NYSDFS: New York Consumer Guide To Health Insurance Companies
New York Consumer Guide toHealth Insurance Companies2017New York StateAndrew M. Cuomo, Governor
Table of ContentsABOUT THIS GUIDE . 2COMPLAINTS . 4PROMPT PAY COMPLAINTS . 9INTERNAL APPEALS . 14EXTERNAL APPEALS. 19GRIEVANCES . 24ACCESS AND SERVICE . 29CHILD AND ADOLESCENT HEALTH . 32ADULT HEALTH . 35WOMEN’S HEALTH . 38BEHAVIORAL HEALTH . 41QUALITY OF PROVIDERS . 44MANAGING MEDICATIONS. 47DIABETES CARE . 50HEALTH INSURANCE COMPANY ACCREDITATION . 53OVERALL COMPLAINT RANKING . 56INDEPENDENT DISPUTE RESOLUTION . 60HOW HEALTH INSURANCE COMPANIES PAY HEALTH CARE PROVIDER . 63TELEPHONE NUMBERS FOR HEALTH INSURANCE COMPANIES . 64CONTACTS AND RESOURCES . 66
2New York Consumer Guide toHealth Insurance Companies DOH collects data through the New York State Department ofHealth’s Quality Assurance Reporting Requirements (QARR) andthe Consumer Assessment of Healthcare Providers and Systems(CAHPS 2).ABOUT THIS GUIDEThe purpose of this Guide1 is to: Inform you of the health insurance products offered in New YorkState and how they work. Help you choose a health insurance company based on quality ofcare and service.DATA SOURCESThe information in this Guide is provided by two New York agencies.1. New York State Department of Financial Services (DFS) isresponsible for protecting the public interest by supervising andregulating financial products and services, including those subject tothe provisions of the Insurance Law and the Banking Law in NewYork State. DFS compiles the complaint and appeal information that appearson pages 4–23, the grievance information that appears onpages 24–28 and the independent dispute resolution informationthat appears on pages 60–62. DFS data are from calendar year 2016.2. New York State Department of Health (DOH) works to protect andpromote the health of New Yorkers through prevention, researchand by ensuring delivery of quality health care. DOH compiles itsportion of the complaint data on page 5 and the information onhealth insurance company performance that appears on pages29–52. DOH data on quality of care and service for health insurancecompanies are from calendar year 2015.DETAILS ABOUT THE DATA The Guide does not include:– HMOs with less than 25 million in premiums or fewer than 5,000members.– Commercial and EPO/PPO plans with less than 50 million inpremiums.– Data for Medicare, Medicaid or self-insured plans.3 Health insurance companies that were in operation during the entire2015 calendar year were required to report DOH data. Health insurance companies are listed alphabetically in the datatables, except for the Overall Complaint Ranking table on pages56–59. Some health insurance companies are listed using different names,depending on whether the data are reported by DFS or by DOH.1This Guide is published pursuant to §210 of the New York Insurance Law.2 CAHPS is a registered trademark of the Agency for Healthcare Research and Quality(AHRQ).3 Forinformation about Medicare coverage, call the Centers for Medicare & Medicaid Services(CMS), the federal agency that oversees this program, at 800-MEDICARE (800-633-4227), orvisit the website at www.medicare.gov. You can also contact the New York State Office forthe Aging Health Insurance Information Counseling & Assistance Program (HIICAP) by calling800-701-0501, or by visiting the website at www.aging.ny.gov/healthbenefits/. Forinformation on New York’s Medicaid program, contact your local county Department of SocialServices.
