Humana Health Plan, Inc./Humana Insurance Company: Lg Ehdhp Npos
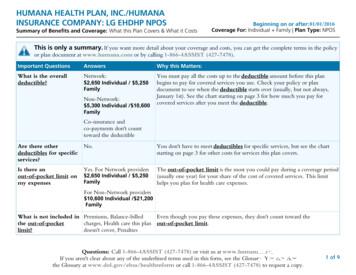
SBC0024M020120130936HUMANA HEALTH PLAN, INC./HUMANAINSURANCE COMPANY: LG EHDHP NPOSSummary of Benefits and Coverage: What this Plan Covers & What it CostsBeginning on or after: 01/01/2016Coverage For: Individual Family Plan Type: NPOSThis is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policyor plan document at www.humana.com or by calling 1-866-4ASSIST (427-7478).Important QuestionsAnswersWhy this Matters:What is the overalldeductible?Network:You must pay all the costs up to the deductible amount before this planbegins to pay for covered services you use. Check your policy or plandocument to see when the deductible starts over (usually, but not always,January 1st). See the chart starting on page 3 for how much you pay forcovered services after you meet the deductible. 2,650 Individual / 5,250FamilyNon-Network: 5,300 Individual / 10,600FamilyCo-insurance andco-payments don't counttoward the deductibleAre there otherdeductibles for specificservices?No.You don't have to meet deductibles for specific services, but see the chartstarting on page 3 for other costs for services this plan covers.Is there anout-of-pocket limit onmy expensesYes. For Network providersThe out-of-pocket limit is the most you could pay during a coverage period(usually one year) for your share of the cost of covered services. This limithelps you plan for health care expenses. 2,650 Individual / 5,250FamilyFor Non-Network providers 10,600 Individual / 21,200FamilyWhat is not included in Premiums, Balance-billedEven though you pay these expenses, they don't count toward thethe out-of-pocketcharges, Health care this plan out-of-pocket limit.limit?doesn't cover, PenaltiesQuestions: Call 1-866-4ASSIST (427-7478) or visit us at www.humana.com.If you aren't clear about any of the underlined terms used in this form, see the Glossary. You can viewthe Glossary at www.dol.gov/ebsa/healthreform or call 1-866-4ASSIST (427-7478) to request a copy.1 of 9
Is there an overallannual limit on whatthe plan pays?No.The chart starting on page 3 describes any limits on what the plan will payfor specific covered services, such as office visits.Does this plan use anetwork of providers?Yes. Seewww.humana.com or call1-866-4ASSIST (427-7478)for a list of Networkproviders.If you use a network doctor or other health care provider, this plan will paysome or all of the costs of covered services. Be aware, your network doctor orhospital may use a non-network provider for some services. Plans use theterm network, preferred, or participating for providers in their network. Seethe chart starting on page 3 for how this plan pays different kinds ofproviders.Do I need a referral tosee a specialist?No.You can see the specialist you choose without permission from this plan.Are there services thisplan doesn't cover?Yes.Some of the services this plan doesn't cover are listed on page 6. See yourpolicy or plan document for additional information about excludedservices.Copayments are fixed dollar amounts (for example, 15) you pay for covered health care, usually when you receivethe service. Coinsurance is your share of the costs of a covered service, calculated as a percent of the allowed amount for the service. Forexample, if the plan's allowed amount for an overnight hospital stay is 1,000, your coinsurance payment of 20% would be 200. This may change if you haven't met your deductible. The amount the plan pays for covered services is based on the allowed amount. If a non-network provider charges morethan the allowed amount, you may have to pay the difference. For example, if a non-network hospital charges 1,500 for anovernight stay and the allowed amount is 1,000, you may have to pay the 500 difference. (This is called balance billing.) This plan may encourage you to use network providers by charging you lower deductibles, copayments andcoinsurance amounts. 2 of 9
