Fundamental Management: Revenue . - MA/RI Chapter Of
Fundamental Management:Revenue Cycle Management &Revenue CalculationsRosemary Sheehan,Vice President Revenue Cycle OperationsSeptember 2017AgendaPart I: Revenue Cycle Management–Need to get it right up front!–Future Payment Methodologies Physicians and hospitals will need to work togetherPart II: Net Revenue & Reserves– Difference Between Gross and Net– Setting Reserve Levels»Contractual Allowances»Denials»Charity Care»Bad Debt2
Revenue Cycle Processes3PHS Revenue Cycle OperationsFront End: Patient Access/Patient Service Center (PSC)Middle: Revenue Integrity (Charge Master, Error Resolution, Audit Functions) Hospital CodingBack End: Acute Hospital Central Billing Office Sub Acute Hospital Central Billing Office Professional Billing Office (Includes coding, charge entry, billing, collections andself-pay)Support Teams: Reimbursement and Revenue AnalysisRCO TrainingAnalysis and AdministrationPayer RelationsTotal Staff: 810 staff supporting theHospital Functions 370 staff supporting thePhysician Functions4
Revenue Cycle Operations (continued)Hospital Tools: Epic (MGH, BWH, NWH, FH and Home Health) 6 additional billing and accounts receivable systems Additional bolt on systems Huron Work listing – Insurance Follow up and Denial ManagementVRS – Remittance PostingXClaims – Claims Editing and TransportHyland Onbase – Document ImagingHarvest - Contract ManagementMedeAnalytics - Reporting & AR AnalysisPhysician Billing Office Tools: Epic Additional bolt on systems Ingenix Claims Manager – Claims Editing Hyland Onbase – Document ImagingFacts: PHS is in the process ofimplementing Epic’srevenue cycle andenterprise-wide clinicalapplications.FY16 Projected Payments 6BBad Debt (less Charity) 72MCharity Care 329MTotal Physicians/Providers billed through the MGPO: 32005Impact of Epic on the Revenue CycleEpic ImprovementsOne patient friendlystatement/customer service teamData integrity (enterprise patientdemographic updates)Exception based workflowsMore efficient and standard chargingpracticesTransparency of revenue cycle metricsFuture BenefitsImproved patient engagement(registration, self‐directed patientestimates, collections, results,communication, etc.)More effective capture of complexcharging, such as infusion (stillenhancing this workflow)Staff efficiencies and lower cost longtermStandard billing workflows; clearerhandoffs between teamsSmaller hospitals will benefit from allthe editing and work listingfunctionalityEase and flexibility meeting payerrules and eliminating manual workSimplicity of meeting futureregulatory and payer changes6
Revenue Cycle Operation (RCO) GoalsThere are three main goals in RCO. Everything we do is todrive improvement in these 3 goals.Optimize Collection of Cash ‐ Increasing Net Revenue7RCO GoalsThere are three main goals in RCO. Everything we do is todrive improvement in these 3 goals.Optimize Collection of Cash ‐ Increasing Net RevenueIncrease Efficiency ‐ Reduce Cost of Operations8
RCO GoalsThere are three main goals in RCO. Everything we do is todrive improvement in these 3 goals.Optimize Collection of Cash ‐ Increasing Net RevenueIncrease Efficiency ‐ Reduce Cost of OperationsProvide Highest Level of Service to our Patients ‐ Improve Engagement9The Revenue Cycle from 30,000 feet . . .PayerEnrollmentFix/ResubmitDeny BalanceSecondPayerBadDebtHSN(Free Care)10
Provider Enrollment1111Payer ranceCoding/ChargeCapturePre-BillingBillingDeny BalanceSecondPayerBadDebtHSN(Free Care)All providers must be enrolled (credentialed) with Third Party Payers in order forphysician services to be billed12
Payer Enrollment Providers must be enrolled with all payers before we can bill theirservices This function is currently decentralized and managed by eachhospital For some payers, the hospitals are delegated, which means that thepayer delegates the full enrollment responsibility to the Hospital.Once a provider is credentialed with the hospital, they becomeimmediately enrolled with the payer. A provider can be enrolledbut still be out of networkwith a specific employergroup or be considered ahigher tier or copayments13Patient Access1414
