Neuro-Ophthalmology: Case After Case Neuro-Ophthalmology .
Neuro-Ophthalmology: Case After Case Neuro-Ophthalmology: Case After Case Nancy J. Newman, MDValérie Biousse, MDEmory University School of Medicine, Atlanta, GANancy J. Newman, MDValérie Biousse, MDEmory University School of Medicine, Atlanta, GA Disclosures:––––Consultant for Gensight, Santhera and StealthResearch support: Gensight, Santhera and NIHData Safety Committee: Quark NAION clinical trialMost illustrations are from Neuro-Ophthalmology Illustrated, Thieme 2019.3rd edition1219 yo woman with visual loss19 yo woman with visual loss Past medical history: Obese Meds: None No tobacco, no alcohol Past 2 weeks:– severe headaches– Rapidly progressive visual loss OU– Diplopia Family history: Unremarkable34Extraocular Movements:Abduction deficit / EsotropiaExaminationVisual acuityColor visionSLE/IOPPupilsLids5Right eyeLeft eye20/3013/14NormalNo RAPDNormal20/2014/14NormalNo RAPDNormal61
Visual field testing Blood pressure 118/66What next?78She needs Send her to Emergency Department In hospital with:– Neurology– Neurosurgery– Neuroradiology– Available 24/7– And Neuro-ophthalmologistNeurologic examinationGeneral examinationBlood pressureBrain MRI with GadoliniumBrain MRV with GadoliniumLumbar puncture if imaging normal Immediately9 Warn Neuro-Ophthalmologist and ED10EvaluationFulminant Idiopathic Intracranial Hypertension Normal neurologic examinationBlood pressure: 122/72Brain MRI with Gadolinium: NormalBrain MRV: Normal (signs of raised ICP)Lumbar puncture:– Opening pressure: 63 cm H2O– Normal CSF contents No anemia, no sleep apnea, no medications11 Acetazolamide 500 mg bid Dramatic improvement of headaches and diplopiaafter lumbar puncture Consult Neurosurgery122
Fulminant Idiopathic Intracranial HypertensionExamination 1 week later 12 hours later: recurrence of headaches and diplopiaVAColor visionSLE/IOPPupilsEOMs– VA: 20/400 right eye, 20/50 left eye– Lumbar drain Lumbo-peritoneal shunt next day13141516Right eyeLeft eye20/5014/14NormalNo RAPDFull20/4014/14NormalNo RAPDFullBilateral Disc Edema (headache)Idiopathic Intracranial HypertensionBrain imaging (contrast)(Normal CT MRI/MRV)-Hydrocephalus-Mass-Venous thrombosisNl CSF OPNl CSFNo RaisedICPPseudo DE17 NormalHeadachesPapilledema Diplopia (VIth) TinnitusMRI rules out intracranial process andvenous thrombosisLumbar puncture confirms high CSF OPand normal CSF contents LPPressure 25cmH2ONl CSFIsolated intracranial hypertensionAbnl CSF -Meningitis-Spinal cordAlwaysreconsider cerebral“Idiopathic”tumorvenous thrombosisintracranialhypertension (IIH) 183
Idiopathic Intracranial HypertensionIdiopathic Intracranial HypertensionEvaluationManagement Severity of headaches Diplopia Visual function Prognosis Rapid onset Patient’s characteristics Severe obesity, black race, male gender Anemia / sleep apnea syndrome / HTN Visualfunction Visual acuity, color vision Visual field (automated perimetry, Goldmannperimetry)1920Raised ICP and PapilledemaVisual Field Testing21Raised ICP and PapilledemaVisual Field Testing22Raised ICP and PapilledemaVisual Field Testing23244
