Evidence From NHS Improvement On Clinical Staff Shortages
Evidence from NHSImprovement on clinicalstaff shortagesA workforce analysisFebruary 2016
About NHS ImprovementNHS Improvement is responsible for overseeing foundation trusts, NHS trusts andindependent providers. We offer the active support these frontline providers need togive patients consistently safe, high quality, compassionate care within local healthsystems that are financially sustainable. By holding providers to account and, wherenecessary, intervening, we help the NHS to meet its short-term challenges andsecure its future.NHS Improvement brings together Monitor, the NHS Trust Development Authorityplus groups from three other organisations: from NHS England both the PatientSafety Team and the Advancing Change Team, from NHS Interim Management andSupport two Intensive Support Teams, together with the National Reporting andLearning System. NHS Improvement is an operational name for the organisationwhich formally comes into being from 1 April 2016.2
ContentsSummary . 41. Background . 62. What has happened to the nursing workforce? . 62.1. Nursing demand has risen rapidly and is outstripping supply . 62.2. Nurse demand has risen partly because of increasing activity, but alsoas a result of safe staffing . 92.3. Providers have responded to the supply shortage in large measure byhiring agency workers, driving up agency costs . 142.4. Improvements in providers’ productivity have moderated the additionaldemand for nurses and the increase in agency spend . 143. What has happened to the consultant workforce? . 153.1. The number of consultants has increased faster than activity . 153.2. Demand is outstripping supply in some key specialties . 164. NHS Improvement’s plan to help providers respond to workforce shortages . 174.1. Supporting local action by providers . 184.2. National actions to support local responses . 193
Summary11.There has been a rapid rise in demand for hospital nurses since publication ofthe Francis Report in February 2013 and the push for higher staffing levels thatfollowed. For example, hospitals’ demand for nurses caring for adult acutepatients in 2014 was 189,000, around 7,000 more than hospitals had beenforecasting just a year earlier and 24,000 more than was forecast two yearsbefore. Taken together, trusts’ current forecasts anticipate further growth in thenursing workforce.2.Rapid growth in the number of nurses employed over the last two-and-a-halfyears has resulted in an increase in the ratio of nurses to patients in hospitals.However, the recent increase has only returned this ratio to where it stood at theend of 2011 (see figure below).Trends in nurse-to-patient ratio, admissions and length of stay 2010 to 201523.The supply of nurses has failed to keep up with this rapid growth in demand.Hospitals estimate they are 15,000 nurses3 short of what they need. Asignificant element of this supply shortfall can be ascribed to the collapse in thenumber of nurses from outside the European Economic Area joining the NHS1Analysis correct as at October 2015.Substantive nurses only.3Nurses trained to care for adults and working in both the acute and the community sectors.24
each year. This figure has fallen by over 95% from its peak of more than 15,000in the early 2000s.4.Inevitably, this significant supply shortfall has driven up the cost of agencynurses. Agency charges for nurses increased by around 30% from 2012 to2015.5.Nevertheless, the nurse shortfall would be even worse were it not forproductivity improvements made by trusts over the last two years. In particular,reductions in average length of stay have offset a sharp increase in hospitaladmissions (see figure above). Without this improvement, there would likely bea need for around 5,000 extra nurses at a cost to the NHS of about 250 millionat agency rates.46.We are supporting local workforce initiatives and working with system partnersto rebalance supply and demand at the national level. Our actions include:4 supporting providers on workforce planning and improving co-ordination at anational level building on the work of the Carter Review to improve provider productivity reducing providers’ agency costs.Our calculation is based on NHS Professionals’ observed rate for a band 5 nurse in 2014/15.5
1. BackgroundThe NHS as a whole directly employs over 640,000 people in the professionallyqualified clinical workforce, including 110,000 doctors and over 315,000 nurses.5Spending on total workforce represents an estimated 70% of a typical hospital’s6costs, with much of this spent on the clinical workforce.7 The right workforce iscrucial to ensuring the quality of care that hospitals provide. It is also central tomaking the productivity and efficiency gains needed to meet their financialchallenges, and transforming services through new care models.Growing shortages of qualified clinical staff have led providers to make increasinguse of agency and other temporary workers to fill vacancies. We have recentlyintroduced new rules on agency workers to help providers address the impact of thistrend on their costs.This report sets out our analysis of the causes and extent of current clinical staffshortages in acute hospitals, focusing on adult nurses8 and consultants.9 Its aims areto provide evidence informing decisions about the sector at a national