Pre‐Service Financial anceCoding/ChargeCaptureDeny e Care)Tools:Critical Functions: Electronic Eligibility Check Payer Web Sites Telephone Call Patient Estimator Registration/Insurance Verification/ FinancialCounseling Referrals/Clinical Authorizations/Pre-certifications Pre-Service Payments15Financial Clearance Most critical set of processes in therevenue cycle If financial clearance is not done well,there is no chance of getting paid Consists of registration, notification,referrals and prior authorization Payers continue to increase the intensityof the rulesRegistrationInsurance detailsReal timeeligibilityAdministrativeReferral –PrimarilyOutpatientServicesNotification toPayers forInpatientAdmissions SurgicalAdmissions –confirm level ofcareClinicalAuthorization forservices such asdrugs,proceduresConfirm benefits,in networkrelationshipMost insurance updates are done by the PatientService CenterAdmitting, ED and central registrars are also ableto do a full patient registrationThe practices should be verifying keydemographics at time of scheduling or at time ofcheck inInconsistencies should be directed to the PSC16
Real Time Eligibility We use NEHEN (New England Healthcare Exchange Network) for our dailyRTE transactions Partners Healthcare was a founding member of NEHEN in 1998 On a weekly basis, we conduct between 1.8 ‐ 2.1 million Real Time Eligibilitytransactions17Top Workqueue Edits Business Model Exception Based In our “Eligibility Needs Review” workqueues, we capture RTEstatuses that comeback in a “Needs Review” status We have our RTE set up to fire a “needs review” status whenany of these data elements do not match: Subscriber DOB Subscriber Name Subscriber ID/Member ID Plan Mismatch These Eligibility Needs Review WQs generate more than 15,000accounts a week We have more than 25 dedicated work queue users withincentral registration that work more than 9,500 accounts a week18
Top Workqueue Edits Our “No Coverage” WQs capture patients that do not haveany insurance coverage on their account The weekly volume of these WQs is over 10,000 We have 25 users that add coverage or mark the patients asself pay for over 6,000 of these accounts per week19Key Definitions in EpicCSN ‐ (contact serial number) ‐ aka visit # Represents an encounter with patient (admission, clinic visit, etc.)HAR ‐ (hospital account record) Account used to group all charges for billing purposes Associated to one or more patient visits A HAR is typically assigned to a visit during the scheduling/registrationprocess. The HAR Advisor is used to recommend when to create a newHAR or assign to an existing HAR. A visit can only be associated to a single HAR20
Charge Capture2121Charge Capture/CodingPayerEnrollmentFix/ResubmitDeny BalanceSecondPayerBadDebtHSN(Free Care)Charge Description Master (CDM): A price needs to be determined for each serviceCharge Capture: Charges come from primarily Epic clinical modules; outputs of clinicalactivityCoding: Coding is performed by certified coders for Inpatient Cases and procedures22
Revenue Integrity/Charging The goal is to ensure that all services that are performed arecaptured appropriately in Epic The revenue integrity team is responsible for all charging decisions,policies and the QA of the charging build in Epic Services can be billed: Hospital Global Hospital Split (health centers) PO/Hospital Split Revenue Capture:Most services are billed through selection of codes on a preference listOR services are charged using a combination of team size and timePharmacy is charged using a mark up of cost Room and Board is calculated based on the patients who are in beds atmidnight Many hospital procedures are generated once the tech completes theexam (cardiology procedures) 23Charge Codes The charge description master (CDM) houses all the charge codes forhospital services Charge codes are built in Epic and linked to cost centers Each charge code has a number of characteristics, such as revenuecode and CPT code A separate Masterfile in Epic details all cost centers (Cost CenterAssignment Table) The linkages of these two tables allows CPT codes to be used inspecific cost centers When we transitioned to Epic, we also moved to one charge master The charge router can manipulate charge and cpt codes: 5 cpt codes can be rolled up into one panel to meet specific payer rules If changes to codes need to be made, the teams reverse the wrong codeand add the new code24