Idiopathic Intracranial HypertensionIdiopathic Intracranial HypertensionFollowup/Treatment (1-2 weeks)Management Follow-up/Treatment Lumbar puncture(1st treatment) CorrectTreatment efficacyVisual function (visual field)Improvementprecipitation factors Drug, anemia, sleep apnea, Followup (1-2 mo) Weightloss (long term) Acetazolamide (1-3 grams/day)Followup (3 mos)Followup (6 mos)25No improvementWorsening-Repeat LP/drain-Surgery ?-Venous stenting?26Optic Neuritis:Is It or Isn’t It ?A 39 y/o man with visual loss right eyePast Medical History: hypertension, cigsNancy J. Newman, M.D.Medications: atenololEmory University School of MedicineAtlanta GA27Family History: Unremarkable28Examination:5 weeks ago:- progressive, painless visual loss ODover 4-5 daysVision:Color:Orbits:SLE:IOPs:Pupils:No previous visual loss or neurologicsymptomsNo rmalNormal1414Pharmacologically Dilated305
3132Optic NeuritisIs It Optic Neuritis?Typical Idiopathic Macular disease A different cause of optic neuropathy33 34Optic NeuritisMimickersSexPainFieldPupilFundus Macular disease35Inflammation of the optic nerveF:M 3:1Age: 15-45Pain on eye movementNormal or swollen discSpontaneous improvementAssociated with multiple sclerosisOptic NeuritisFemaleYesCentralRAPDNerve nl/edemaCSRMaleNoCentralNo RAPDBlister366
SexPainFieldPupilFundusOptic NeuritisFemaleYesCentralRAPDNerve nl/edemaCSRMaleNoCentralNo alNo RAPDBlister38Optic NeuropathyIs It Optic Neuritis?Causes Inflammatory Vascular Compressive/Infiltrative Hereditary Toxic/Nutritional Traumatic Elevated intracranial pressure Elevated intraocular pressure A different cause of optic neuropathy3940Optic NeuritisOptic NeuritisMimickersDDx Inflammatory Vascular Compressive/Infiltrative Hereditary Toxic/Nutritional Traumatic Elevated intracranial pressure Elevated intraocular pressure41Optic NeuritisFemaleYesCentralRAPDNerve nl/edema Anterior ischemic optic neuropathyCompressive optic neuropathyLeber hereditary optic neuropathyOther inflammatory/infectious optic neuritis427
Optic ltitudinalNerve nl/edema Nerve edemaNerve enhancesNerve nlImprovesNo changeSexAgePainFieldFundusMRICourse4344Optic Neuritis Leber HONMaleNoCentralYesSevere lossNerve nlPseudoedemaOp rseImprovesMRINerve enhancesFundusNerve nl/edema45NAIONCompressiveLeber HONAgeYoungerOlderAnyYoungerGenderF MM FM FM FFam HxNo or MSNoNoYesBilateral? 10% at 1yr 10% at 1yrNo100% at 1yrOnsetRapidSlowSubacutePain? (w EOM) RareNoNoColorPoorRapidOften spared PoorPoorVisual Field CentralAltitudinalCentral/tempCecocentralOptic Nerve N /edemaEdemaNl/edemaNl/pseudoMRIAbnl ONNormalTumorNormalPrognosisGoodPoorPoor (if no Rx) PoorSystemicMSHTN/DMNoneNone46Op Neuritis47Optic Neuritis al/TemporalNerve nl/edema Nerve nl/edemaNerve enhances Nerve rseNAIONCompressiveYoungerOlderAnyYoungerGenderF MM FM FM FFam HxNo or MSNoNoYesBilateral? 10% at 1yr 10% at 1yrNo100% at 1yrOnsetRapidSlowSubacutePain? (w EOM) RareNoNoColorPoorRapidOptic NeuritisLeber HONAgeOften spared PoorPoorVisual Field CentralAltitudinalCentral/tempCecocentralOptic Nerve N /edemaEdemaNl/edemaNl/pseudoMRIAbnl ONNormalTumorNormalPrognosisGoodPoorPoor (if no Rx) PoorSystemicMSHTN/DMNoneTypical Idiopathic NoneInflammation of the optic nerveF:M 3:1Age: 15-45Pain on eye movementNormal or swollen discSpontaneous improvementAssociated with multiple sclerosis488
