Decon Binder - STRAC
INGDECONTAMINATION
Table of ContentsInstructor Manual1.2.3.4.5.Class Planning “To Do” list andOHSA Respiratory QuestionnairetemplateClass Agenda, Certificate,Sign-In and Evaluation, CourseObjectivesSlides and Lecture TextClass Handoutsa. Pretestb. Skills Station Check Listsi. PPEii. Patient Deconiii. Decon EquipmentInformation submitted to STRAC
1
Hospital First ReceiverTraining Guide4 Weeks Prior:1. Confirm class date with site coordinator and STRAC2. Coordinate with correct number of faculty and adjunct facultyneeded to have 4:1 ratio for skills station3. Ensure CEUs through STRAC2 Weeks Prior:1. Coordinate with STRAC and site coordinator equipment forskill stations (i.e., PPE and shower)2. Send out reminder notice1 Week Prior:1. Make copies of class handouts2. Confirm additional faculty and adjunct faculty assistance3. Offer assistance to site coordinator for RespiratoryQuestionnaire processFollow-up:1. Submit evaluations to STRAC2. Give copies of roster, tests and skill checklist for sitecoordinator, keep one set for files3. Submit expenses to STRAC
Hospital First ReceiverTrainingAgendaDate:Facility:Welcome, Introductions and Expectations8:00 a.m. – 8:30 a.m.Lecture8:30 a.m. – 9:45 a.m. Purpose of Training Hazardous Agents Response Patient Decontamination Decon / Disaster Response Team Roles and Responsibilities Personal Protective EquipmentBREAK9:45 a.m. – 10:00 a.m.Lecture (continued)10:00 a.m. – 11:00 a.m.LUNCH11:00 a.m. – 12:00 p.m.Decon Response Skills Training Decon Operations Setup (15 min rotations) Connecting the water supply Connecting the electric supply Setting up the tent Using the Ludlum rate meter Donning and Doffing PPE w/ Respirator Use Full Face-Masks with CBRNE cartridges Powered Air Purifying Respirators (PAPRs)12:00 p.m. – 1:00 p.m.1:00 p.m. – 1:45 p.m.1:45 p.m. – 2:15 p.m.BREAK2:15 p.m. – 2:30 p.m.Skills Station Cont.2:30 p.m. – 4:30 p.m.Closing and Evaluation4:30 p.m. – 5:00 p.m.
Certificate of CompletiontoforSuccessfully completing the Hospital FirstReceiver’s Training for DecontaminationPresenter Name and TitleDate
Hospital First ReceiverTrainingSign-In 13.14.15.16.17.18.19.20.Department
Hospital First ReceiverTrainingEvaluationDate:Facility:We hope that your class was fun, yet, informative. However, we continually striveto provide you with quality information that benefits you as a healthcareprofessionalPlease rate the following, on a 1-5 scale (1 being the worst, 5 being the best)Class format12345Organization of information12345Class content meets expectations12345Class content was helpful12345Educator’s preparation level12345Instructor’s communication skills12345Instructor’s knowledge level12345What did you like best about this class?What did you like least about this class?Do you have any suggestions for improving the class?Additional comments:
Hospital First Receiver CourseObjectivesPurpose of Decontamination Response Teams1.Describe the risks and problems for healthcare systems that can occur withhazardous materials incidents2.Explain exposure3.Explain contamination4.Define decontamination5.Explain the purpose of a hospital/healthcare facility decontaminationNeed for Decontamination Response Teams6.Identify hazardous materials7.Define the process for maintaining personal safety during a hazardousmaterials incidentDecontamination Response8.Define Directed Self Decon9.Explain the process of Directed Self Decon10.Demonstrate the procedure for Directed Self Decon11.Define Decontamination Response Team12.Differentiate between the need for directed self decon and decontaminationresponse team initiation13.Define the roles and responsibilities of members of a DecontaminationResponse Team14.Explain the process for decontaminating a patient15.Identify the role of a greeter16.Demonstrate the role of a greeter17.Identify the role of a stripper/bagger18.Demonstrate the role of a stripper/bagger19.Explain the process for proper collection of patient belongings20.Explain the process for proper disposal of patient belongings21.Demonstrate the process for proper collection and disposal of patientbelonging22.Identify the role of a washer/rinse