CommonMedical EventServices You May NeedPrimary care visit to treat aninjury or illnessYour Cost IfYou Use aNetworkProviderNo charge afterdeductibleNo charge afterdeductibleOther practitioner office visit Chiropractor:No charge afterdeductibleSpecialist visitIf you visit a healthcare provider'soffice or clinicPreventive care / screening / No ChargeimmunizationIf you have a testLimitations & Exceptions30% coinsurance 30% coinsurance Chiropractor:Chiropractor:30% coinsurance 12 visits per calendar or plan year30% coinsurance limited coverage for preventive careDiagnostic test (x-ray, blood No charge afterdeductiblework)30% coinsurance No charge afterdeductible30% coinsurance Preauthorization required, penalty may applyNo chargeafterdeductible30% coinsurance Preauthorization required, penalties may apply.(Retail)30 day supply (Retail)30% coinsurance 90 day supply (Mail Order)(Mail Order)Imaging (CT/PET scans,MRIs)If you need drugsGeneric and brand-nameto treat your illness drugsor condition(Retail)No chargeafterdeductibleMore informationabout prescriptiondrug coverage isavailable atwww.humana.com.If you haveoutpatient surgeryYour Cost ifYou Use aNon-NetworkProvider(Mail Order)Facility fee (e.g., ambulatory No charge afterdeductiblesurgery center)30% coinsurance Preauthorization required, penalty may applyNo charge afterdeductible30% coinsurance Physician/surgeon fees3 of 9
CommonMedical EventServices You May NeedEmergency room servicesIf you needEmergency medicalimmediate medicaltransportationattentionUrgent careIf you have ahospital stayIf you have mentalhealth, behavioralhealth, or substanceabuse needsFacility fee (e.g., hospitalroom)Your Cost IfYou Use aNetworkProviderNo charge afterdeductibleNo charge afterdeductibleNo charge afterdeductibleNo charge afterdeductibleYour Cost ifYou Use aNon-NetworkProviderNo charge afterdeductibleNo charge afterdeductibleLimitations & �–––30% coinsurance 30% coinsurance Preauthorization required, penalty may applyMental/Behavioral healthoutpatient servicesNo charge afterdeductibleNo charge afterdeductibleMental/Behavioral healthinpatient servicesNo charge afterdeductible30% coinsurance Preauthorization required, penalty may applySubstance use disorderoutpatient servicesNo charge afterdeductible30% coinsurance Substance use disorderinpatient servicesNo charge afterdeductible30% coinsurance Preauthorization required, penalty may applyPhysician/surgeon feePrenatal and postnatal careIf you are pregnant Delivery and all inpatientservicesNo charge afterdeductibleNo charge afterdeductible30% coinsurance 30% coinsurance 30% coinsurance 30% coinsurance 4 of 9
CommonMedical EventServices You May NeedHome health careRehabilitation servicesIf you need helprecovering or have Habilitation servicesother special healthneedsYour Cost ifYou Use aNon-NetworkProviderLimitations & ExceptionsNo charge afterdeductible30% coinsurance Preauthorization required, penalty may apply90 visits per calendar or plan yearRehabilitation:No charge afterdeductibleTherapy: Nocharge after deductibleRehabilitation:30% coinsuranceTherapy: 30%coinsurancePreauthorization required, penalty may applyPT, OT, ST, CT, AT (limit to 20 visits eachper calendar year)Habilitation: Nocharge after deductibleTherapy: Nocharge afterdeductibleHabilitation: 30%coinsuranceTherapy: 30%coinsurancePreauthorization required, penalty may applyPT, OT, ST, CT, AT (limit to 20 visits eachper calendar year)No charge afterdeductibleNo charge afterdeductibleNo charge afterdeductible30% coinsurance Preauthorization required, penalty may apply90 days per calendar or plan yearEye examNo ChargeNot �––GlassesNot CoveredNot �––Dental check-upNot CoveredNot �––Skilled nursing careDurable medical equipmentHospice serviceIf your child needsdental or eye careYour Cost IfYou Use aNetworkProvider30% coinsurance Preauthorization required, penalty may apply30% coinsurance Preauthorization required, penalty may apply5 of 9
Excluded Services & Other Covered Services:Services Your Plan Does NOT Cover (This isn't a complete list. Check your policy or plan document for otherexcluded services.) Acupuncture Bariatric surgery for morbid obesity Cosmetic surgery, unless to correct afunctional impairment Dental care (Adult), unless for dentalinjury of a sound natural tooth Private-duty nursing Hearing aids Routine foot care Infertility treatment Weight loss programs Long-term care Non-emergency care when travelingoutside the U.S.Other Covered Services (This isn't a complete list. Check your policy or plan document for other covered servicesand your costs for these services.) Chiropractic care - spinal manipulationsare covered6 of 9