3New York Consumer Guide toHealth Insurance Companies1HEALTH INSURANCE COMPANY AND PLAN DEFINITIONSHealth Maintenance Organization (HMO) Plan: A type of coveragethat provides comprehensive health services to members in return for amonthly premium and copayment. In an HMO plan, members choose anin-network primary care physician (PCP) who coordinates eachassigned member’s care. Members need a referral from their PCP toobtain services from in-network specialists and additional providerservices. Although many HMOs require their members to go to doctorsand other providers in the HMO provider network, some HMO plansoffer the option to go out-of-network (for example in an HMO Point ofService [POS] plan). Unless a member has an HMO plan that offers anout-of-network option, out-of-network services are usually not covered.Exclusive Provider Organization (EPO) Plan: A type of coverage inwhich the insurer contracts with doctors, hospitals and other types ofproviders to form a network of providers. Certain services may requirepre-authorization. In an EPO, members must use the providers whobelong to the EPO network or their expenses will not be covered.1 Referencesto the terms “companies” and “plans” are used interchangeably and includeHMOs, EPO/PPOs and commercial health insurance companies, unless it is clear from thecontext, such as in the various charts, that only the term specifically mentioned is beingdiscussed.Preferred Provider Organization (PPO) Plan: A type of managedcare coverage based on a network of doctors and hospitals thatprovide care to an enrolled population at a prearranged discountedrate. PPO members do not usually need a referral to see a specialist,but certain services may require pre-authorization from the healthinsurance company. PPO members may use out-of-network providers;however, members usually pay more when they receive care outsidethe PPO network.Commercial Insurers: Health insurance can also be written by lifeinsurers, property/casualty insurers and other types of insurers.Commercial insurers employ managed care strategies but offer a moretraditional approach to coverage than HMOs. Policyholders are subjectto deductibles and significant out-of-pocket costs unless they use apreferred provider network.
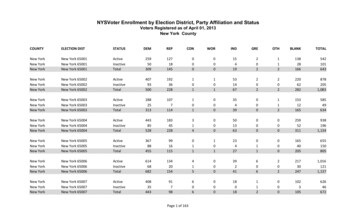
4ComplaintsEach year, the New York State DFS and DOH receive complaints from consumers and health care providers about health insurance companies.Complaints handled by DFS typically involve issues related to prompt payment, reimbursement, coverage, benefits, rates and premiums. Complaintshandled by DOH involve concerns about the quality of care received by Managed Care HMO members. After reviewing each complaint, the Statedetermines whether the health insurance company acted appropriately. If the State determines that the health insurance company did not act inaccordance with its statutory and contractual obligations, the company must resolve the problem to come into compliance.For issues concerning payment, reimbursement, coverage, benefits, rates and premiums, contact DFS at: www.dfs.ny.gov/consumer/fileacomplaint.htmor call 800-342-3736.UNDERSTANDING THE CHARTS Rank: Each health insurance company’s rank is based on howmany complaints were resolved by DFS in favor of the memberor provider, relative to the company’s premiums. A lower numberresults in a higher ranking. A higher ranking means that the healthinsurance company had fewer complaints relative to its size. Premiums: Dollar amount generated by a health insurancecompany in New York State during 2016. Premiums are used tocalculate the complaint ratio so that health insurance companies ofdifferent sizes can be compared fairly. Premium data excludeMedicare and Medicaid. Total Complaints to DFS: Total number of complaints closed byDFS in 2016. Large health insurance companies may receivemore complaints because they have more members than smallerhealth insurance companies. Complaint Ratio: Number of complaints upheld (complaintsresolved in favor of the member or provider) by DFS, divided bythe health insurance company’s premiums. Upheld Complaints by DFS: Number of closed complaintsresolved in favor of the member or provider because DFSdetermined that the health insurance company did not complywith statutory or contractual obligations. Complaints upheld byDFS are used to calculate the complaint ratio and ranking. Total Complaints to DOH: Total number of complaints closed byDOH. Complaints to DOH involve concerns about the quality ofcare received by members with Managed Care HMO plans. Upheld Complaints by DOH: Number of complaints closed byDOH that were decided in favor of the member or provider.