Hospital First Receiver CourseObjectivesDecontamination Response23.Demonstrate the wash-rinse process for an ambulatory patient24.Demonstrate the wash-rinse process for a non-ambulatory patient25.Identify the role of a dryer/dresser26.Demonstrate the role of a dryer/dresser27Identify the role of a hospital gatekeeper28.Demonstrate the role of a hospital gatekeeper29.Explain the purpose of performing self-decon once decontaminationactivities have ceased.Personal Protective Equipment30.Identify proper personal protective equipment for decontaminationresponse31.Verbalize the limitations of personal protective equipment32.Explain the importance of correctly using personal protective equipment33.Explain the dangers associated with using personal protective equipment34.Demonstrate how to don personal protective equipment35.Demonstrate proper self-decon36.Demonstrate how to doff personal protective equipment37.Demonstrate the hand signal used to say „I need help/assistance with thispatient.‟38.Demonstrate the hand signal used to say „I‟m having trouble breathing.‟39.Demonstrate the hand signal used to say „I‟m O.K.‟40.Explain the process for addressing Decontamination Response Teammembers in distress
2
2014HospitalDecontaminationResponse Teams1
2014Your Facility InformationPresented by 2
2014Class ScheduleBreaksRefreshment availabilityRestroomsAnd please turn your cell phones andpagers off or to silentWelcome andIntroductions3
2014IntroductionSection I4
20145 Develop an understanding of hazardoussubstances in an emergency Develop an understanding of the role of the FirstReceiver Develop an understanding of the selection onuse of Personal Protective Equipment (PPE) Develop an understanding of detection devicesand decontamination equipment Develop an understanding of basicdecontamination proceduresCourse Objectives
2014 People who have been contaminated byhazardous agents may arrive at the hospital formedical treatment An estimated 33% of persons from a hazmatincident will bypass EMS and self present athospital. We do not want to compromise the safety of ourstaff or our facility by exposing them tohazardous agentsWhy are we here?6
2014– To you?– To the emergency department?– To the hospital?– To the community? What are the impacts:7If a contaminatedperson is allowedinside our facility
2014Employee exposureand hospital closure iswhat we want to avoid!8
2014 Exposure:A person has been in the area of acontaminate (generally a vapor) Contaminated:A person has come in contact with acontaminate (generally a liquid or solid)Exposure vs.Contamination9
InhalationIngestionAbsorptionInjection2014 Precautions, decontamination, and treatmentoptions may vary based on exposure.–––– Exposure routes include:How does a personbecome exposed?10
2014Home Chemical ExposuresAgricultural ExposuresTransportation SpillsIndustrial SpillsWeapons of Mass Destruction11How does a personbecomecontaminated?
201412 While it has manydefinitions, it is a methodfor cleaning offcontaminated patients Decontamination reducesand prevents the spread ofhazardous agents toemployees and within thefacilityWhat isdecontamination?
2014Hazardous AgentsSection II13
201414According to OSHA: Any substance to whichexposure “results or may result in adverseaffects on the health or safety ofemployees” or “any chemical which is aphysical hazard or a health hazard.”OSHA 29 CFR 1910.120 (a)Hazardous Agents
2014Class 1 – ExplosivesClass 2 – Compressed GasesClass 3 – Flammable LiquidsClass 4 – Flammable SolidsClass 5 – Oxidizers and Organic PeroxideClass 6 – Poisons or Infectious MaterialsClass 7 – Radioactive MaterialsClass 8 – Corrosive MaterialsClass 9 – Miscellaneous15Hazardous Agents
2014– Liquids or powders on the patient– Odors emanating from the patient– Difficulty breathing– Burns, blisters– Foaming at the mouth or tearing– Emesis, defecation, urination Obvious physical signs and symptoms ofhazardous agent exposure:How do you know if apatient has beenexposed?16
201417 Several patients who present with similarsymptoms Patients who present from the same eventor location– Have traveled out of the country– Exhibit unusual signs and symptoms– Are very sick Patients who:Bioagents - what tolook for in triage
2014– Mixed chemicals at home or work18 Initial reports from the patient or EMS maynot indicate exposure Ask questions – complete a thorough andaccurate assessment Patient may not understand that they havebeen exposedDon‟t be deceived!