Components of Revenue Integrity/Charging25Coding2626
CodingCoding for Inpatient Services All services are coded by a certified hospital coder They code using the DRG (Diagnosis Related Grouper) terminology; tocalculate DRG, they identify the: Admission diagnosisPrincipal diagnosisSecondary diagnosis(es)ComorbidityComplicationPrincipal procedureSecondary procedure(s)Coding for Outpatient Services Primarily exception based review of edits Generally medical necessity or diagnosis based editsRisk Coding Capture of chronic diagnosis codes27History of DRGsA Diagnosis‐Related Group (DRG) is a statistical system of classifying anyinpatient stay into groups for the purposes of payment. The DRG classificationsystem divides possible diagnoses into more than 20 major body systems andsubdivides them into almost 500 groups for the purpose of Medicarereimbursement.A DRG, or diagnostic related grouping, is how Medicare and some healthinsurance companies categorize hospitalization costs and determine how muchto pay for a patientʹs hospital stay. Rather than paying the hospital for what itspent caring for a hospitalized patient, Medicare pays the hospital a fixedamount based on the patient’s DRG or diagnosis.If the hospital treats the patient while spending less than the DRG payment, itmakes a profit.If the hospital spends more than the DRG payment treating the patient, it losesmoney.28
History of DRGsIn October 2007, Medicare Severity DRGs (MS‐DRGs) were implemented forMedicare inpatient discharges. CMS replaced 538 DRGs with 745 new DRGs.Every DRG was re‐categorized and had different meanings.MS‐DRGs moved from a two tier (CC/no CC) method of determining severity ofillness to a three tier method which expanded the ability to effectivelydemonstrate severity of illness. The three tier method of Major Complication orCo‐Morbid Condition (MCC), Complication or Co‐Morbid Condition (CC), or noMCC/CC, provided 3 levels of severity determination for reimbursement.With implementation of ICD‐10 in October 2015, CMS and 3M developed andtested new grouper versions for MS‐DRGs and APR‐DRGs for use with ICD‐10diagnosis and procedure codes.29Coding Clinical documentation is critical to coding processes If it is not documented, it did not happen Each hospital has a clinical documentation team (comprised of nurses)that work to ensure all Medicare cases are well documented tooptimize the DRG payment(s) and the quality metrics under valuebased incentive programs30
The Basics of the ICD‐10 Diagnosis CodesAn Example of Structural ChangeICD‐9XXXCategory.ICD‐10XXXXEtiology, anatomicsite, manifestationXCategory.An Example of One ICD‐9 codebeing Represented by MultipleICD‐10 Codes250.6Diabetes mellitus with neurologicalmanifestations type I not stated asuncontrolledX.XEtiology, anatomicsite, manifestationE10XExtension.4.40Type 1 diabetes mellitus with diabetic neuropathy,unspecifiedOne ICD‐9code isrepresentedby multipleICD‐10codes1XE101Type 1 diabetes mellitus with diabetic mononeuropathyE10.44Type 1 diabetes mellitus with diabetic amyotrophyE1049Type 1 diabetes mellitus with other diabeticneurological complication31The Basics of the ICD ICD‐10‐PCS (Procedure codes)The ICD‐10‐PCS is an American procedure coding system that represents a significant step towardbuilding a health information infrastructure that functions optimally in the electronic ageAn Example of Structural ChangeICD‐10‐PCSICD‐9XX.XXAn Example of One ICD-9 code beingRepresented by Multiple ICD-10 ApproachDeviceQualifier0SRB07Z Replacement of Left Hip Joint with Autologous Tissue Substitute, Open Approach0SRB0KZ Replacement of Left Hip Joint with Nonautologous Tissue Substitute, Open Approach0SRB0J7 Replacement of Left Hip Joint with Synthetic Substitute, Ceramic on Ceramic, Open Approach0SRB0J8 