5Complaints—HMOs 2016Data Source: DFS and DOHData Compiled by theNew York State DOHData Compiled by the New York State DFSHMOCapital District Physicians Health PlanCommunity Blue (HealthNow)Empire HealthChoice HMO, Inc.Excellus Health PlanHIP Health Maintenance OrganizationIndependent Health Association, Inc.MVP Health Plan, Inc.Oxford Health Plans (NY), Inc.UnitedHealthcare of New York, Inc.1IfRank1,2Total1 BestComplaints9 Worstto omplaintsby DFS00208398335440409the ratios are the same among HMOs, the HMO with the higher annual premium amount receives a higher ranking.with a lower complaint ratio receive a higher ranking.2HMOsPremiums(Millions ints toDOH01711114218UpheldComplaintsby DOH0000000101
6Complaints—EPO/PPO Health Plans 2016Data Source: DFSEPO/PPO Health PlanAetna Life Insurance Company2CDPHP Universal Benefits, Inc.2CIGNA Health and Life Insurance Company2Empire HealthChoice Assurance, Inc.2Excellus Health Plan, Inc.2Group Health Incorporated2Health Insurance Plan of Greater New York2HealthNow New York Inc.2Independent Health Benefits CorporationNippon Life Insurance Company of AmericaNorth Shore-LIJ Care Connect Insurance Company, Inc.Oscar Insurance CorporationOxford Health Insurance, Inc.UnitedHealthcare Insurance Company of New York2Rank1TotalUpheld1 Best Complaints Complaints14 Worstto DFSby 1866health plans with a lower complaint ratio receive a higher ranking.complaint ratios and premiums include data from the health insurance company’s EPO, PPO and commercial business.2Complaints,Premiums(Millions .01760.0373
7Complaints—Commercial Health Insurance Companies 2016Data Source: DFSCommercial Health Insurance CompanyAmerican Family Life Assurance Company of New YorkBerkshire Life Insurance Company of AmericaCIGNA Life Insurance Company of New YorkCombined Life Insurance Company of New YorkDelta Dental of New York, Inc.3Dentcare Delivery Systems, Inc.3Eastern Vision Service Plan, Inc.4First Reliance Standard Life Insurance CompanyFirst Unum Life Insurance CompanyGenworth Life Insurance Company of New YorkGuardian Life Insurance Company of AmericaHartford Life and Accident Insurance CompanyHM Life Insurance Company of New YorkHumana Insurance Company of New YorkJohn Hancock Life & Health Insurance CompanyLiberty Life Assurance Company of Boston1IfRank1,21 Best32 aints Complaintsto DFSby ums(Millions the ratios are the same among commercial health insurance companies, the commercial health insurance company with the higher annual premium amount receives a higher ranking.health insurance companies with a lower complaint ratio receive a higher ranking.3Plan issues dental coverage only.4Plan issues vision coverage only.2Commercial
8Complaints—Commercial Health Insurance Companies 2016, cont’d.Data Source: DFSCommercial Health Insurance CompanyMassachusetts Mutual Life Insurance CompanyMetropolitan Life Insurance CompanyMutual of Omaha Insurance CompanyMVP Health Services Corporation3National Union Fire Insurance Company of Pittsburgh, PANew York Life Insurance CompanyNorthwestern Mutual Life Insurance CompanyPaul Revere Life Insurance CompanyPrincipal Life Insurance CompanyProvident Life and Casualty Insurance CompanyPrudential Insurance Company of AmericaShelterPoint Life Insurance CompanyStandard Life Insurance Company of New YorkStandard Security Life Insurance Company of New YorkSun Life and Health Insurance CompanyTransamerica Financial Life Insurance CompanyRank1,21 Best32 Complaints Complaintsto DFSby ms(Millions .05220.0165ratios are the same among commercial health insurance companies, the commercial health insurance company with the higher annual premium amount receives a higher ranking.health insurance companies with a lower complaint ratio receive a higher ranking.3Plan issues dental coverage only.2Commercial