2014 Smart Strips - Changes colorswhen exposed to chlorine, pH,fluoride, nerve agents,oxidizers, arsenic, sulfides andcyanide in liquid or aerosolform at minute levels. To use,peel-and-stick adhesive stripor a clip to decon suit. Oncethe protective film is peeled off,the cards are operational for12 hours, or until they areexposed to one of the eightsubstances.CHEMICALMethods of detection:19
Personal Pocket DosimeterDetects Beta andGamma RadiationPortalsPortable andExpandable!201420Pancake Probe(Ludlum) detectsAlpha, Beta andGamma radiationRADIOLOGICALMethods of detection:
C ChemicalB BiologicalR RadiologicalN NuclearE ExplosivesCBRNE:2014Weapons of MassDestruction (WMD)21
201422AnthraxBotulismPlagueSmallpoxTularemiaViral Hemorrhagic Fever (VHF)Infectious Respiratory Disease (SARS or AvianFlu)Biological Agents
2014FeverHeadacheRashNeck stiffnessRespiratory symptomsSigns and Symptomsof exposure tobiological agents23
2014– Sunlight and natural elements– X-rays– Nuclear medicine procedures– Cancer-related radiation treatments– Industry Found in:24Where can Radiationbe Found?
201425 Alpha particles (common) - most harmful ifinhaled or ingested. These can be stopped by asheet of paper. Beta particles - smaller than alpha and stoppedby regular PPE. Gamma/X-ray – not a particle and can penetrateskin and tissue. Will penetrate most PPE. Neutrons – found in nuclear reactions, canpenetrate skin and tissue, cannot be stopped byPPE.Radiological
2014Radiation Exposure26
2014 External contamination occurs whenparticles come in contact with the skin Minimal exposure risk to care giver. Treatacute injury first!– Acute radiation sickness Internal contamination may result whenparticles are ingested or inhaled.RadiologicalContamination27
Respiratory Contact2014Time – Limit exposure timeDistance – Increase distance from sourceShielding – Shield self from the hazardPPE – Use Standard Precautions28Radiation Protection
Nerve AgentsBlister AgentsBlood AgentsChoking AgentsIrritant Agents2014Chemical Agents29
2014S – Salivation (drooling)L – Lacrimation (tearing)U – Urination (loss of bladder control)D – Defecation (loss of bowel control)G – Gastrointestinal (abdominal pain)E – Emesis (vomiting)M – Miosis (pinpoint pupils)– Affect the body‟s nervous system– Signs and symptoms:Nerve agents (pesticides/military agents)Nerve Agents30
2014– Affect the body‟s ability to transport and useoxygen– Examples include cyanideBlood Agents:– Cause burns and blisters– Examples include mustard gas and LewisiteBlister Agents:Chemical Agents31
201432– Cause a person to become incapacitated– Examples include tear gas, mace, and peppersprayIrritants:– Damage lung tissue and mucous membranes– Examples include phosgene and chlorineChoking Agents:Chemical Agents
2014ResponseSection III33
S ShieldI IsolateN NotifyS-I-N201434If a contaminated personpresents to the hospital,what do you do?