Replacement of Left Hip Joint with Synthetic Substitute, Ceramic on Polyethylene, Open Approach0SRB0J6 Replacement of Left Hip Joint with Synthetic Substitute, Metal on Metal, Open Approach81.0SRB0J5 Replacement of Left Hip Joint with Synthetic Substitute, Metal on Polyethylene, Open Approach51Total hip replacementOne ICD‐9code isrepresentedby multipleICD‐10 codes0SRB0JZ Replacement of Left Hip Joint with Synthetic Substitute, Open Approach0SR907Z Replacement of Right Hip Joint with Autologous Tissue Substitute, Open Approach0SR90KZ Replacement of Right Hip Joint with Nonautologous Tissue Substitute, Open Approach0SR90J7 Replacement of Right Hip Joint with Synthetic Substitute, Ceramic on Ceramic, Open Approach0SR90J8 Replacement of Right Hip Joint with Synthetic Substitute, Ceramic on Polyethylene, Open Approach0SR90J6 Replacement of Right Hip Joint with Synthetic Substitute, Metal on Metal, Open Approach0SR90J5 Replacement of Right Hip Joint with Synthetic Substitute, Metal on Polyethylene, Open Approach0SR90JZ Replacement of Right Hip Joint with Synthetic Substitute, Open Approach32
What is Risk Adjustment? Fundamentally, it is an actuarial tool used to calibrate the payments from CMS to MedicareAdvantage Plans based on the relative health of their at‐risk population The goal is to reflect the expected costs of providing care to their patients and to ensure thatappropriate compensation for the health status of the patients Risk adjustment focuses on a subset of ICD 10 codes which are bucketed into HCCs, orhierarchical condition categories (HCCs) There are currently 69,823 ICD‐10 codes that link to 87 HCCs. These HCCs are ranked frommost severe to least severe. The HCCs summarize the patient’s diagnostic profile. (There are 70HCCs of concern to PHS Primary Care.) CMSʹ model is accumulative, meaning that a patient can have more than one HCC categoryassigned to them and the are additive in that the risk weights of different HCCs are addedtogether to produce a risk score or RAF (Risk Adjustment Factor) The HCCs must be captured every calendar year for CMS to impact the risk adjustment andtherefore the Medicare Advantage payment This model or a similar model is used to risk adjust the Accountable Care Organization,Medicaid and Commercial Risk contractsThe ABCs of HCCs: Decoding CMSʹs Hierarchical Condition CategoriesBy Holly J. Cassano, CPCApril 14, 20113333The RAF Score The combination of HCC diagnosiscodes with demographic datacomprise the Risk Adjustment Factoror RAF Score, and this communicateshealth severityAge & Gender The RAF score acts as a multiplierwhen CMS calculates its payments Conditions must be documented andbilled at least once per calendar yearfor inclusion in the risk model Variations on the RAF Score are a keypart of how risk adjusted panels arecalculated by our commercial payersas wellTotal chronicconditions anddiseaseinteractions(HCCs)Medicaid ordisability statusRAFScore34
Pre‐Billing FunctionPayerEnrollmentFix/ResubmitDeny tPayerPre-BillingPay BadDebtPatientPostBilling WriteOffPostBalanceSecondPayerHSN(Free Care)Pre Claim Editing: PHS uses Ingenix for physician & XClaim for hospital servicesEdits look for: Missing data (diagnosis, doctor number, etc.) Correct coding (e.g., check for medical necessity)35 Other Payer specific billing requirementsPre Billing All hospital services run through a number of edits toensure that claims are clean before they are sent to thepayer Editing Tools: Epic edits Xclaim edits (Nthrive Product) The edits are disbursed to the teams most capable ofresolving the edits quickly Currently the clean claim rate is around 86%36
Billing Process ‐ The easy part!PayerEnrollmentFix/ResubmitDeny BillingBadDebtPatientPostHSN(Free Care)The goal is to send all claims electronically to all payers.However, often still send paper bills when: Medical Records are required Billing a Secondary Payer37Claims Processing Claims are sent electronically to the payers via a standard HIPAA transaction(837) For inpatient services, we capture all services and combine them onto oneclaim with to and from dates Any outpatient services performed within 72 hours of the inpatientadmissions are also combined on the inpatient claim Partners uses Nthrive’s Xclaim product as the claims clearing houseTotal Imports CountTotal Imports Dollars 174,187Total Imported Dirty CountTotal Imported Dirty Dollars% Imported Dirty (Count)% Imported Dirty (Volume)Annualized Claim CountAnnualized Claim Dollars1,280,3615,242,721,669 1,035,926,61514%20%5,121,444 20,970,886,67738