level,10 and tohighlight some of the materials we are developing to support providers. Further, thereport sets out the actions we will take at a national level with our system partners tosupport providers facing workforce shortages.2. What has happened to the nursing workforce?2.1. Nursing demand has risen rapidly and is outstripping supplySince the end of 2012, there has been a large increase in demand for hospitalnurses across the NHS. In 2014, providers reported to Health Education England(HEE)11 that they needed 189,000 adult nurses12 (acute) in total, yet two yearsearlier they predicted they would need only 165,000; in 2013, this had risen to over180,000 (see Figure 2).5Health and Social Care Information Centre NHS workforce statistics – June 2015, files/kf/field/field publication .pdf7According to NHS Employers, 50.6% of NHS employees are professionally qualified clinical staff orce-in-numbers8‘Adult nurses’ in our analysis refers collectively to all nurses caring for adult acute, elderly and adultgeneral patients.9Other areas and specialties, such as general practice, may also be experiencing shortages but areoutside the scope of this study.10Analysis correct as at October 2015.11HEE asks providers for their forecast workforce demand each year.12HEE defines adult nurses differently from us as it bases its definition on training branches. Wherewe cite HEE adult nursing data, we indicate whether the data are for nurses working in the adultacute and/or community sector.6
This rise in demand is reflected in the increasing numbers of nurses employed.Between October 2012 and April 2015 the number of adult nurses employed grew by10,000 full-time equivalents (FTEs) or 6.4% (see Figure 1).However, demand still exceeds supply. HEE’s data indicate that providers had15,489 FTE vacancies for adult nurses (both those working in the acute and thecommunity sector) in April 2014, equivalent to a 6.5% vacancy rate.13 At that time,trusts also indicated to HEE that they expected to need a further 6,389 nurses in2014/15.14Figure 1: Qualified adult nursesemployed in the NHSFigure 2: Numbers employed andforecast demand for adult nurses(FTE) working in the acute sectorSource: HSCICSource: HEEOne factor contributing to continuing high vacancy levels is the drop in recruitment ofnurses from outside the European Economic Area (EEA). International recruitmenthas historically helped fill gaps between predicted and actual demand for nurses,and since 2009 the number of nurses coming to the UK from the EEA has increased.However, the number of nurses who join the UK nursing register from outside theEEA has declined substantially. As shown in Figure 3, in the early 2000s, 12,000 to15,000 non-EEA nurses joined the UK nursing register each year. From 2008/09 to2014/15 this number fell to around 1,000 nurses a year, and in 2014/15 only 665non-EEA nurses were registered.1314HEE Workforce plan for England 2015/16 – note that the vacancy figure is as at 1 April 2014.Overall requirements are predicted to increase by 5,642 FTE in 2019. Increases in 2014/15 arepredicted to be followed by reductions between 2015 and 2019. HEE Workforce plan for England2015/16.7
Figure 3: New registrations on the Nursing and Midwifery Council registeraccording to EEA and non-EEA originSource: RCN (2015) International recruitment 2015More generally, the supply of UK-trained nursing staff is slow to respond to demandchanges. In the NHS, as in many other health systems,15 the future supply of nursesis planned centrally. Training a nurse takes more than three years. So when demandrises considerably and rapidly, the supply of trained nurses available to fill hospitals’substantive (ie permanent) nursing posts cannot easily respond at the same pace.The increase in demand has also come at a time when fewer nurses are qualifying –between 2010/11 and 2012/13 the number of nursing training places fell by 12.7%from 20,092 to 17,546.16Return-to-practice schemes are another means of expanding supply. The centrallyfunded return-to-practice initiative between February 1999 and March 2004 resultedin 18,500 former nurses and midwives returning to work in the NHS.17 However,recent schemes have not had the same level of success – around 1,300 nursessigned up to HEE’s most recent scheme.15See, for example, King’s Fund (2009) NHS workforce planning: limitations and -practice.pdf168
The increase in demand for nurses appears to be continuing. In July 2015, 75% ofNHS trust finance directors indicated they planned to increase their permanentnursing staff in the next six months.182.2. Nurse demand has risen partly because of increasing activity, but also asa result of safe staffingThree main factors may drive changes in hospitals’ demand for nurses. The first isexpected levels of activity: the more patients that hospitals expect to admit, the morenurses they will need. The second is those patients’ levels of sickness (or acuity): ahigh proportion of seriously sick patients will need more nursing hours. Lastly, sectorreports and new policies concerning staffing levels can change demand for nurses.The Mid Staffordshire NHS Foundation Trust Public Inquiry’s findings (the FrancisReport) were published in 2013. The report was commissioned after serious failingsat the trust. One recommendation was to create tools to establish the safe