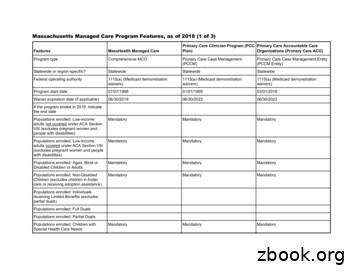
Massachusetts Managed Care Program Features, As Of 2018(1 .
Massachusetts Managed Care Program Features, as of 2018 (1 of 3)Primary Care Clinician Program (PCC Primary Care Accountable CarePlan)Organizations (Primary Care ACO)FeaturesMassHealth Managed CareProgram typeComprehensive MCOPrimary Care Case Management(PCCM)Primary Care Case Management Entity(PCCM Entity)Statewide or region-specific?StatewideStatewideStatewideFederal operating authority1115(a) (Medicaid demonstrationwaivers)1115(a) (Medicaid demonstrationwaivers)1115(a) (Medicaid demonstrationwaivers)Program start date07/07/199801/01/199503/01/2018Waiver expiration date (if ns enrolled: Low-incomeadults not covered under ACA SectionVIII (excludes pregnant women andpeople with s enrolled: Low-incomeadults covered under ACA Section VIII(excludes pregnant women and peoplewith s enrolled: Aged, Blind orDisabled Children or AdultsMandatoryMandatoryMandatoryPopulations enrolled: Non-DisabledChildren (excludes children in fostercare or receiving adoption datoryMandatoryIf the program ended in 2018, indicatethe end datePopulations enrolled: Individualsreceiving Limited Benefits (excludespartial duals)Populations enrolled: Full DualsPopulations enrolled: Partial DualsPopulations enrolled: Children withSpecial Health Care Needs1
FeaturesMassHealth Managed CarePrimary Care Clinician Program (PCC Primary Care Accountable CarePlan)Organizations (Primary Care ACO)Populations enrolled: NativeAmerican/Alaskan NativesMandatoryMandatoryMandatoryPopulations enrolled: Foster Care andAdoption Assistance ChildrenVoluntaryVoluntaryVoluntaryPopulations enrolled: Enrollment choice OtherperiodN/AOtherPopulations enrolled: Enrollment broker Maximusname (if applicable)MaximusMaximusPopulations enrolled: Notes onenrollment choice period14 days with a 90 day plan selectionperiod.Benefits covered: Inpatient hospitalphysical healthXBenefits covered: Inpatient hospitalbehavioral health (MH and/or SUD)XBenefits covered: Outpatient hospitalphysical healthXBenefits covered: Outpatient hospitalbehavioral health (MH and/or SUD)X14 daysBenefits covered: Partial hospitalization XBenefits covered: PhysicianXBenefits covered: Nurse practitionerXBenefits covered: Rural health clinicsand FQHCsXBenefits covered: Clinic servicesXBenefits covered: Lab and x-rayXBenefits covered: Prescription drugsXBenefits covered: Prosthetic devicesXBenefits covered: EPSDTXBenefits covered: Case managementXX2
FeaturesMassHealth Managed CarePrimary Care Clinician Program (PCC Primary Care Accountable CarePlan)Organizations (Primary Care ACO)Benefits covered: SSA Section 1945authorized health homeBenefits covered: Health home care(services in home)XBenefits covered: Family planningXBenefits covered: Dental services(medical/surgical)XBenefits covered: Dental (preventativeor corrective)Benefits covered: Personal care (stateplan option)XBenefits covered: HCBS waiver servicesBenefits covered: Private duty nursingBenefits covered: ICF-IDDBenefits covered: Nursing facilityservicesXBenefits covered: Hospice careXBenefits covered: Non-EmergencyMedical TransportationXBenefits covered: Institution for MentalDisease inpatient treatment for peopleages 21-64 defined by 42 CFR§438.6(e) as an 'in lieu of' benefitX3