Why don’t the Payers just pay the claims?PayerEnrollmentFix/ResubmitDeny SecondPayerBillingBadDebtHSN(Free Care)Some Reasons Payers Deny Claims: Referral required but not obtainedPre-authorization missing or incorrectOther insurance involved (e.g., WC,MVA) Member no longer eligibleService not covered by the planService deemed not medically necessaryFiling limit exceeded39After an initial denial, can the claim be fixed?PayerEnrollmentFix/ResubmitDeny atientPaymentPayerRoot Cause teamswork on fixing theprocessto preventPostPayfuture denials.Pre-BillingClaimsthat cannot BadbePatientBalancefixed end up as Debt“Write‐Offs”SecondPayerBillingHSN(Free Care)Much effort in the backend is spent re-working initial “denials”: Contacting patients for better dataContacting doctors for referralsProviding PIP exhaust letters for Motor VehiclesProvide documentation for medical necessity40
Insurance Follow UpResponses from payers are posted to Epic through an electronic file, called an 835The file contains the following information: Payment Allowed amount Rejection code (if the claim doesn’t pay or partially pays) Patient LiabilityOnce the detail is posted to Epic, logic determines what the next actions are: Patient Liability bill patient Partial Pay (80%) Co‐insurance due bill secondary Claim Rejects file to a work queue for third party reviewer processingTop rejections: Auth/Referral Coordination of Benefits Patient not covered Not Medically Necessary Filing Limit41Patient Responsibility PayerEnrollmentFix/ResubmitDeny BalanceSecondPayerBadDebtHSN(Free Care)Two types of Patient Balances: “True” Self Pay (Uninsured) and Balances After Insurance Typically, patients get 4 statements / letters and phone calls for larger amounts. Currentlystratifying self pay follow-up by propensity to pay. Often, receiving a bill results in a call withupdated insurance information Unpaid balances generally are written off to bad debt.42
Self Pay ApproachCustomer Service PBS is handling 40,000 calls per month; call abandonment rate of 5‐6%Collections Self Pay balances flow into a series of follow up workqueues for action eitherthrough calls or targeted letters Accounts are prioritized for action using a Propensity to Pay/Expected Valueanalysis provided by our contracted vendor, ConnanceTrends in Benefit structures: High Deductible plans ( 2K‐ 5K) Co‐insurance plans (80%/20%) There is no approach to track patients with these types of plans There is no indicator in Epic to identify these plans, at this point43Self Pay Collections44
Self Pay ApproachEpic SBO Process Settings Guarantors are mailed one statement per month whenever there is a qualifyingbalance at the account (HAR) level in the patient ‘bucket’. SBO function is based on the creation of a Hospital Accounts receivable (HAR).This is done for both hospital (HB) and professional (PB) accounts. Each HAR canhave both insurance balances and patient balances pending. A HAR will only qualify for a statement when the entire balance is in the patientbucket. The account will not qualify for a statement is there are any balancespending in insurance within the HAR. Statements generate every 30 days and include all qualifying HAR’s. Accounts areincluded on the next available statement if there is a statement cycle running. Ifthere have been no recent statements then they start a new cycle and immediatelybill to the patient. The total guarantor balance must be greater than zero for any statement to beproduced including any deposits or pre‐visit payments. Accounts process through 4 dunning levels (4 statements). Accounts will notqualify for additional statements unless the statement cycle is manually reset. After 4 