Atypical Optic Neuritis BilateralIntra-ocular cellsDisc swellingHemorrhagesExudates (“star”) ypical Optic Neuritis AQP4 (NMO) Abs MOG Abs50A 39 y/o man with painless visual loss OD to20/200 over 5 days, past history of HTN,no family history of visual loss, and noimprovement over the past 5 weeks.A 39 y/o man with painless visual loss OD to20/200 over 5 days, past history of HTN,no family history of visual loss, and noimprovement over the past 5 weeks. Normal maculaRight RAPDNormal MRI orbits/brain with contrastNo vision recovery OD and no vision lossOS for 1 year51Normal maculaRight RAPDNormal MRI orbits/brain with contrastNo vision recovery OD and no vision lossOS for 1 year52 37-yo woman with visual loss OS Visual loss OS: Central shadow Progression over 5 days Pain with eye movements PMHx: 2 normal pregnancies 2 abortions No associated neurologic or systemicsymptoms Fam Hx: Unremarkable53BilateralSevereNo recoveryRecurrent549
ExaminationExamination BP: 116/74, RR 67 Neurologic examination normal VA Color Orbits Lids IOP SLE Pupils ount FingersNo controlNormalNormal15Normal RAPDFull56Visual FieldsFundus5758Diagnosis ?What next ? Optic neuropathy OS Retrobulbar Inflammatory Refer « Idiopathic optic neuritis »-59-6010
Work-upBrain MRI Negative syphilis testing Normal ACE Negative AQP4/MOG antibodies6162Management-Follow-up: 6 weeks later 3 days IV methylprednisolone (250 mgq6 hours) 10 days oral prednisone (taper)63 /14NormalNormal15Normal RAPDFull64Follow-up: 6 weeks later65VAColorOrbitsLidsIOPSLEPupilsEOMFollow-up: 6 weeks later6611
Patient’s Questions What next ? Are you sure it is an optic neuritis? Is it idiopathic demyelinating opticneuritis? Do I have MS ? What is my risk of MS ? How should I be treated ? Refer-6768HPI51 yo woman with visual loss in left eyePMHx: Breast cancer 11 years prior (lumpectomy, radiation,chemotherapy, neg lymph nodes) Hypertension, borderline diabetes Migraine headaches (no aura) Medications: Hydrochlorothiazide, aspirin 81, vitamins, ibuprofen prnFollowed by neurologist for episodes of tingling of both legsand occasionally left arm shaking Normal brain MRI Scheduled for electromyography Saw optometrist for annual visit: Decreased vision left eye Left optic nerve pallor “Left optic neuritis” 6970Neuro-Ophthalmology 71Neurologist: Cancelled electromyography Repeated brain MRI (normal) Planned LP for possible multiple sclerosis BP: 148/92. BMI 32Visual acuity Color vision Slit lamp IOP Pupils Eye movements Patient: Panicked Refused LP Second opinionRight eye20/2014/14Mild cataracts12NormalFullLeft eye20/403/1413RAPD Full7212
Humphrey Visual FieldsFundus ExaminationLeft eyeRight eye73Right eyeLeft eye74DiagnosisReview MRILeft optic neuropathy (chronic)Incidentally found No pain 7576With contrast777813
MRI Orbits with Contrastand Fat SuppressionMRI Orbits with ContrastLeft Optic Nerve Sheath Meningioma7980 20-yo WM with visual loss in both eyes Age 8: told he had « swelling OU »during routine examination Asymptomatic Observed yearly, without change PMHx Unremarkable Fam Hx: Unremarkable College student – no ETOH or drugs8182 Age 20 (8 months prior seeing us) Sudden, painless visual loss OS MRI brain/orbits: normal CBC, bartonella, toxo, RPR, FTA:normal or negative VA: 20/20 OD; 20/200 OS “Swelling” OS838414