201435– Protect yourself by using standardprecautions– Do not touch the patient or allow anyone elseto have patient contact without at least an N95 mask and glovesDon‟t become part of the problem SHIELD
201436 Get the contaminated patient out of thefacility to a pre-designated location If someone has something on them, don‟tlet them go away Isolate the exposed scene and deny entryuntil hazard assessment is completed andarea is cleaned, if neededISOLATE
2014 Work with your Supervisor to determineyour facility‟s need to activate theDecontamination Response Team (DRT)or initiate disaster response procedures– Security should wear appropriate PPE whilesecuring the area.37 Notify your Supervisor that a contaminatedpatient has arrived at the facility If needed, call Security to secure the areaNOTIFY
201438 A contaminated non-ambulatory patientpresents to the facility More contaminated patients present to thefacility than can be managed by staff onsite A Mass Casualty Incident (MCI) has beendeclared in your communityActivation of theDecontaminationResponse Team
––––––––2014Maintain Safe Environment – Safety Officer and RSODecon Set Up / Support – Team LeaderSite Access Control - SecurityTriage – Nurse or PhysicianStripper / BaggerWasher / RinserDryer / DresserHospital Gatekeeper39 A trained group of personnel with resources to operatein a contaminated area and perform the followingfunctions:What is aDecontaminationResponse Team?
– Team debriefing2014 Ensure the safety of the facility and personnel Setup of decon operations Triage, reassure and direct contaminated patientsthrough the process Perform decontamination procedures Recovery operations:– Equipment cleaning– Management of wastewater40Duties of DRT Membersin the HospitalDecontamination Zone
201441Hospital DecontaminationZone
Hospital GatekeeperCOLDWasher / RinserDryer / DresserWARMStripper / BaggerHOTSite Access ControlSTART Triage2014– Safe area– Use Standard Precautions Hospital Post-Decontamination ZoneCOLD42– Area where decontamination activitiestake place– MUST use appropriate hazardousagent PPEWARM Hospital Decontamination Zone– Area of isolation– MUST use appropriate hazardousagent PPE Contaminated Area HOTControl Zones –ContaminationReduction Corridor
– Up Hill– Up Wind– Up Stream201443 To ensure that the agent does notcontaminate the „clean‟ area, set-updecontamination activities so that they are:HospitalDecontamination Zone
2014Secure the areaEstablish a perimeterEstablish control zonesInitiate crowd control measuresEnsure proper PPE is worn and safetyprocedures are followed44Ensure the Safety of theFacility and Personnel
201445 Establish Decontamination Zone Access decontamination supplies Assemble the decontamination shelter andadjunct equipment Ensure access to contaminated waste forease of removal during decon operations EPA requires run-off be contained if at allpossible for proper disposalSetup of DeconOperations
TriageStationHOT ZONEArrivalPoint2014WARM minationCOLD ZONECleanTriageArea46Our Hospital‟s DeconSet-Up
2014 Utilize START (Simple Triage and RapidTreatment) Explain the decontamination process Collect contaminated belongings47Triage, Reassure andInstruct ContaminatedPatients
Focus on doing themost for the most Utilize START Triagemethod2014Triage during aMass CasualtyIncident48
Separate clothing andvaluables Place in transparent andsealable collection bags Label clothing andvaluables for tracking,retrieval and investigationpurposes2014Collection ofcontaminatedbelongings49
2014 Consider patient modesty– Use Standard Precautions– May require use of hazardous agent PPE50 Appropriate for conscious and ambulatorypatients Directed decon can be used for smallnumbers of contaminated patients Protect yourself first:Directed Decon
2014– Have patient dry their body– Provide patient with a clean covering– Re-evaluate patient Wash body with soap and warm water for 5 minutes Rinse body with warm water for 5 minutes– Have patient remove all valuables and clothing– Place contaminated valuables and clothing in asealable bag– Starting from the head down, have patient:51Process for PerformingDirected Decon
2014Decontamination of NonAmbulatory Patients“Assisted Decon”52