statements, accounts still unpaid will be sent to one of 2 collection vendors45Self Pay ApproachPatient Engagement Patients have two opportunities to review their accounts without engaging withCustomer Service by using our Pay‐by‐Phone IVR or through Partners PatientGateway (PPG) IVR – Patients can call Customer Service and choose an option off the phone menuto review or pay their account balance. The system will confirm their last statementbalance and current account balance. Patients can pay they balances by credit cardover the phone. System operates 24/7. Partners Patient Gateway – Patients can log into their Partners Patient Gatewayaccount for multiple actions: View a copy of their last statement. Paperless billing is possible using this feature View current account balances. The patient can see some details of their accounts that can’tbe printed on the statement Pay their account by credit card. They can either pay the entire balance or selectedaccounts Prepay copays for future visitsFuture PPG Enhancements are expected to include the ability for a patient to updatetheir insurance, demographics, set up a payment plan and request estimates.46
Major Patient Engagement InitiativesTechnology Expand texting and email use forappointment confirmations Expand functionality in thePatientGateway Online paymentsEstablish payment plansCheck in to appointmentsUpdate demographics/insurance Expand the use of Epic Welcome KiosksPatient Estimates Expand Epic functionality to BWH andFH Financial Counselor teams Currently live at MGH and NWH Expand to outpatient departments suchas Radiology Proactively push out estimates topatients for scheduled appointmentsPatient Statements Continue to improve the PatientStatement Convene annual patient focus groups tocapture feedback to ensure that ourstatements remain patient‐friendly47Typical Revenue Operations MetricsDays in AR: Measures how fast cash is being collected - PHS Goal 50 days for theAMCs, 36 days for the Community HospitalsAR Aging: Measures health of AR; the older the AR, the less likely it is that itwill be collected – PHS Goal AR older than 90 days should be 15%Cash Collection Rate: Goal should be to collect 100% of target (after deduction for budgeteduncollectible amounts of bad debt, denials, charity)Denial Percentage: Will depend on payer mix – PHS Goal 1% of Net RevenueBad Debt Percentage: Will depend on payer mix, charity care policy & demographics – PHSGoal 1-2% of Net Revenue48
AgendaPart I: Revenue Cycle Management–Need to get it right up front!–Future Payment Methodologies Physicians and hospitals will need to work togetherPart II: Net Revenue & Reserves– Difference Between Gross and Net– Setting Reserve Levels»Contractual Allowances»Denials»Charity Care»Bad Debt49Financial ReportingGross vs. Net Key question: How much of our Gross Revenue do wereally expect to collect? Start with Gross Revenue; but then need n for Contractual AllowancesProvision for DenialsProvision for Charity CareProvision for Bad Debt50
Income Statement vs. Balance Sheet ModelTwo options: Income Statement approach looks at new revenue eachmonth and provides a reserve for expected non-collectables Balance Sheet approach looks at the AR by Payer and agingbucket each month and estimates how much reserve isrequired for each “bucket”. Each month, an entry is made totrue up the provision to the most current estimated need Some entities use both– Use Income Statement method each month– Then validate with the Balance sheet method on quarterlybasis51Two versions of the Income Statement Approach Contractual provisions often determined from:– Contract Management System» Each Payer contract modeled and loaded– Note need to update the model for contract changes, price increases,etc.» System reviews each claim & models contractual allowance needand “expected net revenue”– Historical payment history» Does not model expected payment claims by claim» Uses history of cash collection to estimate future collections» Updated periodically to “true up” estimates to actual cashcollections52
