
Nutrition during a woman's life From: ACC/SCN and IFPRI. 4th Report on the World Nutrition Situation: Nutrition Throughout the Life Cycle. Geneva: WHO, 2000. Nutrition during a woman's life From: ACC/SCN and IFPRI. 4th Report on the World Nutrition Situation: Nutrition Throughout the Life Cycle. Geneva: WHO, 2000.
Nutrition Evaluation: the systematic comparison of current findings with the previous status, nutrition intervention goals, effectiveness of overall nutrition care, or a reference standard Nutrition Care Outcomes: the results of nutrition care that are directly related to the nutrition diagnosis and the goals of the intervention plan
BioMed 4100 Veterinary Clinical Chemistry, On-line BioMed 4110/V_PBIO 7110 Veterinary Cytology BioMED 4120 Principles of Toxicology On-line LAB_AN 9437 Lab Animal Pathology . Hematology Rounds Human Health and the Environment - Image Review Joint Pathology Center Wednesday Slide Conference
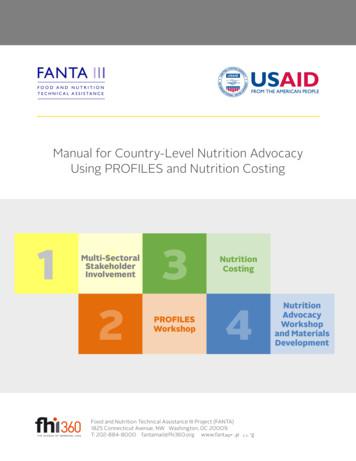
Manual for Country-Level Nutrition Advocacy . Using PROFILES and Nutrition Costing. FANTA III. FOOD AND NUTRITION TECHNICAL A SSISTANCE. Food and Nutrition Technical Assistance III Project (FANTA) 1825 Connecticut Avenue, NW Washington, DC 20009 T: 202-884-8000 fantamail@fhi360.org www.fantaproject.org. 1. 3. Nutrition . 1 Costing. Multi-Sectoral
healthcare team may complete nutrition screening. Nutrition screening should be completed upon admission to a healthcare setting and when nutrition risk is triggered, there should be an automatic referral to the registered dietitian (RD) or the nutrition care team for a comprehensive nutrition assessment.
2. ASPEN & Cleveland Clinic. Nutrition-Focused Physical Exam: An Illustrated Handbook American Society for Parenteral and Enteral Nutrition; 2016. 3. Mordarski, B, Wolff, J. Nutrition Focused Physical ExamPocket Guide. 2nd Edition. Academy of Nutrition and Dietetics; 2018. 4. Litchford M. Nutrition Focused Physical Assessment: Making Clinical .
USDA. Project Team Jane Duffield, MPA Supplemental Nutrition Assistance Program, Food and Nutrition Service, USDA Jackie Haven, MS, RDN Center for Nutrition Policy and Promotion, USDA Sarah A. Chang, MPH, RDN Center for Nutrition Policy and Promotion, USDA Maya Maroto, MPH, RDN Child Nutrition, USDA. Pilot Schools Thurgood Marshall Academy Public