2014ChildrenInfantsDisabledService AnimalsLaw EnforcementDeceased IndividualsOther Special Needs53Special Populations
2014 Parents Ease fears Decon parent andchild Extend rule of thumbtime Additional assistancefor parent54Special Population:Children
Take precautions againstdropping infant Enter through non-ambulatoryside Precautions against hypothermia Parental accommodations Ease fears Decon parent and child Extend rule of thumb time Additional assistance for parent201455Special Population:Infants
Consider type of disability andassociated equipment Wheelchair, walker, etc., istreated as personal property Casts (temporary or fixed) willrequire removal for decon Considerations for deaf and orblind populationSpecial Population:Disabled201456
2014 Muzzle‟s for all animals should berequirement Handler should be kept with theservice animal when possible Animal: wash for 10, rinse for 10 Consider vinyl collar or muzzle toensure all areas rinsed Leather apparatus will bedisposed of57Special Population:Service Animals
Weapons must berendered safe prior todecon Inventory & secureweapon Weapons may begovernment propertynot personal201458Special Population:Law Enforcement
Decedent handled last Move decedent through nonambulatory line Treat decedent with reverence Ensure decedent is properlycovered Secure personal effects201459Special Population:Decedent
2014 Language considerations: federalrequirement to provide translation services Cultural considerations: nationality, religion,etc.60Special Population:Other Needs
Evaluatedecontaminationefforts Re-triage Begin patienttracking Transport topatient care areas201461Duties of DRT Members inthe Hospital Post-DeconZone
2014PERSONAL PROTECTIVE EQUIPMENTSECTION IV62
201463– These could have been prevented with the use ofappropriate safety measures and personalprotective equipment Many hazardous agents are odorless, colorlessand tasteless; you may be exposed before youknow it! Recent studies have shown that only a smallnumber of health care workers have hadadverse effects following exposure tocontaminated patientsHow are you at risk?
201464 Unfortunately, no one type of PPE will protectagainst all hazardous agents! Appropriate PPE is determined by thecharacteristics and amount of the hazardousagent present. PPE must be used correctly in order to reduceexposure. When the agent is unknown – use the highestlevel of PPE available prior to starting any deconprocedure.Personal ProtectiveEquipment (PPE)
––––––Face shieldMaskGownGlovesBootiesBonnet2014 Hazardous agents may require, at a minimum,specific types of Standard Precautions toprevent exposure Examples include:StandardPrecautions65
201466 Each level provides for a certain amount ofskin and respiratory protection againstbiological and chemical agents– Level A PPE– Level B PPE– Level C PPE– Level D PPE Four levels:Hazardous Agent PPE
2014 Weakness: bulky, heavy, and increasedpotential for heat stress and slip, trip or fallinjuries, requires a great deal of education forsafety– Vapor protective suit (fully encapsulating)– Self contained breathing apparatus (SCBA)– Chemical resistant gloves and boots67 Provides the highest level of skin and respiratoryprotection:Level A PPE
2014Level A Protection68
201469 Weakness: bulky, heavy, increased potential forheat stress and slip, trip or fall injuries and maynot reduce exposure to all agents, requires agreat deal of education– Liquid splash protection suit (chemical resistant)– Self contained breathing apparatus (SCBA)– Chemical resistant gloves and boots Provides a lower level of skin protection with thehighest level of respiratory protection:Level B PPE
201470Level B Protection
201471 Weakness: bulky, heavy, increased potential forheat stress and slip, trip or fall injuries and maynot reduce exposure to all agents, cannot beused in an oxygen-deprived area.– Liquid splash protection suit with or without a hood(chemical resistant)– Air-Purifying Respirator (filters vary)– Chemical resistant gloves and boots Provides a lower level of skin and respiratoryprotection:Level C PPE
201472Level C Protection