9Prompt Pay ComplaintsNew York State requires all health insurance companies to: Pay undisputed electronic claims within 30 days and pay undisputed paper claims within 45 days of receipt, or Request all additional information from the member or the provider, if necessary, within 30 days of receipt of the claim, or Deny the claim within 30 days of receipt.For issues concerning payment, reimbursement, coverage, benefits, rates and premiums, contact DFS at: www.dfs.ny.gov/consumer/fileacomplaint.htmor call 800-342-3736.UNDERSTANDING THE CHARTS Rank: Each health insurance company’s rank is based on thenumber of prompt pay complaints upheld, relative to thecompany’s premiums. A lower number results in a higher ranking.A higher ranking means that the health insurance company hadfewer complaints relative to its size. Upheld Prompt Pay Complaints: Number of closed prompt paycomplaints where DFS determined that the health insurance companywas not processing claims in a timely manner. Prompt pay complaintsupheld by DFS are used to calculate the prompt pay complaint ratioand ranking. Total Complaints: Total number of complaints closed by DFS in2016. Complaints typically involve issues about prompt payment,reimbursement, coverage, benefits, rates and premiums. Premiums: Dollar amount generated by a health insurance companyin New York State during 2016. Premiums are used to calculate theprompt pay complaint ratio so that health insurance companies ofdifferent sizes can be compared fairly. Premium data excludeMedicare and Medicaid. Total Prompt Pay Complaints: Total number of prompt paycomplaints closed by DFS in 2016. Large health insurancecompanies may receive more complaints because they have moremembers and pay more claims than smaller health insurancecompanies. Prompt Pay Complaint Ratio: Number of prompt pay complaintsupheld divided by the health insurance company’s premiums.
10Prompt Pay Complaints—HMOs 2016Data Source: DFSHMOCapital District Physicians Health PlanCommunity Blue (HealthNow)Empire HealthChoice HMO, Inc.Excellus Health PlanHIP Health Maintenance OrganizationIndependent Health Association, Inc.MVP Health Plan, Inc.Oxford Health Plans (NY), Inc.UnitedHealthcare of New York, Inc.Rank1,21 Best9 Worst139285467Total1IfTotalComplaintsTotalPrompt PayComplaintsUpheldPrompt PayComplaintsPremiums(Millions )Prompt he ratios are the same among HMOs, the HMO with the higher annual premium amount receives a higher ranking.with a lower complaint ratio receive a higher ranking.2HMOs
11Prompt Pay Complaints—EPO/PPO Health Plans 2016Data Source: DFSEPO/PPO Health PlanAetna Life Insurance Company3CDPHP Universal Benefits, Inc.3CIGNA Health and Life Insurance Company3Empire HealthChoice Assurance, Inc.3Excellus Health Plan, Inc.3Group Health Incorporated3Health Insurance Plan of Greater New York3HealthNow New York Inc.3Independent Health Benefits CorporationNippon Life Insurance Company of AmericaNorth Shore-LIJ Care Connect Insurance Company, Inc.Oscar Insurance CorporationOxford Health Insurance, Inc.UnitedHealthcare Insurance Company of New York3Rank1,2TotalUpheld1 BestTotalPrompt Pay Prompt Pay14 Worst Complaints Complaints 8381,40044021541512611028243718351the ratios are the same among EPO/PPO health plans, the EPO/PPO health plan with the higher annual premium amount receives a higher ranking.health plans with a lower complaint ratio receive a higher ranking.3Complaints, complaint ratios and premiums include data from the health insurance company’s EPO, PPO and commercial business.2EPO/PPOPremiums(Millions )Prompt 20.00770.0151
12Prompt Pay Complaints—Commercial Health Insurance Companies 2016Data Source: DFSCommercial Health Insurance CompanyAmerican Family Life Assurance Company of New YorkBerkshire Life Insurance Company of AmericaCIGNA Life Insurance Company of New YorkCombined Life Insurance Company of New YorkDelta Dental of New York, Inc.3Dentcare Delivery Systems, Inc.3Eastern Vision Service Plan, Inc.4First Reliance Standard Life Insurance CompanyFirst Unum Life Insurance CompanyGenworth Life Insurance Company of New YorkGuardian Life Insurance Company of AmericaHartford Life and Accident Insurance CompanyHM Life Insurance Company of New YorkHumana Insurance Company of New YorkJohn Hancock Life & Health Insurance CompanyLiberty Life Assurance Company of Boston1IfRank1,21 Best32 21114151100111924104221Total PromptUpheldPayPrompt PayComplaints (Millions 8221.79398.8095.2070.70168.37109.8765.77the ratios are the same among commercial health insurance companies, the commercial health insurance company with the higher annual premium amount receives a higher ranking.health insurance companies with a lower complaint ratio receive a higher ranking.3Plan issues dental coverage only.4Plan issues vision coverage only.2CommericialPrompt 90.00000.0000