Example of Contractuals via Cash StudiesContractual Provision via historical cash studies(Column 1 times Column 3 Column 5)GrossRevenue1C/ANet Cash(from ed 3Quick Balance Sheet Example – One Payer1. Start with AR Balance for Payer by aging bucket . . .PayerManagedCare ARDenialNeed %Need0-6060-120120-180180-365 00200,0001,700,0002. Apply estimates of reserve need calculated from historical run outsNote that the assumed need percentage increases with the age of thereceivable. This exercise would be completed for every Payer to determinethe total need.54
How Do You Estimate the “Denial Need”?How to Conduct a “Run Out Analysis”1.Identify all AR accounts as of a point in time»2.3.Say, 2 years ago. . .Watch what happens to the AR over time»What transactions hit these accounts?»See how much from each Payer / aging bucket ended up as contractual, bad debt, denial,charityTranslate into percentages to use in balance sheet model55Run Out Example by Aging . . .Summary Run‐Out by Aging (amount)56
Quick Note on Third Party Liabilities Other adjustments to net revenue may berequired due to things like:– Risk contracts, e.g., pay for performance– Price protected PAF’s57Pulling it Together: A Simple ExampleGross Revenue: 50 million Set aside 40% for Contractual Allowance 20 million 30 millionLess Other Billing Reserves: Set aside 10% Charity Care 5 million Set aside 2% Denials 1 million Set aside 2% Bad Debt 1 million 7 millionSubtotal (NPSR) 23 millionrd 3 Party: Add P4P 1 million 1 millionNet Revenue 24 million58
Questions?Thank you for your time!5959
Sep 22, 2017 · Fundamental Management: Revenue Cycle Management & Revenue Calculations Rosemary Sheehan, Vice President Revenue Cycle Operations September 2017 2 Agenda Part II: Net Revenue & Reserves – Difference Between Gross and Net – Setting Reserve Levels »Contractual Allowances
Strategies to Optimize Your Pharmacy Revenue Cycle 9/2/2020 5 Presentation Outline 1. Optimal Revenue Cycle Management Program 1. Creating a case for a revenue cycle program 2. Revenue cycle program structure 3. Involving pharmacist leadership 4. Put a revenue cycle program to practice 2. Revenue Improvement and Preservation Strategies 1.
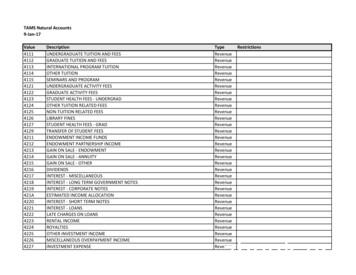
Jan 17, 2009 · 446F VECTOR-BORNE DISEASES. Revenue 446G. REVENUE - REAL TIME Revenue. 446H AEROBIOLOGY. Revenue 446I. . USHC PHARMACY CREDIT CARD SALES Revenue. Student Hlth Svc Use Only 4531. ASSESSED STUDENT FEES Revenue. 4532 VOLUNTARY STUDENT FEES. Revenue . GIFT SHOP INCOM
CHAPTER TWO Revenue Accounting and Reporting Procedures 9 2.1 Revenue Chart of Accounts 9 2.2 Taxes 11 2.3 Other Revenue 11 . 4.10.1 Auditing the revenue money receipts, the auditor shall verify 31 4.11 References for Revenue Auditing 32 ANNEXURES 35. REVENUE MANUAL 2019 1 INTRODUCTION
revenue recognition model to the new revenue standard's control-based model is a fundamental change in how entities are required to think about revenue recognition. The new revenue standard eliminates many of the revenue recognition rules prescribed under legacy US GAAP and replaces them with a principles-based framework
Revenue Cycle team Revenue Cycle Management Presented by: Kimberly Moore Director, Health Care Revenue Cycle Consulting 701.239.8673 . Cash Collection as a % of Adjusted net Patient Service Revenue: Indicator to accurately report effectiveness for converting Patient Service Revenue into
S.1 Revenue Requirements Table S1 shows the 2015 and 2016 Revenue Requirements and the respective annual changes. The revenue requirement shown here differs from the revenue requirement found in the COSACAR, which treats rate discounts as a cost for the purposes of cost allocation. Table S1 Revenue Requirements Millions 2014 Plan 2015 2016
estimated appro- approp unemployment reserve for reserve for reserve for capital repair nonspendable assigned aprop unassigned boe entry revenue revenue revenue priations fund balance reserve retrmnt cont tax certiorari emp benefits reserve - 07 reserve prepaid exp fund bal fund bal budget date item # code received #510 budget code #
enFakultätaufAntragvon Prof. Dr. ChristophBruder Prof. Dr. DieterJaksch Basel,den16. Oktober2012, Prof. Dr .