2014 Weakness: provides no chemicalprotection and limited respiratoryprotection– Clothes (uniform, scrubs, street clothes)– Standard Precautions Provides the lowest level of skin andrespiratory protection:Level D PPE73
Your every day workclothes!201474Level D Protection
––––––Face shieldMaskGownGlovesBootiesBonnet “Trauma Team” gear:2014Radiation PPE75
– Heat Exhaustion– Heat Stroke2014Incorrect use or improper selectionPenetration into the PPE (holes/rips)Slips, trips and fallsLoss of dexterity, limited vision, impairedcommunication Heat-related illness Risks of HazardousAgent PPE76
2014– Muscle spasms– Dry skin– Fatigue– Dizziness– Dry mouth– Increased heart rate and breathing Signs and symptoms:Heat Cramps77
2014– Headache– Heavy sweating. Intense thirst– Light-headedness– Feeling faint/weakness– Pale and cool, moist skin– Increased pulse (120-200) Signs and symptoms:Heat Exhaustion78
2014– High body temperature ( 103 degrees)– Absence of sweating– Skin is hot and red– Rapid pulse; difficulty breathing; constrictedpupils– Severe symptoms of Heat Exhaustion– Advanced symptoms may include seizure,loss of consciousness or death Signs and symptoms:Heat Stroke79
2014 If you recognize any of these signs andsymptoms in yourself or another teammember, NOTIFY the DRT Leader Immediately remove the DRT memberfrom their post Doff the DRT member Perform decontamination procedures Treat accordinglyBe careful 80
Blood PressurePulseRespirationsTemperatureWeightRecent medical history for diarrhea, vomiting, etc 201481 Orally hydrate during this time Team leader needs to be aware of environmental factorsthat may limit time in suits. Maximum time in suits is 45minutes (including self-decon)–––––– DRT members must receive a pre- and post-deconmedical screen:Medical Screen Pre- andPost-Decon
2014 Chemical resistant booties or rubber boots Chemical-resistant and nitrile gloves– 3-M Breath Easy Powered Air Purifying Respirators (PAPRs)– Scott O-Vista Full Face Mask Air Purifying Respirators (APRs)– Cooling Vest optional Tychem suits with duct tape to sealWhat are we going tobe using?82
2014 Requires fit-testing and appropriate filterfor useAPRs83
2014 Does not require fit-testing Requires batteries and appropriate filtersPAPRs84
2014 Equipment must be properly maintainedand checked before and after each use– No fit testing needed for PAPR Medical surveillance of DRT member Staff must be fit tested for APRRespiratory ProtectionProgram85
2014– Inner Gloves– Tychem Suit– PVC Boot Covers or chemicalresistant rubber boots– Outer Gloves– Duct Tape around glove and bootopenings and suit zipper– Respirator – if using APR, duct tapeseal– Write identifier and don time on ducttape on back of suitWork with a Buddy! Put on:DonningPPE86
2014 It‟s important to be able to communicatewith the other members of the DeconResponse Team while wearing PPE Some facilities have communicationequipment that fits under PPE. If you donot have access to that equipment or itfails Communicating whileusing PPE87
201488“I need help with thispatient”
201489“I‟m having troublebreathing”
2014“I‟m OK”90
Decon ResponseTeam must nowdecon themselves intheir PPE and thenthe equipment Once in the PostDecontaminationZone, DRT memberscan doff PPE201491The last patient hasbeen decontaminated now what?
2014Duct tape at suit and glove sealsOuter glovesRespiratorPeel suit away frombody– PVC boot covers– Inner gloves–––– Work with a Buddy! For speed, cut with scissors and peel off or Take off:Doffing PPE92
––––2014Remove them from their postRemove their PPE suit and clothesPerform assisted deconTreatIf one of the team becomes a patient:What do you do if one ofthe DRT Members goesdown?93
2014Questions andAnswers94
2014– Directed Decon– Ambulatory Patient Decon– Non-Ambulatory Patient Decon Patient Decontamination– Connecting the Water Supply– Connecting the Electrical Supply– Setting up the Shower System Setup of Decon Equipment– Use of APRs– Use of PAPRs Donning and Doffing PPEPractice Activities95
2014Medical Surveillance Questionnaire96
2014Class Evaluation97
201498We hope that you found this informative andfun!Thank you for your time and your interest inbeing a member of your facility‟s DeconResponse Team.