13Prompt Pay Complaints—Commercial Health Insurance Companies 2016, cont’d.Data Source: DFSCommercial Health Insurance CompanyMassachusetts Mutual Life Insurance CompanyMetropolitan Life Insurance CompanyMutual of Omaha Insurance CompanyMVP Health Services Corporation3National Union Fire Insurance Company of Pittsburgh, PANew York Life Insurance CompanyNorthwestern Mutual Life Insurance CompanyPaul Revere Life Insurance CompanyPrincipal Life Insurance CompanyProvident Life and Casualty Insurance CompanyPrudential Insurance Company of AmericaShelterPoint Life Insurance CompanyStandard Life Insurance Company of New YorkStandard Security Life Insurance Company of New YorkSun Life and Health Insurance CompanyTransamerica Financial Life Insurance Company1IfRank1,2Total PromptUpheldTotal1 BestPayPrompt Pay32 Worst Complaints Complaints Premiums(Millions )Prompt 00.00000.0042the ratios are the same among commercial health insurance companies, the commercial health insurance company with the higher annual premium amount receives a higher ranking.health insurance companies with a lower complaint ratio receive a higher ranking.3Plan issues dental coverage only.2Commericial
14Internal AppealsAn internal appeal or utilization review (UR) occurs when a member or provider asks a health insurance company to reconsider its refusal to pay for amedical service that the health insurance company considers experimental, investigational, not medically necessary, a clinical trial or a treatment for arare disease. A member may also appeal when the health plan denies a request to pay for an out-of-network service1 if the health plan offers analternate service in-network or if the health plan denies an out-of-network referral.2Health insurance companies are required to have appeals reviewed by medical professionals. Common internal appeals involve the medical necessityof hospital admissions, length of hospital stays and use of certain medical procedures.UNDERSTANDING THE CHARTS Filed Appeals: Number of internal appeals submitted to thehealth insurance company by members or providers in 2016. Closed Appeals: Number of internal appeals that the healthinsurance company decided by the end of 2016. Reversals on Appeals: Number of closed internal appealswhere the health insurance company decided in favor ofmembers or providers. If a health insurance company’s decision todeny payment or coverage is reversed on an internal appeal,the health insurance company agrees to pay for the service orprocedure. Reversal Rate: Percentage of reversals on appeals divided byclosed appeals.1 Anout-of-network service denial is a pre-authorization request that is denied because theservice is not available in-network and the health plan recommends an alternate in-networkservice that it believes is not materially different from the requested out-of-network service.2 Anout-of-network referral denial occurs when the member’s out-of-network referral request isdenied because the health plan has an in-network provider with appropriate training andexperience to meet the particular needs of the member.KEEP IN MINDA health insurance consumer should pay specific attention to a healthinsurance company that has a very high or very low reversal rate.Please note: There is no “ideal” reversal rate. A low reversal rate may indicate that the health insurancecompany’s initial decisions are correct, so fewer decisions requirereversal, but an unusually low reversal rate may indicate that thehealth insurance company does not give appropriatereconsideration to initial decisions. A high reversal rate may indicate that a health insurancecompany’s internal appeal process is responsive to members andproviders, but an unusually high reversal rate may indicate thatthe health insurance company’s process for making initialdecisions is flawed. The number of internal appeals filed may be higher for healthinsurance companies that actively promote the appeal processand encourage members and providers to appeal deniedservices.
