NHS
NHSEImproving QualityFirst steps towards quality improvement:A simple guide to improving services
IMPROVEMENT. PEOPLE. QUALITY. STAFF. DATA.STEPS. LEAN. PATIENTS. PRODUCTIVITY. IDEAS.REDESIGN. MAPPING. SOLUTIONS. EXPERIENCE.SHARE. PROCESSES. TOOLS. MEASURES.INVOLVEMENT. STRENGTH. SUPPORT. LEARN.CHANGE. TEST. IMPLEMENT. PREPARATION.KNOW-HOW. SCOPE. INNOVATION. FOCUS.ENGAGEMENT. DELIVERY. DIAGNOSIS. LAUNCH.RESOURCES. EVALUATION. NHS. PLANNING.TECHNIQUES. FRAMEWORK. AGREEMENT.UNDERSTAND. IMPLEMENTATION. SUSTAIN.
FIRST STE PS T OWARDS QU AL IT Y I MP RO VE ME N T: A S I MP L E G U I D E T O I MP RO VI N G S E R VI C E SCONTENTS4Introduction6Chapter 18Chapter 2- Improvement models- Defining the change idea and developing aims11 Chapter 3- Managing a successful project14 Chapter 4- Levers and drivers – framing the work for a wider audience16 Chapter 5- Getting the right people involved18 Chapter 6- Involving patients and carers in service redesign22 Chapter 7- Communicating the right things to the right people24 Chapter 8- Improvement tool: Process mapping28 Chapter 9- Improvement tool: Plan, do, study, act cycles30 Chapter 10 - Measuring your efforts34 Chapter 11 - Improvement tool: Using statistical process control charts37 Chapter 12 - Human dimensions of change40 Chapter 13 - Sharing your success44 Acknowledgements2/3
FIRST STE PS T OWARDS QU AL IT Y I MP RO VE ME N T: A S I MP L E G U I D E T O I MP RO VI N G S E R VI C E SINTRODUCTIONIf you are involved at any level in improving health orBefore implementing a solution and changing your service, it issocial care, this resource will provide the informationessential to understand your current system by mapping theyou need for your first steps towards making qualityprocess, collecting and analysing the service data, along withimprovements, giving your improvement project theasking patients and staff for their views, in order to determinebest possible chance of success.where improvements can be made. Don’t rush intoimplementing whole system changes without testing andWhether you are experienced at running improvementmeasuring small incremental changes. Learn from experienceprojects or not, this blend of project management andand be prepared to be flexible as your first idea may not be theimprovement tools, combined with practical know-howbest or the right solution.and first hand experience gained from working with NHSteams, should prove invaluable.This resource is not intended as a complete guide but provides ashort overview with the most relevant tools and other resourcessignposted for further exploration.If you want to deliver sustainable improvements with greaterspeed and confidence, this resource will help you take the firststeps.
“ Every system isperfectly designedto get the results itachieves”Paul Batalden4/5
FIRST STE PS T OWARD S Q UA LI TY IM P ROVE M E NT: A S I MP L E G UI D E T O I MP RO VI N G S E R VI C E SDo I really need a model toimprove things?CHAPTER 1Improvement modelsThere are many models which can supportyour improvement project; however, wepromote two such models: a five stepapproach to successfully manage thechange project from initial concept tocompletion, and the Model for Improvementto provide a framework for developing,testing and implementing changes.understanding what you are going toaccomplish, identifying a core team toundertake the work and a team to supportthe direction of the work along withidentifying patients and carers to beinvolved. Work should be aligned to bothlocal and national objectives together withstructured plans to measure improvements.Five step improvement approachA five step improvement approach has beendefined to provide a systematic frameworkfrom the beginning to the end of yourimprovement project which will give yourproject a greater chance of sustainablesuccess.The launch phase is the official start of theproject. The team should be formed; projectplans, communication plans and datacollection plans should be in place and anexecutive sponsor identified to support theproject. The preparation phase incorporateseverything you need to do before theofficial start of your project. This includesdefining your project aims and objectives,collecting baseline data for your service,The diagnosis phase is aboutunderstanding the current process,dispelling assumptions, using data to definethe problem and to build upon the baselinedata.The implementation phase tests andmeasures potential solutions using a plan,do, study, act (PDSA) cycle (chapter 9),implements the best solution and introducesstandard work and mistake proofing for aquality sustainable process.Very often, it is clear that we need toget on and improve things and youmay be tempted to leap in and do so.However, a very high proportion ofprojects fail, and one way to increasethe chances of your own projectsucceeding is to adopt a moresystematic, tried and tested approachsuch as those outlined on this page.Quality improvement requires the will,the ideas and the execution of thoseideas to succeed – very often, we havethe will to make things happen, but byusing models such as these, we canensure we develop the best possiblechange ideas and approachimplementation in a planned andsystematic way to enhance ourchances of success.The final phase is evaluation whereachievements are celebrated, learning andprinciples are captured and the improvementbecomes the norm.