Your Rights to Continue Coverage:If you lose coverage under the plan, then, depending upon the circumstances, Federal and State laws may provide protections that allowyou to keep health coverage. Any such rights may be limited in duration and will require you to pay a premium, which may besignificantly higher than the premium you pay while covered under the plan. Other limitations on your rights to continue coverage mayalso apply.For more information on your rights to continue coverage, contact the plan at 1-866-4ASSIST (427-7478). You may also contact yourstate insurance department, the U.S. Department of Labor, Employee Benefits Security Administration at 1-866-444-3272 orwww.dol.gov/ebsa, or the U.S. Department of Health and Human Services at 1-877-267-2323 x61565 or www.cciio.cms.gov.Your Grievance and Appeals Rights:If you have a complaint or are dissatisfied with a denial of coverage for claims under your plan, you may be able to appeal or file agrievance. For questions about your rights, this notice, or assistance, you can contact:Humana, Inc.: www.humana.com or 1-866-4ASSIST (427-7478)Department of Labor Employee Benefits Security Administration: 1-866-444-EBSA (3272) or www.dol.gov/ebsa/healthreformDepartment of Insurance, 311 West Washington Street, Suite 300, Indianapolis, IN 46204-2787, Phone: 317-232-2427Department of Insurance, Consumer Services Division, 311 West Washington Street, Suite 300, Indianapolis, IN 46204-2787,Phone: 317-232-2395 or 800-622-4461, Fax: 317-234-2103Does this Coverage Provide Minimum Essential Coverage?The Affordable Care Act requires most people to have health care coverage that qualifies as "minimum essential coverage."This plan or policy does provide minimum essential coverage.Does this Coverage Meet the Minimum Value Standard?The Affordable Care Act establishes a minimum value standard of benefits of a health plan. The minimum value standard is60% (actuarial value). This health coverage does meet the minimum value standard for the benefits it �–To see examples of how this plan might cover costs for a sample medical situation, see the next 7 of 9
About these CoverageExamples:These examples show how this plan might covermedical care in given situations. Use theseexamples to see, in general, how much financialprotection a sample patient might get if they arecovered under different plans.This isnot a costestimator.Don't use these examples toestimate your actual costsunder this plan. The actualcare you receive will bedifferent from theseexamples, and the cost ofthat care will also bedifferent.See the next page forimportant information aboutthese examples.Having a babyManaging type 2 diabetes(normal delivery)(routine maintenance ofa well-controlled condition)n Amount owed to providers: 7,540n Plan pays *n Patient pays *n Amount owed to providers: 5,400n Plan pays *n Patient pays *Sample care costs:Hospital charges (mother)Routine obstetric careHospital charges (baby)AnesthesiaLaboratory testsPrescriptionsRadiologyVaccines, other preventiveTotalSample care costs: 2,700 2,100 900 900 500 200 200 40 7,540Patient pays:DeductiblesCopaysCoinsuranceLimits or exclusionsTotal****PrescriptionsMedical Equipment andSuppliesOffice Visits and ProceduresEducationLaboratory testsVaccines, other preventiveTotal 2,900 1,300 700 300 100 100 5,400Patient pays:DeductiblesCopaysCoinsuranceLimits or exclusionsTotal******* Coverage Examples are not complete at this time. Example amounts for the"Patient pays" and "Plan pays" fields will be available at a later date.8 of 9
Questions and answers about the Coverage Examples:What are some of theassumptions behind theCoverage Examples? Costs don't include premiums. Sample care costs are based on nationalaverages supplied by the U.S.Department of Health and HumanServices, and aren't specific to aparticular geographic area orhealth plan. The patient's condition was not anexcluded or preexisting condition. All services and treatments started andended in the same coverage period. There are no other medical expenses forany member covered under this plan. Out-of-pocket expenses are basedonly on treating the condition inthe example. The patient received all care fromnetwork providers. If the patient hadreceived care from non-networkproviders, costs would havebeen higher.What does a CoverageExample show?Can I use Coverage Examples tocompare plans?For each treatment situation, theCoverage Example helps you see howdeductibles, copayments, andcoinsurance can add up. It also helps yousee what expenses might be left up to youto pay because the service or treatmentisn't covered or payment is limited.