15Internal Appeals—HMOs 2016Data Source: DFSHMOCapital District Physicians Health PlanCommunity Blue (HealthNow)Empire HealthChoice HMO, Inc.Excellus Health PlanHIP Health Maintenance OrganizationIndependent Health Association, Inc.MVP Health Plan, Inc.Oxford Health Plans (NY), Inc.UnitedHealthcare of New York, ,1402734,477ReversalReversals 53.48%45.57%internal appeals can exceed filed internal appeals in 2016 because closed internal appeals also include internal appeals filed prior to 2016.
16Internal Appeals—EPO/PPO Health Plans 2016Data Source: DFSEPO/PPO Health PlanFiledAppealsClosedAppeals1Aetna Life Insurance Company2CDPHP Universal Benefits, Inc.2CIGNA Health and Life Insurance Company2Empire HealthChoice Assurance, Inc.2Excellus Health Plan, Inc.2Group Health Incorporated2Health Insurance Plan of Greater New York2HealthNow New York Inc.2Independent Health Benefits CorporationNippon Life Insurance Company of AmericaNorth Shore-LIJ Care Connect Insurance Company, Inc.Oscar Insurance CorporationOxford Health Insurance, Inc.UnitedHealthcare Insurance Company of New rsalReversals 5.37%37.43%39.14%internal appeals can exceed filed internal appeals in 2016 because closed internal appeals also include internal appeals filed prior to 2016.appeals and reversal rates include data from the health insurance company’s EPO, PPO and commercial business.
17Internal Appeals—Commercial Health Insurance Companies 2016Data Source: DFSCommercial Health InsuranceCompany1American Family Life Assurance Company of New YorkBerkshire Life Insurance Company of AmericaCIGNA Life Insurance Company of New YorkCombined Life Insurance Company of New YorkDelta Dental of New York, Inc.3Dentcare Delivery Systems, Inc.3Eastern Vision Service Plan, Inc.4First Reliance Standard Life Insurance CompanyFirst Unum Life Insurance CompanyGenworth Life Insurance Company of New YorkGuardian Life Insurance Company of AmericaHartford Life and Accident Insurance CompanyHM Life Insurance Company of New YorkHumana Insurance Company of New YorkJohn Hancock Life & Health Insurance CompanyLiberty Life Assurance Company of Boston1ManyFiled AppealsClosedAppeals2Reversals onAppealsReversal 00%0.00%of the commercial companies do not write traditional comprehensive health insurance products, and therefore have no internal appeals.internal appeals can exceed filed internal appeals in 2016 because closed internal appeals also include internal appeals filed prior to 2016.3Plan issues dental coverage only.4Plan issues vision coverage only.2Closed
18Internal Appeals—Commercial Health Insurance Companies 2016, cont’d.Data Source: DFSCommercial Health Insurance Company1Filed AppealsClosedAppeals2Massachusetts Mutual Life Insurance CompanyMetropolitan Life Insurance CompanyMutual of Omaha Insurance CompanyMVP Health Services Corporation3National Union Fire Insurance Company of Pittsburgh, PANew York Life Insurance CompanyNorthwestern Mutual Life Insurance CompanyPaul Revere Life Insurance CompanyPrincipal Life Insurance CompanyProvident Life and Casualty Insurance CompanyPrudential Insurance Company of AmericaShelterPoint Life Insurance CompanyStandard Life Insurance Company of New YorkStandard Security Life Insurance Company of New YorkSun Life and Health Insurance CompanyTransamerica Financial Life Insurance 01040000400011039014,3381ManyReversals onAppeals08,532042000020003017011,439of the commercial health insurance companies do not write traditional comprehensive health insurance products, and therefore have no internal appeals.internal appeals can exceed filed internal appeals in 2016 because closed internal appeals also include internal appeals filed prior to 2016.3Plan issues dental coverage only.2ClosedReversal %79.78%
19External AppealsAfter an unsuccessful internal appeal, members and providers may request an external appeal when a health insurance company continues to refuse topay for/ provide reimbursement for health care services on the basis that services are experimental, investigational, not medically necessary, a clinicaltrial or a treatment for a rare disease. A member may also appeal when the health plan denies a request to pay for an out-of-network service1 if thehealth plan offers an alternate service in-network or if the health plan denies an out-of-network referral.2 If the health plan denies coverage of a nonformulary drug, the member or provider may be eligible to request a formulary exception for that drug through the external appeal process,depending on the type of policy3. A formulary is a list of prescription drugs that are covered by a member’s health plan.Before requesting an external appeal, you usually must complete the
Health insurance companies that were in operation during the entire 2015 calendar year were required to report DOH data. Health insurance companies are listed alphabetically in the data tables, except for the Overall Complaint Ranking table on pages 56-59. Some health insurance companies are listed using different names,
New York Buffalo 14210 New York Buffalo 14211 New York Buffalo 14212 New York Buffalo 14215 New York Buffalo 14217 New York Buffalo 14218 New York Buffalo 14222 New York Buffalo 14227 New York Burlington Flats 13315 New York Calcium 13616 New York Canajoharie 13317 New York Canaseraga 14822 New York Candor 13743 New York Cape Vincent 13618 New York Carthage 13619 New York Castleton 12033 New .