3
Regional Decontamination Response Team (DRT) CurriculumUpdated: 02-2008#1.Slide TitleHospital DecontaminationTeamsSlide TextWelcome to the Regional Decontamination Response TeamCourse sponsored by the EMS-Hospital Disaster Group orEHDG. This curriculum was developed by the health careproviders within Trauma Service Area-P as a way to providespecific training on healthcare facility decontaminationresponse. This training course is based on the HazMat forHealthcare curriculum and was developed on a regional levelto ensure a consistent and coordinated response to anyincident that results in contaminated patients, as well as, toreduce facility-training costs.2.Presented By Introduction of InstructorsNamePlace of Employment/DepartmentBackgroundRelated Training3.Welcome & IntroductionsIntroduction of Class ParticipantsNamePlace of Employment/DepartmentBackgroundRelated TrainingExplain the Class LogisticsClass length and break timesCell phone/pager useLocation of restrooms and phonesLocation of vending machinesFood/drink restrictions (if any)Lunch arrangementsQuestions regarding class set-up / agenda4.Section I:Introduction:5.Course ObjectivesDevelop an understanding of hazardous substances in anemergencyDevelop an understanding of the role of the First ReceiverDevelop an understanding of the selection on use of PersonalProtective Equipment (PPE)Develop an understanding of detection devices anddecontamination equipmentDevelop an understanding of basic decontaminationprocedures6.Why are we Here?Since 9/11, hospitals have become increasingly aware of theirvulnerability to manmade and natural incidents. Our focustoday will be on contaminate related events, whether from anPage 1
Regional Decontamination Response Team (DRT) CurriculumUpdated: 02-2008#Slide TitleSlide Textaccidental internal or external event. Persons exposed tohazardous materials may present to hospitals for treatmentand possible decontamination.Prior to their treatment for medically related issues,contaminated patients must be decontaminated so as not toplace the facility or its personnel at risk for becomingcontaminated with biological, chemical, or radiological agents.A healthcare facility‟s number one priority is to protect theiremployees, their environment, and their property.You are being trained to become a member of your healthcarefacility‟s Decontamination Response Team. This team willmost likely be activated AFTER emergency managementpersonnel know an incident has occurred.As part of a healthcare facility‟s Decon Response Team, youare tasked with ensuring the safety of personnel and thefacility. This is accomplished by performing complete andthorough decontamination of contaminated or exposedpatients.7.If a contaminated person isallowed inside our facility What if a contaminated patient were able to enter a facility fortreatment prior to decontamination, what are the possibleconsequences for that facility?Facilitate discussion among participants. Answers mayinclude:Close the department/hospitalDamaged public imageContamination of staff, patientsCost of facility decontaminationEmployee health effectsLoss of workLoss of revenue8.Employee exposures & hospitalexposure is what we want toavoid!As you‟ve heard, the potential consequences of acontaminated person entering your facility for treatment canhave severe and lasting effects.9.Exposure vs. ContaminationPatients that have been exposed to biological, chemical, orradiological agents may be contaminated so, what‟s thedifference between exposed and contaminated?Exposure is when a person has been in the area of an agentand there is a potential for absorption or surfacecontamination.Contamination means there is an agent on the person thatMUST be removed or washed away to prevent additionalharm.Anyone that is in the area of exposure to a hazardous agentPage 2
