Prior Authorization And "Gold Card" Processes - NCOIL
Prior Authorization and “Gold Card” Processes National Council of Insurance Legislators November 19th, 2021
Overview Prior authorization overview Current problems Advocacy and Recommendations Gold Carding
Prior Authorization Overview Prior Authorization: Utilization management method requiring claims for services to be reviewed and approved by a health care payer before services are rendered to patients. According to America’s Health Insurance Plans (AHIP), prior authorization is implemented by health plans to help ensure patients receive optimal care based on well-established evidence of efficacy and safety, while providing benefit to the individual patient. The AHA philosophically agrees with this concept and recognizes that prior authorization, when utilized appropriately and effectively, can accomplish these goals. However, too frequently these programs create significant problems for providers as they try to deliver care.
Problems with Prior Authorization (1) Patient Care Delays/Abandonment (2) Administrative Burden
Issues with Care Access due to Prior Authorization Slow processing times delay care or lead to abandonment 2020 AMA Survey: 94% of physicians reported delays in patient care due to prior authorization. 79% reported that patients sometimes abandon treatment due to prior authorization delays. COVID-19 Public Health Emergency Significant Issues with transfers to post-acute care CMS suspended many prior authorizations and urged Medicare Advantage Organizations to do the same
Administrative Burden: Insurer requirements and submission methods Is prior authorization required for a particular service? o Specific treatments requiring authorization differs between health plans (even those issued by the same insurer). What information/documentation required for approval? o Prior authorization forms and clinical criteria used to evaluate requests varies How should the request and supporting documentation be sent to the payer? o Fax o Phone call o Portal
Prior Authorization Advocacy Prior Authorization Reform Principles (2017) Prior Authorization Consensus Statement (2018) Agency Outreach Legislative Solutions
Recommendations Standardize process Reduce timeframes Limit usage to drugs/procedures with high cost or high rate of inappropriate use Create pathways to provider exemption
AHA Asks: Standardize Standardize and Automate: Format for communicating services subject to prior authorization Format for prior authorization requests and responses within workflow Appeals processes CMS Prior Authorization Regulation (proposed Dec. 2020)
AHA Asks: Improve Usage and Timing Process improvements: Track approval/denial rates and eliminate prior authorization on services for which requests are approved over 90% of the time. Prior authorization processing 24 hours per day, 7 days per week Faster timeline for responses o Urgent Care: 24 hours o Non-urgent: 48 hours Create pathways for provider exemption
Gold-Carding Gold-carding: A process that exempts providers with a record of consistent adherence to prior authorization criteria from prior authorization submission requirements Promotes more timely access to care by eliminating unnecessary obstacles between patients and treatments. Allows health plans to focus prior authorization on providers whose patterns frequently deviate from plan criteria.
Gold-Carding Texas Law: First of its kind! More forthcoming Additional states considering legislation Improving Seniors Timely Access to Care Act Asks the HHS Secretary to develop regulations that ensure plans adopt prior authorization programs that allow for the modification of prior authorization requirements based on the performance of such providers and suppliers with respect to adherence to evidence-based medical guidelines and other quality criteria”
Questions?
Gold-Carding Gold-carding: A process that exempts providers with a record of consistent adherence to prior authorization criteria from prior authorization submission requirements Promotes more timely access to care by eliminating unnecessary obstacles between patients and treatments. Allows health plans to focus prior authorization on
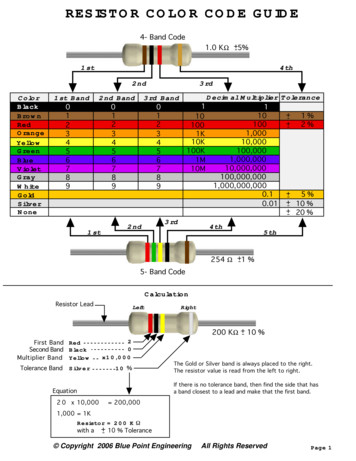
.56 ohm R56 Green Blue Silver.68 ohm R68 Blue Gray Silver.82 ohm R82 Gray Red Silver 1.0 ohm 1R0 Brown Black Gold 1.1 ohm 1R1 Brown Brown Gold 1.5 ohm 1R5 Brown Green Gold 1.8 ohm 1R8 Gray Gold 2.2 ohm 2R2 Red Red Gold 2.7 ohm 2R7 Red Purple Gold 3.3 ohm 3R3 Orange Orange Gold 3.9 ohm 3R9 Orange White Gold 4.7 ohm 4R7 Yellow Purple Gold 5.6 ohm 5R6 Green Blue Gold 6.8 ohm 6R8 Blue Gray Gold 8 .
Gold 6230 2.1 20 27.5 10.4 Y 125 Gold 6226 2.7 12 19.25 10.4 Y 125 Gold 6152 2.1 22 30 10.4 Y 140 Gold 6140 2.3 18 25 10.4 Y 140 Gold 6130 2.1 16 22 10.4 Y 125 Gold 5220 2.2 18 24.75 10.4 Y 125 Gold 5218R 2.1 20 27.5 10.4 Y 125 Gold 5218 2.3 16 22 10.4 Y 105 Gold 5217 3 8 11 10.4 Y 115 Gold 5215 2.5 10 13.75 10.4 Y 85 Gold 5120 2.2 14 19 10.4 Y .
Cards on KSU 64 If card is a Loop card 64 If card is a T1 card 64 If card is a PRI card 65 If card is an ETSI PRI card 66 If card is a DID card 66 If card is an E&M card 66 If card is a BRI-U2, BRI-U4 or BRI-ST card 66 If
A. Perfect Pair letterpress folded card: SS-01 B. HEY GIRL HEY flat card with gold foil: SS-02 C. Splatter paint flat card with gold foil: SS-03 D. Cheers confetti flat card with gold foil: SS-04 E. Thank You folded card with gold foil: SS-05-Teal F. Thank You folded card with gold foil: SS-05-Blush G. Than
4 For services described in this policy, see below for products where prior authorization might be required if the procedure is performed outpatient. Outpatient Commercial Managed Care (HMO and POS) Prior authorization is not required. Commercial PPO and Indemnity Prior authorization is not required. Medicare HMO BlueSM Prior authorization is not required.
Jane Doe with authorization code 654321 and authorization level 2 . Joe user with authorization code 999999 and authorization level 1 . Step 2.-Configuring Forced Authorization Codes . Go to the administration page of Cisco Unified Comm unications Manager, select Call Routing TAB, then select Force Authorization Codes as shown in the image s below.
From Land to Sea stamp set (A card 1) Fresh Fruit stamp set (A card 1, B card 1, C card 1) Sprinkles of Life stamp set (A card 2) Balloon Builders stamp set (B card 1, C card 1) Thankful Thoughts stamp set (B card 2) No Bones About It stamp set (C cards 3 & 4, D card 2) Tin of Card stamp set (C card 4) Stylized Birthday
Titulli I diplomuar në administrim publik Numri në arkiv i akreditimit [180] 03-619/9 Numri në arkiv i akreditimit [240] 03-1619/19 (10.11.2017) Vendimi për fillim me punë 03-1619/19 (10.11.2017) Data akreditimit 21.03.2017 Përshkrimi i programit Programi i administrimit publik ka një qasje multidisiplinare të elementeve kryesore të studimit në fushën e Administratës publike dhe .