üYes. When you look at the SummaryDoes the Coverage Examplepredict my own care needs?Are there other costs I shouldconsider when comparing plans?ûNo. Treatments shown are justüYes. An important cost is theexamples. The care you would receivefor this condition could be differentbased on your doctor's advice, your age,how serious your condition is, andmany other factors.Does the Coverage Examplepredict my future expenses?ûNo. Coverage Examples are not costestimators. You can't use the examplesto estimate costs for an actual condition.They are for comparative purposes only.Your own costs will be differentdepending on the care you receive, theprices your providers charge, and thereimbursement your health plan allows.of Benefits and Coverage for otherplans, you'll find the same CoverageExamples. When you compare plans,check the "Patient Pays" box in eachexample. The smaller that number, themore coverage the plan provides.premium you pay. Generally, thelower your premium, the more you'llpay in out-of-pocket costs, such ascopayments, deductibles, andcoinsurance. You should also considercontributions to accounts such ashealth savings accounts (HSAs), flexiblespending arrangements (FSAs) orhealth reimbursement accounts(HRAs) that help you payout-of-pocket expenses.Questions: Call 1-866-4ASSIST (427-7478) or visit us at www.humana.com.If you aren't clear about any of the underlined terms used in this form, see the Glossary. You can viewthe Glossary at www.dol.gov/ebsa/healthreform or call 1-866-4ASSIST (427-7478) to request a copy.9 of 9
HUMANA HEALTH PLAN, INC./HUMANA INSURANCE COMPANY: LG EHDHP NPOS Summary of Benefits and Coverage: What this Plan Covers & What it Costs Beginning on or after: 01/01/2016 Coverage For: Individual Family Plan Type: NPOS This is only a summary. If you want more detail about your coverage and costs, you can get the complete terms in the policy
Humana Plans are offered by Humana Medical Plan, Inc., Humana Employers Health Plan of Georgia, Inc., Humana Health Plan, Inc., Humana Health Benefit Plan of Louisiana, Inc., Humana Health Plan of Ohio, Inc., Humana Health Plans of Puerto Rico, Inc. License # 00235-0008, Humana
MyHumana at Humana.com or by calling 1-800-233-4013. Humana group dental plans are offered by Humana Insurance Company, HumanaDental Insurance Company, Humana Insurance Company of New York, Humana Health Benefit Plan of Louisiana, The Dental Concern, Inc., Humana Medical
Humana group dental plans are offered by Humana Insurance Company, HumanaDental Insurance Company, Humana Insurance . CompBenefits Company, CompBenefits Dental, Inc., Humana Employers Health Plan of Georgia, Inc. or DentiCare, Inc. (d/b/a CompBenefits) This is not a complete disclosure of plan qualifications and limitations. Your agents will .
Why choose a Humana network provider? Humana Medicare PPO network providers must take payment from Humana for treating plan members. Network providers coordinate with Humana, which makes it easier to share information. Patients may have a better experience when providers share information this way. Humana supplies in-network .
Let’s talk about Humana Walmart Rx Plan (PDP) Find out more about the Humana Walmart Rx Plan (PDP) plan - including the drug services it covers - in this easy-to-use guide. Humana Walmart Rx Plan (PDP) is a stand-alone prescription drug plan with a Medicare contract. Enrollment in this
wellcare health insurance company of kentucky, inc wellcare ky hmo/hmopos h9870 passport health plan, inc. passport advantage ky hmo/hmopos h1951 humana health benefit plan of louisiana, inc. humana la hmo/hmopos h1961 peoples health, inc. peoples health la hmo/hmopos h3928 aetna health inc. (la) aetna medicare la hmo/hmopos
With most Humana Medicare Advantage plans, prescription drug coverage is usually built in. All questions can be answered from a knowledgeable Humana sales representative with a call to one number. 6. PROVEN TRUSTWORTHY Humana is going beyond insurance to become your partner in health. Humana is a Fortune 100 company with 60 years in the
wisdom and determination on this day of celebration. We stand on the shoulders of many clouds of witnesses. We bring to you our time, talents and money to continue the work you began with our ancestors. We stand in the middle of greater possibilities. You have carried us through many dangers, toils and snares. Eyes have not seen, nor ear heard, neither have entered the heart of men and women .