staffingneeds of each service. The National Institute for Health and Care Excellence (NICE)then developed safe staffing guidelines for hospital wards.19 Although the NICEguidance does not specify a staff-to-patient ratio, it suggests that patients are atincreased risk of harm if a nurse regularly has to care for more than eight patients ona ward during the day.20 In addition, in 2013 the National Quality Board (NQB)published guidance setting out expectations of hospitals’ nursing staff capacity andcapability. The Care Quality Commission’s (CQC’s) inspections also assess whetherstaffing is safe. We refer to the Francis Report, NQB guidance, NICE guidelines andtheir use alongside the CQC inspection regime collectively as ‘safe staffing’.We have tested whether safe staffing has been a cause of the recent increase indemand for nursing staff. It is difficult to disentangle its effects on nurse demandfrom the other two causes – activity and levels of sickness.21 However, the stepchange in demand in the period after publication of the Francis Report in early 2013indicates that safe staffing has had a strong impact on acute hospitals’ demand fornursing staff, specifically:18Response to the question: ‘Is your organisation planning to increase the number of permanentnursing staff in the next six months?’ King’s Fund Quarterly Monitoring Report July 2015 –http://qmr.kingsfund.org.uk/2015/16/19Safe staffing timeline, key milestones: Francis Report, February 2013 National Quality Board Guidance 2013 – ow-to-guid.pdf guidance on publishing staffing data monthly from April 2014 –www.england.nhs.uk/2014/04/01/hard-truths/ NICE safe staffing guidelines, July 2014 – endations (July 2014).21In addition, here we have not controlled for any other aspects of quality.9
As highlighted above (Figure 1), there was a sudden upturn in employment ofadult nurses from early 2013. It increased by 4.6% from January 2013 toJanuary 2015. Providers revised upwards their forecasts for the number of adult nurses theywould need to meet 2014 demand (Figure 2). The ‘nurse-to-patient bed day ratio’ (a measure we have developed to showthe intensity of nursing care – see Box 1) shows an increase from January2013 to January 2015, driven by providers employing greater numbers ofnurses. The increase was about 4% when the ratio includes only substantivenurses and an estimated 6% when agency nurses are included.The increase in the nurse-to-patient bed day ratio after the Francis Report followed aperiod when the ratio had been falling (see Box 1). More recent increases havereturned the ratio to its December 2011 level. This has coincided with rising numbersof admissions, making it harder to maintain the ratio than it was in 2011.Box 1: Nurse-to-patient bed day ratioTo assess the impact of safe staffing on demand for nursing staff, we havedeveloped a new measure of the intensity of nursing care – the ‘nurse-to-patientbed day ratio’.22 This ratio increases when there are more nurses for each patientin hospital at any particular time.23 The number of ‘patient bed days’ is the numberof admissions multiplied by their length of stay, so we express the ratio as:FTE nursesAdmissions average length of stayChanges in each of its three elements affect the ratio: it will rise if either thenumber of nurses increases or admissions fall or length of stay falls.This measure reflects the volume of patients in hospital at any one time and soaims to capture the amount of nursing care they receive. However, it doesn’tcompletely capture the time patients spend (or need) with nurses because: As well as capturing nurses’ contact time24 with patients, it also capturesnurses’ time spent on activities that are not classified as direct patient care.We are not aware of evidence that the time nurses spend on either type of22Estimated using inpatient admissions and length of stay data from the Hospital Episode Statistics,the number of substantive adult, general and elderly nurses from the electronic staffing record, andan estimate of agency nurse use from our agency survey 2014/15.23This could be more fully referred to as ‘acute, general and elderly nurse FTE per bed days within acalendar month in acute settings’.24An example of how nursing activity can be defined can be found in Appendix A of NHS England’sGuide to care contact time – r-staffingguide-care-contact-time.pdf10
work has changed significantly over the period, although we might expectproviders to have responded to safe staffing by increasing care contact timeper patient for each nurse in the ways described by NHS England.25It does not capture differences in different patients’ needs for nurse time.For example, a higher prevalence of patients with dementia in a hospitalwould lead to a higher overall patient need for contact time.Changes in components of the ratio FTE nurses. We described the upward trend in nurse numbers above. Patient bed days (ie admissions average length of stay). As Figure 4 shows,changes in the bed days’ component can be split into three periods. In periodone, it fell as length of stay reduced faster than admissions grew. In period two,it started to rise, as admissions also rose and length of stay reductions stalled.In period three, it remained constant, as increases in admissions and reductionsin length of stay cancelled each other out.Figure 4: Breakdown of patient bed days, 2010 to 2015Source: Estimated using inpatient admissions and length of stay data from the Hospital EpisodeStatistics, the number of substantive adult, general and elderly nurses from the electronic staffingrecord. Twelve-month moving averages used to account for seasonal fluctuations.25NHS England Safer staffing: a guide to care contact time – -staffing-guide-care-contact-time.pdf11