Model for ImprovementWhat are we trying to accomplish?How will we know that achange is an improvement?What changes can we make that willresult in the improvements that we seek?ACTSTUDYThe framework, which was developed by ateam at the Institute for HealthcareImprovement in the USA, includes three keyquestions to ask before embarking on achange programme, supported by a processfor testing change ideas using plan, do,study, act (PDSA) cycles.PLANDOThe Model for ImprovementThe model for improvement is incorporatedinto the five step approach and wasdesigned to provide a framework fordeveloping, testing and implementingchanges that lead to improvement. Toachieve improvements we need to take thetime to plan change and test it out andresist the temptation to rush into wholesalechanges to systems. This way, we will knowwhat is working well, and what is not sosuccessful. Small scale changes can beundone and replaced by alternative ideas.6/7The sum of all of the change ideas that aretested and successfully implemented will bethe effective redesign of processes or waysof working.What are we trying to accomplish? Clear and focused goals that focus onproblems that cause concern for patientsand staff Consistent with local and nationaloutcomes, plans and frameworks Bold and aspirational With clear numerical targets.How will we know if a change is animprovement? What can we measure that will change ifthe system is improved? How can we obtain this data? Is itavailable in existing information systems,or will we need to collect this manually? What is the best way to display the datawe collect so that we can decide whetherwe are improving the system and whetherthe improvement is sustainable? Measure the baseline – how is the processor system performing before the changeis made? Measure regularly during testing – what isthe impact immediately, and what is theimpact over a period of time? Continue to measure after theimprovement is implemented, to ensurethat the change is sustained.What changes can we make that willresult in improvement? Many change ideas are generated atprocess mapping events (See Chapter 8) Use techniques of creative thinking andinnovation to generate ideas and to sortthem into those to be tested Learn from your colleagues – we knowthat there are many examples of goodpractice currently available.The Model for Improvement is a tried andtested approach for implementing anyaspect of change in health services. Addressthe three questions before embarking onservice redesign, to keep the work focusedand relevant and to ensure that you canmeasure the impact of changing the system.Use PDSA cycles (chapter 9) to test out ideason a small scale and to win commitmentbefore implementing changes across wholedepartments, processes and systems.Further explanation of the Five StepApproach and Model for Improvement isdetailed in later chapters.