N Earth Science Reference Tables — 2001 Edition 3 Generalized Bedrock Geology of New York State modified from GEOLOGICAL SURVEY NEW YORK STATE MUSEUM 1989 N i a g a r R i v e r GEOLOGICAL PERIODS AND ERAS IN NEW YORK CRETACEOUS, TERTIARY, PLEISTOCENE (Epoch) weakly consolidated to unconsolidated gravels, sands, and clays File Size: 960KBPage Count: 15Explore furtherEarth Science Reference Tables (ESRT) New York State .www.nysmigrant.orgNew York State Science Reference Tables (Refrence Tables)newyorkscienceteacher.comEarth Science - New York Regents January 2006 Exam .www.syvum.comEarth Science - New York Regents January 2006 Exam .www.syvum.comEarth Science Textbook Chapter PDFs - Boiling Springs High .smsdhs.ss13.sharpschool.comRecommended to you b
CITY OF NEW YORK, BRONX, KINGS, NEW YORK, QUEENS, AND RICHMOND COUNTIES, NEW YORK 1.0 INTRODUCTION 1.1 Purpose of Study This Flood Insurance Study (FIS) revises and updates a previous FIS/Flood Insurance Rate Map (FIRM) for the City of New York, which incorporates all of Bronx, Kings, New York, Queens, and Richmond counties, New York, this alsoFile Size: 1MB
Garden Lofts Hoboken,New York Soho Mews 311 West Broadway, New York 8 Union Square South, New York 129 Lafayette St., New York The Orion Building 350 West 42nd St., New York Altair 20 15 West 20th St., New York Altair 18 32 West 18th St., New York The Barbizon 63rd St. & Lexington Ave., New York T
New York 65024 : Active . 648 : 108 . 0 : 4 . 19 : 1 . 0 : 324 . 1,104 New York New York 65024 Inactive 27 8 0 0 0 0 0 12 47 New York New York 65024 Total 675 116 0 4 19 1 0 336 1,151 New York : New York 65025 . Active
relation to persons joining the New York state and local retirement system, the New York state teachers’ retirement system, the New York city employees’ retirement system, the New York city teachers’ retirement system, the New York city board of education retirement system, the New York city police pension fund, or the New York
18/10 Stainless Steel New York-00 5 pc. placesetting (marked u) New York-01 Dinner Knife u 24 cm New York-02 Dinner Fork u 20.5 cm New York-03 Salad Fork u 18.8 cm New York-04 Soup Spoon (oval bowl) u 18.8 cm New York-05 Teaspoon u 15.5 cm New York-06 Cream Soup Spoon (round bowl) 17.5 cm New York-07 Demitasse Spoon 11 cm
Vincent is a Scrum Master, Agile Instructor, and currently serves as an Agile Delivery Lead at a top US bank. Throughout his career he has served as a Scrum Master and Agile Coach within start-ups, large corporations, and non-profit organizations. In his spare time he enjoys watching old movies with family. Mark Ginise AGILE ENGINEER AND COACH Mark Ginise leads Agility training for the federal .