The impact of changes on the ratioFigure 5 below shows how changes in the ratio’s components contributed tofluctuations in the ratio itself between 2010 and April 2015. The number of nursesis shown in green and the number of patient bed days in blue. Before publicationof the Francis Report in February 2013, changes in the ratio were mainly driven bychanges in patient bed days as adult nursing numbers remained broadly flat overthe period (although overall nursing26 numbers were falling slightly at this time).However, from February 2013 onwards (period three), when we might expect tostart seeing an impact from safe staffing, increases in nursing numbers drove theincrease in the ratio. The number of patient bed days stayed broadly constant, butthe nurse-to-patient bed day ratio increased by 4% because trusts were employingmore substantive nurses. This is consistent with trusts implementing safe staffingin the wake of the Francis Report by increasing their nursing levels, bringing thenurse-to-patient bed day ratio back up to the levels of September 2011.Figure 5: Nurse-to-patient bed day ratio, 2010 to 2015 (substantive nursesonly)Source: Estimated using inpatient admissions and length of stay data from the Hospital EpisodeStatistics, the number of substantive adult, general and elderly nurses from the electronicstaffing record. Twelve-month moving averages used to account for seasonal fluctuations.26Qualified nursing, midwifery and health visiting staff.12
Including changes in agency nurse useIncluding only numbers of substantive nurses in the nurse-to-patient bed day ratiois likely to underestimate actual changes in the ratio. We know that demand foragency nurses increased rapidly over period three. Figure 6 shows that overallagency spend fell in periods one and two but rose significantly following theFrancis Report. Including an estimate of the increase in employment of agencynurses from Q1 2012/1327 in the ratio shows it may have grown by around 6% overthis two-year period.Figure 6: Nurse-to-patient bed day ratio (including agency) and agency spend,2009 to 2015Source: Estimated using inpatient admissions and length of stay data from the Hospital EpisodeStatistics, the number of substantive adult nurs
6 1. Background The NHS as a whole directly employs over 640,000 people in the professionally qualified clinical workforce, including 110,000 doctors and over 315,000 nurses.5 Spending on total workforce represents an estimated 70% of a typical hospital’s6 costs, with much of this spent on the clinical workforce.7 The right workforce is crucial to ensuring the quality of care that hospitals .
bunchberry dr nhs wms amb . burgundy ln nhs wms twl . burkwood dr nhs wms amb . burning tree st chs wms twl . burnock dr chs wms mbe . burr ridge rd nhs nms twl . burrwood ave nhs nms ang . burrwood st nhs nms ang . burt dr chs cms lce
of NHS Direct, and led the team preparing New Labour's first White Paper, The New NHS: Modern, dependable, which laid the foundations and structure for the current NHS reform programme. He was a member of the top management board of the NHS for 12 years, between 1988 and 2000. His earlier career included 23 years in NHS management,
Currently working to align with work on RightCare'sFrailty Pathway and the Geriatric Medicine workstream of NHS Improvement's Getting It Right First Time (GIRFT) programme . NHS RightCare is a programme of NHS England Piers Glen NHS RightCare Delivery Partner 8 bpollington@nhs.net 07710 152763. Title: PowerPoint Presentation
It is now referenced in the Mandate to NHS England, the NHS Planning Guidance and the CCG Improvement and Assessment Framework. The RightCare programme includes the Commissioning for Value packs and tools, the NHS Atlas series and a number of casebooks. NHS England has committed significant funding to rolling out the RightCare
NHS Long Term Plan Implementation Framework I 3 Introduction to the NHS Long Term Plan Implementation Framework 1.1 The NHS Long Term Plan, published in January 2019, set out a 10-year practical programme of phased improvements to NHS services and outcomes, including a
allowances are known as NHS Bursaries’1 and apply to courses qualifying students for certain professions (see Professions with training funded by NHS Bursaries). Students wishing to undertake these courses apply for an NHS bursary instead of Student Finance. NHS Bursaries are award
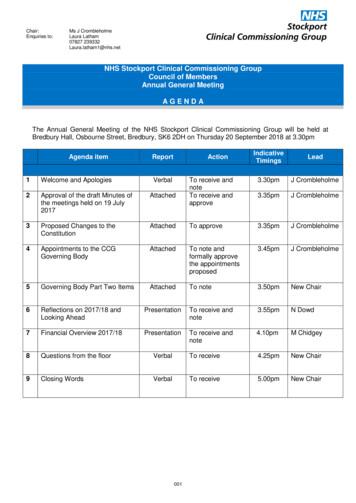
Dr Ranjit Gill . Chief Clinical Officer . NHS Stockport CCG . John Greenough . Lay Member . NHS Stockport CCG . Louise Hayes . Head of Communications and Engagement NHS Stockport CCG . Diane Jones . Director of Service Reform . NHS Stockport CCG . Dr Deborah Kendall .
Patient rights and NHS promises. 13. Part 4 - The things patients should do to help. 27. Part 5 - Rights and promises the NHS makes for NHS staff. 29. Part 6 - The things staff should do to help. 33. Part 7 - Telling the NHS