Regional Decontamination Response Team (DRT) CurriculumUpdated: 02-2008#Slide TitleSlide Textshould be decontaminated because it may not be possible tosee the agent on the person. Err on the side of caution.10.How does a person becomeexposed?People can be exposed to biological, chemical, andradiological toxins through internal and external accidentalspills, as well as through terrorist attacks. Any one of theseagents will adversely affect a hospital if a contaminated personis allowed inside prior to decon.Exposure routes include:Inhalation – breathing in air with hazardous particlesIngestion – eating or drinking food with particles on themAbsorption – through the skin, especially if clothes are allowedto remain onInjection – through needles and other invasive devices*Based on exposure, precautions, decontamination, andtreatment options may vary.11.How does a person becomecontaminated?Contamination can occur any day through average means.One could be exposed from the chemicals under their kitchensink, working in the fields, or driving down the highway.12.What is decontamination?It is the process of reducing and preventing the spread ofcontamination by having a person wash their body –
8. Define Directed Self Decon 9. Explain the process of Directed Self Decon 10. Demonstrate the procedure for Directed Self Decon 11. Define Decontamination Response Team 12. Differentiate between the need for directed self decon and decontamination response team initiation 13. Define the roles and responsibilities of members of a Decontamination
electric charge to the decon solution. The charged decon droplets will envelop and adhere to the target. The result is the ability to perform a more effective decon, for a wide range of incidents, with significantly less decon set up. DeconIQ will include interactive lecture supported by videos,
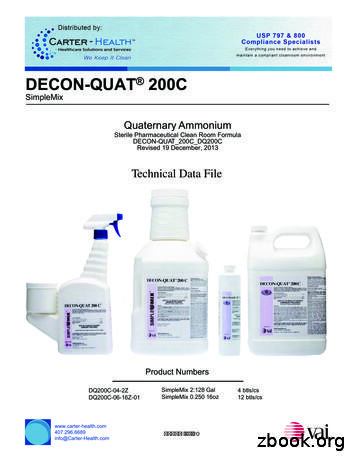
DECON-QUAT 200C DECON-QUAT 200C PRODUCT DESCRIPTION DECON-QUAT 200C is a fifth generation quaternary ammonium solution for use in in pharmaceutical, biotechnology, medical device manufacturing facilities, healthcare facilities, and hospitals. This product is a One Step Disinfectant, Non-Food Contact Sanitizer,
decon supplies could be the most cost effective preparation for on-scene decon, but requires transporting victims to hospitals for secondary decon. Thirteen counties lack any fire service or hospital decon equipment. Seven counties are located in northwest Minnesota, three in the southeast corner, and three in east central Minnesota.
Blood Typing Lab pages 23-29 binder pages 4-6 Fingerprinting Lab pages 30-31 binder page 7 Blood Spatter Lab pages 32-43 binder pages 8-13 Shoe Impressions pages 44- 45 binder page 14 Pathology pages 46-48 binder pages 15-18 ****DNA pages 49-50 binder pages *****must be done last
This study presents the further refinement of the original Decon Green "Classic" to the New Decon Green formula. Four main Four main problems were identified with the "Classic": 1) limited capacity for non-traditional agents; 2) long-term stability; 3) homogeneity;
DECON-PHENE II Technical Data File Page 7 of 16 Veltek Associates, Inc. 15 Lee Boulevard, Malvern, PA 19355-1234 T: 610-644-8335 F: 610-644-8336 www.sterile.com Rev: 07Apr2022 ML Rev: D-19 DECON-PHENE II High pH Phenolic Sanitizer Formulated for Effective Aseptic Controlled Environment ("Clean Room") Sanitation .
DECON-SPORE 200 Plus is available as a 2.3% sporicidal dilution ratio (3 oz/gallon) in a 16 oz trigger spray and 1 gallon container. Both 16 oz and 1 gallon containers are sterile and come in our one-step, ready-to-use, SimpleMix System. Each sterile container of DECON-SPORE 200 Plus is individually double bagged sterile in easy tear packaging.
(An Alex Rider adventure) Summary: After a chance encounter with assassin Yassen Gregorovich in the South of France, teenage spy Alex Rider investigates international pop star and philanthropist Damian Cray, whose new video game venture hides sinister motives involving Air Force One, nuclear missiles, and the international drug trade. [1. Spies—Fiction. 2. Adventure and adventurers—Fiction .