FIRST STE PS T OWARD S Q UA LI TY IM P ROVE M E NT: A S I MP L E G UI D E T O I MP RO VI N G S E R VI C E SWhat is the purpose of a clear aimor objective?CHAPTER 2Defining the change idea anddeveloping aimsA clear and accurate project definition is oneof the most important tasks to ensure thesuccess of any improvement project.When starting out, begin by focusing on theproblem you are trying to solve, rather thana solution you are trying to implement - noone likes change for change sake!Analyse the problem by talking and listeningto those involved, collect baseline data andrecognise the impact of not changinganything at all. Once you have a clearunderstanding of the problem, it is vital toobtain agreement and support from thoseinvolved as you will find that differentpeople have different knowledge based ontheir past experiences. Agreement will alsoincrease team engagement and will providea stable platform to take the next step indeveloping the scope of your project withfocused aims and objectives.Project scopeWhen defining your change idea, take timeto consider and clearly document what iswithin the scope of your project as well aswhat is out of scope.Examples of poorly written project aimsWe will improve cancer servicesThis aim doesn’t clearly state what thechange will actually improve and who wouldbe responsible in improving the services. Arethe improvements for every cancer patientor just patients with certain types of cancer(e.g. breast cancer) or for all types of cancersfor a specific group of patients (e.g. childrenand young people)? The project aim muststipulate how much the service is going tobe improved, when it is going to becompleted and what is the impact of theimprovement.To ensure everyone is workingtowards the same goal and everyonehas the same expectations. It isimportant to define this clearly, sothat you can also identify what it isrelevant to measure and to help avoidproject creep as your work progresses.A good aim statement can help tomotivate people about your project asbeing something worthwhile,measurable and achievable.“ If you don’t know whereyou are going, you arelikely to end upsomewhere else!”Yogi Berra
The scope should include information aboutthe project boundaries and key deliverables.However, be cautious of the size of theproject scope. A large wide ranging projectscope may mean the work does not haveenough focus or detail, or may achieve verylittle by trying to do too much; whereas anarrow focused scope may lead to a projectthat does not make a significant differenceand cannot be transferable or able to scaleup.A well defined project scope is critical toprevent a project creeping out of control.‘Project creep’ is when the scope of a projectgrows from its original parameters intosomething more or different from theoriginal intention. Implications of achanging scope could include project failure,unclear deliverables, confusion, increasedbudgets and expanding timeframes.Project aimA project aim should be aspirational,measureable and consistent with local andnational priorities and plans.A good aim statement should include: What we are trying to achieve For whom How much By when Compared to what And why?8/9We will achieve a 20% reduction inemergency admissions for heart failurepatients by March 2015This example does provide a clear anumerical target to aim for, but what is the20% measured against? Is it 20% reductionfrom the previous year? Is it realistic? Couldit be achieved?All practices need to use a care planningapproach for all patients with a longterm condition‘Need to’ is not an improvement aim. Is thisall practices across the country or allpractices in the consortia? Which careplanning approach should be used? Whenshould this be completed and what will itachieve?A good aim may look like this100% of patients on our list with aconfirmed diagnosis of COPD will have acomprehensive review and will have anindividualised care plan developed with thelead GP or practice nurse by March 2013.This will ensure that they are optimally caredfor and better able to manage theircondition, thereby reducing the frequencyand severity of exacerbations and the needfor possible future hospital admissions.Ensure your scope and aim is clear toeveryone involved. The language we use inthe NHS is sometimes ambiguous and canbe interpreted in different ways by differentpeople, for example ‘self management plan’- is this a piece of paper with genericinformation given to all symptomaticpatients or a personalised care plan for eachpatient? It is really important that you areclear in your aim and don’t leave anything tochance.Why should I get consensus aboutthe problem before starting theproject?There are numerous reasons why youshould discuss the problem andachieve a consensus before startingyour project. Different people willhave different ideas about theproblem, so it is important that youunderstand their perspective (as youmight learn something new) and forothers to understand your perspective.See the elephant analogy in Chapter 3.Very few people will understand thefull story as their perspective is basedon their own experiences. This processof gaining consensus, talking andlistening to the people involved in theprocess will assist with engagementand support for the project.