3 months later: Repeat MRI: normal « More blood tests » : all normal Lumbar puncture: OP: 16 cm CSF contents: normal Visual loss OD VA: 20/100 OD; CF OS8586Examination 2 months later VA Col Vis Orbit Lid IOP SLE Pupils EOMODOSCFNo controlNormalNormal14NormalNormalFullCFNo controlNormalNormal15Normal1.2 RAPDFull87Goldmann Visual Fields-88FundusWork-up Leber’s hereditary optic neuropathy: 3 primary mutations: mt DNA 11778 mt DNA 14484 mt DNA 3460 Negative-899015
Leber’s Hereditary Optic NeuropathyWork-up Blood sent to lab with expertise in LHON Complete sequencing of mtDNA 10 mutations found Including, novel mtDNA mutation atnp 12848 (heteroplasmic) Alters complex 1 Subacute sequential bilateral central visual lossAge of onset typically 18-30 (range 1-87)Male predominance (80-90%)Progression in each eye over weeks to monthsRecognized interval between eyes in 50%(days to months) 97% bilateral within 1 year-9192Leber’s Hereditary Optic Neuropathy Acuity usually worse than 20/200 Color vision affected early Central or cecocentral defects9394 95Leber’s Hereditary Optic NeuropathyLeber’s Hereditary Optic NeuropathySpontaneous RecoveryAssociated FindingsMay occur years later4% - 71%Depends on the mtDNA mutationMore likely if visual loss before age 20 (esp 10) Cardiac conduction defectsMinor neurologic abnormalitiesMultiple sclerosis-like illnessMore severe neurologic syndromes9616
14841?Leber Hereditary Optic Neuropathy14598*14502*Determinants of Phenotype Genotype–the mutation–heteroplasmy MtDNA factors Nuclear factors Environmental factors10680?10197*d9798Hereditary Optic NeuropathiesMitochondrial DiseasesSymptomatic TreatmentTreatment Improve quality of life: reading, navigating,communication, employment, driving Low-vision aids Avoid mitochondrial toxicity: Tobacco use ? Heavy alcohol use Meds with mitochondrial toxicity Environmental toxins Genetic counseling Symptomatic Disease-modifying Mitochondrial diseases Hereditary optic neuropathies Idebenone (900mg/d) (ongoing clinical trial) Gene therapy (ongoing clinical trials)99100Hereditary Optic NeuropathiesMtDNA Mitochondrial DisordersTreatmentTreatment – Nuclear Transfer Genetic counseling Symptomatic Disease-modifying Mitochondrial diseases Hereditary optic neuropathies Idebenone (900mg/d) (ongoing clinical trial) Gene therapy (ongoing clinical trials)101 Oocyte nuclear spindle replacement Pronuclear transfer between zygotesMutant mtDNAIn vitro fertilizationWild type mtDNA(Tachibana M, et al. Nature 2009;461:367-372)(Craven L, et al. Nature 2010;465:82-85)10217
Leber Hereditary Optic NeuropathyTreatment Ideal “laboratory” for testing treatment efficacy Sequential visual loss: therapeutic window Accessibility via topical or intravitreal route Implications for other optic neuropathies103104Leber Hereditary Optic NeuropathyTreatment – Gene TherapyDifferent patient inclusion criteria Allotopic RescueOnset of vision lossREVERSE 6 months to 1 yr37 patientsFully enrolled Feb 2017Same design One eye randomized toGS010; other eye receivedsham injection; “best” eyetreated half the timeGroup 1Same endpoints at Week 48Primary Mean difference change frombaseline, ETDRS letters, drugtreated eyes vs. sham treated eyes(LogMAR)SecondaryRESCUEOnset of vision loss 6 months39 patientsFully enrolled July 2017GS010in right eyeSHAM inleft eyeGroup 2GS010in left eyeSHAMin right eye105 SD-OCT, visual field, color andcontrast vision Responder analysis:o Gain from baseline of 15 ETDRSletterso Snellen acuity 20/200 Treat