Primary Care Clinician Program (PCC Primary Care Accountable CarePlan)Organizations (Primary Care ACO)FeaturesMassHealth Managed CareBenefits covered: Other (e.g., nursemidwife services, freestanding birthcenters, podiatry, etc.)Acupuncture, audiology, breast pump,chiropractic, diabetes self-managementtraining, dialysis, DME, earlyintervention, emergency services,fluoride varnish, hearing aids, infertilitydiagnosis, dentures, medical nutritiontherapy, orthotics, podiatry, radiologyand diagnostic tests, tobacco cessation,vision care, speech therapy,occupational therapy, physical therapy,SNF, chronic or rehab, othersQuality assurance and improvement:HEDIS data required?YesNoNoQuality assurance and improvement:CAHPS data required?YesNoNoQuality assurance and improvement:Accreditation required?YesNoNoQuality assurance and improvement:Accrediting organizationNCQAVoluntary participation in EQRperformance measure validationQuality assurance and improvement:EQRO contractor name (if applicable)Innovative Resource Group, LLC D/B/A Innovative Resource Group, LLC D/B/A Innovative Resource Group, LLC D/B/AKEPROKEPROKEPROPerformance incentives: Paymentbonuses/differentials to reward plansPerformance incentives: Preferentialauto-enrollment to reward plansXXPerformance incentives: MCOs/PHPsXrequired or encouraged to pay providersfor value/quality outcomesXPerformance incentives: Public reportscomparing plan performance on keymetricsPerformance incentives: Withholds tiedto performance metrics4
FeaturesMassHealth Managed CareParticipating plans: Plans in ProgramTufts Health Plan; Boston MedicalCenter Health PlanNotes: Program notesPrimary Care Clinician Program (PCC Primary Care Accountable CarePlan)Organizations (Primary Care ACO)Multiple Primary Care ProvidersCommunity Care Cooperative; PartnersHealthCare Choice; Steward HealthChoiceServices provided in this program arecovered by total cost of care rather thancapitation.5
Massachusetts Managed Care Program Features, as of 2018 (2 of 3)Program of All-Inclusive Care forthe Elderly (PACE)Accountable Care PartnershipPlansProgram typeProgram of All-inclusive Care for theElderly (PACE)Comprehensive MCOBehavioral Health Organization (BHO)only (PIHP and/or PAHP)Statewide or region-specific?Bristol, Essex, Franklin, Hampden,Hampshire, Middlesex, Norfolk,Plymouth, Suffolk, WorcestorStatewideStatewideFederal operating authorityPACE1115(a) (Medicaid demonstrationwaivers)1115(a) (Medicaid demonstrationwaivers)Program start 2022Populations enrolled: Low-incomeadults not covered under ACA SectionVIII (excludes pregnant women andpeople with disabilities)MandatoryMandatoryPopulations enrolled: Low-incomeadults covered under ACA Section VIII(excludes pregnant women andpeople with andatoryMandatoryFeaturesWaiver expiration date (if applicable)MassHealth BH/SUD PIHPIf the program ended in 2018, indicatethe end datePopulations enrolled: Aged, Blind orDisabled Children or AdultsVoluntaryPopulations enrolled: Non-DisabledChildren (excludes children in fostercare or receiving adoption assistance)Populations enrolled: Individualsreceiving Limited Benefits (excludespartial duals)Populations enrolled: Full DualsVoluntaryPopulations enrolled: Partial DualsVoluntaryPopulations enrolled: Children withSpecial Health Care NeedsMandatoryMandatoryMandatory6
FeaturesPopulations enrolled: NativeAmerican/Alaskan NativesProgram of All-Inclusive Care forthe Elderly (PACE)Accountable Care PartnershipPlansMassHealth BH/SUD therOtherMaximusMaximusPopulations enrolled: Foster Care andAdoption Assistance ChildrenPopulations enrolled: Enrollmentchoice periodN/APopulations enrolled: Enrollmentbroker name (if applicable)Populations enrolled: Notes onenrollment choice periodEnrollment open all year, effective the 14 days with 90 day plan selectionfirst day of the next month followingperiod.the date on which the member electsto enroll.Benefits covered: Inpatient hospitalphysical healthXXBenefits covered: Inpatient hospitalbehavioral health (MH and/or SUD)XXBenefits covered: Outpatient hospitalphysical healthXXBenefits covered: Outpatient hospitalbehavioral health (MH and/or SUD)XXXBenefits covered: PartialhospitalizationXXXBenefits covered: PhysicianXXXBenefits covered: Nurse practitionerXXXBenefits covered: Rural health clinicsand FQHCsXXBenefits covered: Clinic servicesXXBenefits covered: Lab and x-rayXXBenefits covered: Prescription drugsXXBenefits covered: Prosthetic devicesXXDailyXXX7
FeaturesProgram of All-Inclusive Care forthe Elderly (PACE)Benefits covered: EPSDTBenefits covered: Case managementAccountable Care PartnershipPlansMassHealth BH/SUD PIHPXXXBenefits covered: Health home care(services in home)XXBenefits covered: Family planningXXBenefits covered: Dental services(medical/surgical)XXXBenefits covered: SSA Section 1945authorized health homeBenefits covered: Dental (preventative Xor corrective)Benefits covered: Personal care (state Xplan option)Benefits covered: HCBS waiverservicesXBenefits covered: Private duty nursing XBenefits covered: ICF-IDDBenefits covered: Nursing facilityservicesXXBenefits covered: Hospice careXXBenefits covered: Non-EmergencyMedical TransportationXXBenefits covered: Institution for MentalDisease inpatient treatment for peopleages 21-64 defined by 42 CFR§438.6(e) as an 'in lieu of' benefitXX8
Program of All-Inclusive Care forthe Elderly (PACE)Accountable Care PartnershipPlansBenefits covered: Other (e.g., nursemidwife services, freestanding birthcenters, podiatry, etc.)The PACE program covers allmedically necessary services for theenrolled population, including but notlimited to all covered Medicare andMedicaid services.Acupuncture, audiology, breast pump,chiropractic, diabetes selfmanagement training, dialysis, DME,early intervention, emergencyservices, fluoride varnish, hearingaids, infertility diagnosis, dentures,medical nutrition therapy, orthotics,podiatry, radiology and diagnostictests, tobacco cessation, vision care,speech therapy, occupational therapy,physical therapy, SNF up to 100 daysper contract year, chronic or rehab,and Home Health (nursing andtherapies). LTSS are covered throughFFS. (Note: this list is not fullyinclusive).Children’s Behavioral Health Initiative(CBHI) services, Emergency ServicesProgram, and Diversionary Services:Community Crisis Stabilization,Community-Based Acute Treatmentfor Children and Adolescents (CBAT),Acute Treatment Services (ATS) forSubstance Use Disorders (Level III-7),Clinical Support Services (CSS) forSubstance Use Disorders (Level III.5),and Transitional Care Unit (TCU),Community Support Program (CSP),Partial Hospitalization, Psychiatric DayTreatment, Structure OutpatientAddiction Program (SOAP), Programof Assertive Community Treatment,and Intensive Outpatient Treatment,Transitional Support Services (TSSW)for Substance Use Disorders,Residential Rehabilitation Services forSubstance Use Disorder andEnhanced Residential RehabilitationServices for Dually Diagnosed.Quality assurance and improvement:HEDIS data required?NoYesYesQuality assurance and improvement:CAHPS data required?NoYesNoQuality assurance and improvement:Accreditation required?NoYesYesQuality assurance and improvement:Accrediting organizationNCQANCQAQuality assurance and improvement:EQRO contractor name (if applicable)Innovative Resource Group, LLCD/B/A KEPROInnovative Resource Group, DBAKEPROFeaturesPerformance incentives: Paymentbonuses/differentials to reward plansMassHealth BH/SUD PIHPX9
FeaturesProgram of All-Inclusive Care forthe Elderly (PACE)Accountable Care PartnershipPlansMassHealth BH/SUD PIHPXXPerformance incentives: Preferentialauto-enrollment to reward plansPerformance incentives: Public reportscomparing plan performance on keymetricsPerformance incentives: Withholdstied to performance metricsPerformance incentives: MCOs/PHPsrequired or encouraged to payproviders for value/quality outcomesParticipating plans: Plans in ProgramXElder Service Plan of CambridgeHealth Alliance; Upham's ElderService Plan; Elder Service Plan ofHarbor Health; Fallon Health SummitEldercare; Element Care Inc; SerenityCare PACE Program; Mercy Life Inc;Neighborhood PACEAtrius Health in partnership with Tufts Massachusetts Behavioral HealthPartnershipHealth Public Plans (THPP); BethIsrael Deaconess Care Organization(BIDCO) in partnership with TuftsHealth Public Plans (THPP); BostonChildren’s Health ACO in partnershipwith Tufts Health Public Plans (THPP);Cambridge Health Alliance (CHA) inpartnership with Tufts Health PublicPlans (THPP); Merrimack Valley ACOin partnership with AllWays HealthPartners; Boston Accountable CareOrganization in partnership with BMCHealthNet Plan; Mercy Medical Centerin partnership with BMC HealthNetPlan; Signature Healthcare inpartnership with BMC HealthNet Plan;Southcoast Health in partnership withBMC HealthNet Plan; HealthCollaborative of the Berkshires inpartnership with Fallon Health; ReliantMedical Group in partnership withFallon Health; Wellforce in partnershipwith Fallon Health; Baystate HealthCare Alliance in partnership withHealth New England10
FeaturesNotes: Program notesProgram of All-Inclusive Care forthe Elderly (PACE)Enrollment numbers do not includeprivate pay enrollees, if any.Accountable Care PartnershipPlansMassHealth BH/SUD PIHPFull duals are only enrolledmandatorily if less than 21 years ofage. The 1915(b) waiver providesmanaged behavioral health benefitsfor participants enrolled in the MFP-CLand MFP-RS 1915(c) waivers. Allother 1915(c) waiver HCBS areprovided on a fee-for-service basis.11
Massachusetts Managed Care Program Features, as of 2018 (3 of 3)FeaturesMoney Follows the PersonBehavioral Health Supports (MFPBH)Senior Care OptionsProgram typeBehavioral Health Organization (BHO)only (PIHP and/or PAHP)Comprehensive MCO MLTSSStatewide or region-specific?StatewideCounties of Barnstable, Bristol, Essex,Franklin, Hampden, Hampshire,Middlesex, Norfolk, Plymouth, Suffolk,Worcester and BerkshireFederal operating authority1915(b)/1915(c)1915(a)/1915(c)Program start date04/01/201307/01/2004Waiver expiration date (if applicable)03/31/201812/31/2018If the program ended in 2018, indicatethe end date03/31/2018Populations enrolled: Low-incomeadults not covered under ACA SectionVIII (excludes pregnant women andpeople with disabilities)MandatoryPopulations enrolled: Low-incomeadults covered under ACA Section VIII(excludes pregnant women and peoplewith disabilities)MandatoryPopulations enrolled: Aged, Blind orDisabled Children or AdultsMandatoryVoluntaryPopulations enrolled: Full DualsMandatoryVoluntaryPopulations enrolled: Partial DualsMandatoryVoluntaryPopulations enrolled: Non-DisabledChildren (excludes children in fostercare or receiving adoption assistance)Populations enrolled: Individualsreceiving Limited Benefits (excludespartial duals)12
Money Follows the PersonBehavioral Health Supports (MFPBH)Senior Care OptionsPopulations enrolled: NativeAmerican/Alaskan NativesMandatoryVoluntaryPopulations enrolled: Foster Care andAdoption Assistance ChildrenExemptFeaturesPopulations enrolled: Children withSpecial Health Care NeedsPopulations enrolled: Enrollment choiceperiodOtherPopulations enrolled: Enrollment brokername (if applicable)Populations enrolled: Notes onenrollment choice periodMedicaid members are eligible to enrollall year, with enrollment effective thefirst day of the month following themonth in which the member decided toenroll. Dual eligible members areeligible to enroll in accordance with theMedicare Advantage enrollment period,with enrollment effective the first day ofthe month following the month in whichthe member decided to enroll.Benefits covered: Inpatient hospitalphysical healthXBenefits covered: Inpatient hospitalbehavioral health (MH and/or SUD)XBenefits covered: Outpatient hospitalphysical healthBenefits covered: Outpatient hospitalbehavioral health (MH and/or SUD)XXXXBenefits covered: Partial hospitalization XXBenefits covered: PhysicianXBenefits covered: Nurse practitionerX13
FeaturesMoney Follows the PersonBehavioral Health Supports (MFPBH)Benefits covered: Rural health clinicsand FQHCsBenefits covered: Clinic servicesSenior Care OptionsXXXBenefits covered: Lab and x-rayXBenefits covered: Prescription drugsXBenefits covered: Prosthetic devicesXBenefits covered: EPSDTBenefits covered: Case managementXXBenefits covered: SSA Section 1945authorized health homeBenefits covered: Health home care(services in home)XBenefits covered: Family planningXBenefits covered: Dental services(medical/surgical)XBenefits covered: Dental (preventativeor corrective)XBenefits covered: Personal care (stateplan option)XBenefits covered: HCBS waiver servicesXBenefits covered: Private duty nursingXBenefits covered: ICF-IDDBenefits covered: Nursing facilityservicesXBenefits covered: Hospice careXBenefits covered: Non-EmergencyMedical TransportationX14
FeaturesMoney Follows the PersonBehavioral Health Supports (MFPBH)Senior Care OptionsBenefits covered: Institution for MentalDisease inpatient treatment for peopleages 21-64 defined by 42 CFR§438.6(e) as an 'in lieu of' benefitBenefits covered: Other (e.g., nursemidwife services, freestanding birthcenters, podiatry, etc.)Emergency Services Program andDiversionary Services, CommunityCrisis Stabilization, Acute TreatmentServices (ATS) for Substance UseDisorders (Level III-7), Clinical SupportServices (CSS) for Substance UseDisorders (Level III-5) and TransitionalCare Unit (TCU), Community SupportProgram (CSP), Partial Hospitalization,Partial Psychiatric Day Treatment,Structure Outpatient Addiction Program(SOAP), Program of AssertiveCommunity Treatment and IntensiveOutpatient TreatmentAll MassHealth covered LTSS and allservices described in theCommonwealth 1915(c) Frail ElderWaiverQuality assurance and improvement:HEDIS data required?NoYesQuality assurance and improvement:CAHPS data required?NoYesQuality assurance and improvement:Accreditation required?NoNoQuality assurance and improvement:Accrediting organizationQuality assurance and improvement:EQRO contractor name (if applicable)KEPROPerformance incentives: Paymentbonuses/differentials to reward plansPerformance incentives: Preferentialauto-enrollment to reward plans15
FeaturesMoney Follows the PersonBehavioral Health Supports (MFPBH)Performance incentives: Public reportscomparing plan performance on keymetricsSenior Care OptionsXPerformance incentives: Withholds tiedto performance metricsPerformance incentives: MCOs/PHPsrequired or encouraged to pay providersfor value/quality outcomesParticipating plans: Plans in ProgramMoney Follows the Person- BehavioralHealth Supports (MFP-BH)Boston Medical Center Healthnet Plan;Commonwealth Care Alliance; NavicareHMO; Senior Whole Health; TuftsHealth Plan; United HealthcareNotes: Program notesMassHealth members enrolled in thetwo 1915(c) MFP Waivers who are nototherwise eligible for the 1115demonstration were mandatorilyenrolled in this 1915(b) Waiver. The1915(c) waivers included both the MFPCommunity Living (MFP-CL, waivercontrol number MA.1027) and the MFPResidential Supports (MFP-RS, waivercontrol number MA.1028) Waivers. TheMFP-BH Waiver (MFP-BH, waivercontrol number MA.0002) ranconcurrently with these 1915(c) waivers.MFP waiver participants must be age18-64 with disabilities or age 65 or overand must be on MassHealth Standard.The SCO Program is a voluntaryprogram offered to MassHealthmembers age 65 and older residing inthe service area of a Senior CareOganization. The SCO program isavailable in 12 of the 14 counties inMassachusetts. The SCO programcovers all medically necessary Medicaidand Medicare covered services throughits provider network. Each enrolleeselects a PCP upon enrollment,receives care coordination, andparticipates in and signs off on thedevelopment of his/her care plan. EachSenior Care Organization is alsodesignated by CMS as a MedicareAdvantage Special Needs Plan forindividuals dually eligible for Medicareand Medicaid.16
Southcoast Health in partnership with BMC HealthNet Plan; Health Collaborative of the Berkshires in partnership with Fallon Health; Reliant Medical Group in partnership with Fallon Health; Wellforce in partnership with Fallon Health; Baystate Health Care Alliance in partnership with Health New England : Massachusetts Behavioral Health Partnership
Managed Care 101 Medicaid, Managed Care, and Children More than 70% of Medicaid beneficiaries are enrolled in private managed care organizations (MCOs) Almost 9 of every 10 children enrolled in Medicaid and CHIP receive health care through a managed care arrangement 39 states rely on MCOs to cover all or some of their Medicaid
population is served by managed care. Per RCW 74.09.522, "The Legislature finds that competition in the managed health care marketplace is enhanced, in the long term, by the existence of a large number of managed health care system options for Medicaid clients. In a managed care delivery system, whose goal is to focus on prevention, primary
program, Statewide Medicaid Managed Care (SMMC) (Part IV of Chapter 409, Florida Statutes). Statewide Medicaid Managed Care has two program components: Long Term Care Managed Care Program oImplementation begins 7/1/12 with release of ITN oCertain recipients will be required to e
Florida’s proposal to provide Medicaid long-term services and supports (LTSS) through managed care. As is generally the case in Medicaid managed care, Florida’s move to managed care is being promoted by the state as a way to provide care in a more coordinated fashion, but in practice may limit access to care
services through managed care.1 Medicaid managed care programs provide a wide array of acute health care services (primary, specialty and behavioral health care, pharmacy, dental and diagnostic services) and LTSS (nursing, home health care, therapy services, home and community-based services, nursing facility and attendant care).
C h a p t e r 1 Salesforce Managed Package This chapter includes the following topics: Salesforce Managed Package Overview, 5 Salesforce Managed Package URLs, 5 Installing the Managed Package, 6 Uninstalling and Deleting the Managed Package, 9 More Information, 10 Salesforce Managed Package Overview You need the Informatica Cloud Real Time for Salesforce package (the .
Apr 01, 2019 · same time on February 2, 2019, the Managed Care Plan would submit one attestation listing all five reports being submitted. If a Managed Care Plan is submitting one weekly report on February 2, 2019, and four quarterly reports on February 3, 2019, a separate a
Managed Care Services Agreement CONTRACT TO PROVIDE MANAGED CARE SERVICES FOR THE MEDICAID and FAMILY ACCESS TO MEDICAL INSURANCE SECURITY (FAMIS) PROGRAMS JULY 1, 2020 - JUNE 30, 2021 . Medallion 4.0 Managed Care Contract SFY21v3 2 CONTENTS