An adaptation of a Hindi proverbFive visually impaired people touch an elephant to learnwhat it is like. Each one feels a different part."Hey, the elephant is like a tree trunk," said thefirst man who touched the elephant’s leg."Oh, no! The elephant is like a snake" said thesecond man who felt the trunk."Oh, no! It is like a rope," said the third man whotouched the tail."It is like a brush" said the fourth man whorubbed the elephant ear.And the fifth man said "It’s soft and mushy "They began to argue about the elephant and they allinsisted they were right. They all were right in what theywere saying as they had all developed an understandingbased on their own experiences and perspective. However,they did not have an understanding of the whole elephant.Imagine the elephant to be a patient. Differentclinicians and health care staff see the patient indifferent ways, all of them correct, but by not seeingthe whole patient pathway, their understanding islimited. Make sure you understand the entireprocess/patient pathway before starting anyimprovement project.
FIRST STE PS T OWARD S Q UA LI TY IM P ROVE M E NT: A S I MP L E G UI D E T O I MP RO VI N G S E R VI C E SWhat makes successful projects?CHAPTER 3Managing a successful projectStarting out on any improvement project isan exciting time, and you are likely to be fullof enthusiasm and optimism. However,things don’t always go entirely to plan and itcan be hard to maintain impetus andprogress with enthusiasm alone.For a project to be successful, it is importantthat an adequate amount of time is spenton managing the project.Spending time getting the preparatory workright first time will be beneficial later in theproject. Preparatory work includes: Getting the right team (Chapter 5) Having a good relationship with yourexecutive sponsor (Chapter 5) Having a solid project plan (Chapter 3) Having a robust communication plan(Chapter 7) Understanding the current service(Chapter 2 and 8)10/11 Collecting baseline data and having adata collection plan (Chapter 10 and 11) Understanding your customerrequirements (Chapter 6).A project plan is fundamental to theestablishment of the project. It sets thecontract for improvement and establishesthe mandate, priorities and resourceavailability. In other words, it spells outclearly what, how and when is to be done,so that everyone is aware of theircommitments and how they will impact onthe project’s success. It can be tempting toignore this element as ‘bureaucratic’ or‘administrative’, but it is an essential tool forensuring there is clarity about the projectand that expectations are managed. Thisneed not be an onerous process, but theplan does need to clearly spell out the keyareas. Getting the right peopleinvolved from the start of theproject Having a clear aims statement Planning, monitoring and control Having a real understanding ofthe current issue or problem Measurable improvementswhich are achievements not justactivities Having clear links to local andnational objectives i.e. a clearreason to do it Involving patients and carers,(ideally) from the beginning Displaying effectivecommunication.The plan is developed in the preparationphase of the project and enables decisionsto be made with regard to modifying orcancelling the initiative in situations wherethe required support for the project eitherchanges or is lacking. The plan is usedthroughout the project for monitoringand control.
FIRST STE PS T OWARDS QU AL IT Y I MP RO VE ME N T: A S I MP L E G U I D E T O I MP RO VI N G S E R VI C E SWhy do projects fail? Project aims and objectives notclearly defined or articulated Little or no top level supportand leadership for the project Lack of effective engagementwith key players and patients Poorly planned projects Inadequately monitored,controlled and managed Failure to take account of localand national priorities Poor communication Failure to divide the project intosmall manageable tasks Unable to collect and analysedata.A project plan should specify: Aims and objectives Background to the project Scope of project Expected deliverables Timescale Analysis of risk Resources Budget Method/process Accountability Identification of the project sponsor Data and measures Dependencies (i.e. links between oneaction and another) How the work is going to be sustainedand spread to other areas.Project plans come in many different styles, buteach should set out all the actions that have tooccur to achieve the improvement, as well asclearly stating when these will happen andwho is responsible for doing them.Is my work a project?A project is a temporary piece of workwith a defined start and finish, and willnot continue indefinitely. Project workis also designed to deliver a definedoutcome or benefit from doing thework.Does someone need to projectmanage for a project to besuccessful?Yes, within the project team, someoneneeds to be responsible for the role.Without someone to undertake thisrole, it is unlikely that even the smallestproject team will deliver what it setsout to achieve within the agreedparameters.
Isn’t project management justunnecessary bureaucracy andadministration?Good project management is not justbureaucracy. It is about ensuring thereis consistent co-ordination, drive andevaluation of the project so that itremains focused and effective. Nothaving someone to manage theproject usually means that no onetakes overall responsibility for ensuringthat all the components are beingdelivered – and the project may thenfalter or fail.What is the role of a projectmanager?The role of a project manager is tohave oversight of the entire projectand take responsibility for controllingand monitoring each aspect, alongwith reporting the successes, learningand failures of the project. Not everyproject needs to a dedicated projectmanager, but every project requiressomeone to undertake the roles andresponsibilities of a project manager(see Chapter 5).12/13What is the difference between aresearch and improvement project?An improvement project is abouttesting ways to implement evidencebased care and find out the best wayfor a service to be organised anddelivered. It is about testing innovationor new ways of working and not abouttesting whether treatments orinterventions actually work.
FIRST STE PS T
Chapter 6 - Involving patients and carers in service redesign Chapter 7 - Communicating the right things to the right people Chapter 8 - Improvement tool: Process mapping Chapter 9 - Improvement tool: Plan, do, study, act cycles Chapter 10 - Measuring your efforts Chapter 11 - Improvement tool: Using statistical process control charts
bunchberry dr nhs wms amb . burgundy ln nhs wms twl . burkwood dr nhs wms amb . burning tree st chs wms twl . burnock dr chs wms mbe . burr ridge rd nhs nms twl . burrwood ave nhs nms ang . burrwood st nhs nms ang . burt dr chs cms lce
of NHS Direct, and led the team preparing New Labour's first White Paper, The New NHS: Modern, dependable, which laid the foundations and structure for the current NHS reform programme. He was a member of the top management board of the NHS for 12 years, between 1988 and 2000. His earlier career included 23 years in NHS management,
NHS Long Term Plan Implementation Framework I 3 Introduction to the NHS Long Term Plan Implementation Framework 1.1 The NHS Long Term Plan, published in January 2019, set out a 10-year practical programme of phased improvements to NHS services and outcomes, including a
allowances are known as NHS Bursaries’1 and apply to courses qualifying students for certain professions (see Professions with training funded by NHS Bursaries). Students wishing to undertake these courses apply for an NHS bursary instead of Student Finance. NHS Bursaries are award
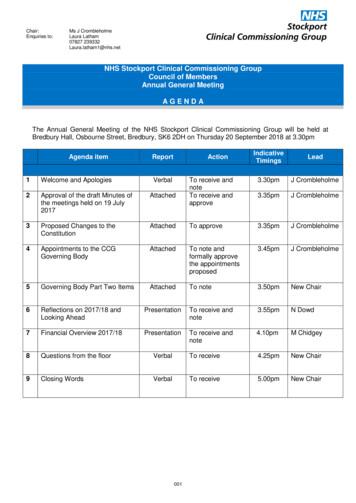
Dr Ranjit Gill . Chief Clinical Officer . NHS Stockport CCG . John Greenough . Lay Member . NHS Stockport CCG . Louise Hayes . Head of Communications and Engagement NHS Stockport CCG . Diane Jones . Director of Service Reform . NHS Stockport CCG . Dr Deborah Kendall .
Patient rights and NHS promises. 13. Part 4 - The things patients should do to help. 27. Part 5 - Rights and promises the NHS makes for NHS staff. 29. Part 6 - The things staff should do to help. 33. Part 7 - Telling the NHS
Currently working to align with work on RightCare'sFrailty Pathway and the Geriatric Medicine workstream of NHS Improvement's Getting It Right First Time (GIRFT) programme . NHS RightCare is a programme of NHS England Piers Glen NHS RightCare Delivery Partner 8 bpollington@nhs.net 07710 152763. Title: PowerPoint Presentation
It is now referenced in the Mandate to NHS England, the NHS Planning Guidance and the CCG Improvement and Assessment Framework. The RightCare programme includes the Commissioning for Value packs and tools, the NHS Atlas series and a number of casebooks. NHS England has committed significant funding to rolling out the RightCare