–Most illustrations are from Neuro-Ophthalmology Illustrated, Thieme 2019. 3rd edition Neuro-Ophthalmology: Case After Case Nancy J. Newman, MD Valérie Biousse, MD Emory University School of Medicine, Atlanta, GA 19 yo woman with visual loss Past medical history: Obese Meds: None No tobacco, no alcohol Family history: Unremarkable
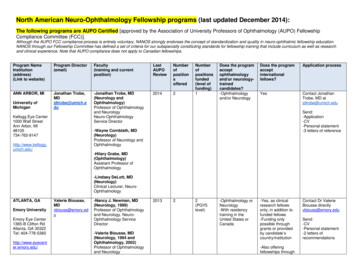
ophthalmology.html #neuro Rudrani Banik, rbanik@nyee.edu Rudrani Banik, M.D. Contact Dr. Rudrani (Ophthalmology 2001) Associate Professor of Ophthalmology (Neurology 1978 and Ophthalmology 1980) Professor of Ophthalmology and Neurology 2014 1 -Ophthalmology or Neurology -With residency
Pediatric Ophthalmology, Neuro-Ophthalmology,Genetics Cornea and External Eye Disease. Editors B. Lorenz A.T.Moore With 89 Figures,Mostly in Color, and 25 Tables Pediatric Ophthalmology, Neuro-Ophthalmology, Genetics 123. Series Editors Guenter K.Krieglstein,MD Professor and Chairman
October 2016. We considered 8 subspecialties of ophthalmology in this study: comprehensive ophthalmology, retina/vitreous, pediatric ophthalmology, cornea/external disease, glaucoma, oculoplastics, neuro-ophthalmology, and uveitis. Comprehensive ophthalmology is the broadest clinical area and includes everything from complete eye
Medical Director, NYEE-West Palm Beach An Unprecedented Look at Acute Solar Retinopathy Michelle Rhee, MD Associate Director of Ophthalmology, Elmhurst Hospital Neuro-Ophthalmology Mark Kupersmith, MD System Chief, Neuro-Ophthalmology, MSHS Valerie Elmalem, MD Joel Mindel, MD Ocular Oncology Paul Finger, MD Ophthalmic Pathology
3 Comprehensive Ophthalmology A.K Khurana 5th edition Reference books 1 Kanski’s linical Ophthalmology Brad Bowling 8th Edition 2 Oxford handbook of Ophthalmology 3rd Edition 3 For Clinical methods visit Chua Website www.mrcophth.com The marks allotted for your Ophthalmology paper in the 4th Professional MBBS exam are as under:
61 MD (Ophthalmology) Dr. Sahil Agarwal P-2015/13963 62 MD (Ophthalmology) Dr. Divya Kumari P-2015/13964 63 MD (Ophthalmology) Dr. Karthikeyan M P-2015/13965 64 MD (Ophthalmology) Dr. Dhanawath Naveen Rathod P-2015/13967 65 MD (Ophthalmology) Dr. Suresh Azimeera P-2015/13968
Clinical Ophthalmology by Shafi M. Jatoi Basic Ophthalmology by Renu Jogi Kanski [s Clinical Ophthalmology by Brad Bowling Anatomy of Eye Ophthalmology by Richard S. Snell Parsons Eye Disease TABLE OF SPECIFICATIONS EYE (PRE-ANNUAL/ANNUAL IV PROFESSIONAL EXAMAMINATION: THEORY): Time Allowed 03 hrs. (In
ANsi A300 (Part 9) and isA bMP as they outline how risk tolerance affects risk rating, from fieldwork to legal defense, and we wanted to take that into account for the Unitil specification. The definitions and applications of the following items were detailed: