September 25, 2014 Inside Job - Citizen
September 25, 2014www.citizen.orgInside JobHow an Influential Group of Doctors Exerts Influence OverMedicare Payments to Physicians
AcknowledgmentsThis report was written by Adam Crowther, Researcher for Public Citizen’s Congress Watchdivision, and edited by Congress Watch Research Director Taylor Lincoln and CongressWatch Director Lisa Gilbert.About Public CitizenPublic Citizen is a national non-profit organization with more than 300,000 members andsupporters. We represent consumer interests through lobbying, litigation, administrativeadvocacy, research, and public education on a broad range of issues including consumerrights in the marketplace, product safety, financial regulation, worker safety, safe andaffordable health care, campaign finance reform and government ethics, fair trade, climatechange, and corporate and government accountability.Public Citizen’s Congress Watch215 Pennsylvania Ave. S.EWashington, D.C. 20003P: 202-546-4996F: 202-547-7392http://www.citizen.org 2014 Public Citizen.
ContentsBackground on Medicare’s Relative Value-Based Payment System. 7Components of a Medicare Part B Physician Payment . 9Criticisms of the RUC. 12RUC Proceedings and Results are not Readily Available to the Public . 12The Self-Regulation Authority Granted to the RUC Fails to Ensure Unbiased Recommendations . 13Time Values Submitted by Physicians to the RUC Often Are Vastly Inflated . 13The RUC Process for Evaluating New, Revised, and Potentially Misvalued Codes ProducesHighly Skewed Results. 14Results of Five Year Reviews (1995 to 2010) . 16Results of Annual Reviews of Misvalued Codes (2012-2014). 17The RUC’s Membership Imbalance Contributes to the Shortage of Primary Care Physicians . 18Health Care Experts Criticize RUC Process . 21Policy Solutions . 23
Public CitizenInside JobAnd that was the point where I knew the system had been co-opted It hadbecome a political process, not a scientific process. And if you don’t think it’spolitical, you only have to look at the motivation of why AMA wants this job.”--Harvard School of Public Health Professor William Hsaio, commenting on thegovernment’s decision to give the American Medical Association authority overthe committee that recommends values used in setting Medicare payments.The key data point in the formula that is used to set Medicare payment rates islargely determined by a secretive committee that is managed and funded by theAmerican Medical Association (“AMA”), the overarching trade association ofphysicians. 1 This committee is the AMA’s Relative Value Scale Update Committee(commonly referred to as the “RUC”), whose recommendations to the Centers forMedicare and Medicaid Services (“CMS”) are a major factor in determining physicianpayments for each procedure covered by Medicare Part B. This component ofMedicare, also known as supplemental insurance, was responsible for 255.1 billionout of 575 billion in payments by the entire Medicare program in 2013. 2 About 75percent of Medicare Part B funding comes from taxpayers. 3The RUC has been accused of overstating many of the factors used to determine aphysician payment. In one example, the Washington Post reported that a physicianwas able to bill the government for procedures that would have required him towork an average of 26 hours a day for a year, based on the RUC-influenced data usedby CMS. 4 When the RUC has recommended adjusting the values that determinephysician payments, it has been more than five times as likely to increase pay for aprocedure as decrease it. Although the RUC is not an official federal advisorycommittee, CMS has historically accepted its recommendations approximately 90percent of the time, although the rate has decreased somewhat in recent years. 51 Peter Whoriskey and Dan Keating, How a Secretive Panel Uses Data that Distorts Doctors’ Pay,WASHINGTON POST (July 20, 2013), http://wapo.st/1rS6qi7.2 Part B covers many services not covered by Medicare Part A, or hospital insurance. See also TheFacts on Medicare Spending and Financing, KAISER FAMILY FOUNDATION (viewed September 11, 2014),http://bit.ly/1pchvq4.3 The Facts on Medicare Spending and Financing, KAISER FAMILY FOUNDATION (viewed September 11,2014), http://bit.ly/1pchvq4.4 Peter Whoriskey and Dan Keating, How a Secretive Panel Uses Data that Distorts Doctors’ Pay,WASHINGTON POST (July 20, 2013), http://wapo.st/1rS6qi7.5 Miriam J. Laugesen, Roy Wada, and Eric M. Chen, In Setting Doctors’ Medicare Fees, CMS AlmostAlways Accepts the Relative Value Update Panel’s Advice on Work Values, 31 HEALTH AFFAIRS 965, 965972 (2012).September 25, 20144
Public CitizenInside JobIn theory, the total amount spent paid by CMS to physicians participating inMedicare Part B is a fixed pie. In general, if adjusting the underlying framework thatdetermines physician payments is expected to cause an increase or decrease of 20million in Medicare expenditures, CMS must make adjustments to offset thatincrease. 6The RUC’s influence over physician payments extends well beyond Medicarepayments because private insurers also use the Medicare payment framework as abaseline for determining their payments. 7 Private insurance companies often settheir payments based on the underlying Medicare fee schedule. 8 Because privatesector costs are not limited by an overarching cap, the RUC’s upward pressure onper-procedure pay is likely increasing the nation’s overall health care bill.Specialists are overrepresented on the RUC at the expense of primary carephysicians. To the extent that the RUC’s members are biased towards their ownspecialties, this results in the overvaluing of specialty procedures at the expense ofprimary care. Because there are significantly more specialty procedures thanprimary care procedures, the overvaluation of specialty and procedural services hascaused U.S. specialists’ pay to rise much more rapidly than primary care physicianssince the formation of the RUC. 9Higher pay to specialists creates greater incentives for medical students to practicespecialty or procedural medicine, resulting in a shortage of primary care physicians.Wait times to see primary care physicians already are much longer than forspecialists, and the percentage of primary care physicians accepting new patients islower than for specialists. The shortage of primary care physicians is likely to growworse in the coming years. 106 42 C.F.R. 405, 410, 411, et al, Medicare Program; Revisions to Payment Policies Under the PhysicianFee Schedule, Clinical Laboratory Fee Schedule & Other Revisions to Part B for CY 2014; Final Rule,(December 2013).7 Brian Klepper, The RUC, Health Care Finance’s Star Chamber, Remains Untouchable, HEALTH AFFAIRSBLOG (February 1, 2013), http://bit.ly/1Beb7YG.8 Elisabeth Rosenthal, Patients Costs Skyrocket; Specialists’ Income Soar, NEW YORK TIMES (January 18,2014), http://nyti.ms/1BU4ydg.9 Press Release, McDermott Bill: “Family Doctor for Every Family Act,” Office of Rep. Jim McDermott(D-Wash.) (March 30, 2011), http://bit.ly/1tRW3hp.10 Press Release, MMS Study Shows Patient Wait Times for Primary Care Still Long, MassachusettsMedical Society (July 15, 2013), http://bit.ly/1o7cowo. See also Health Resources and ServicesAdministration Bureau of Health, PROJECTING THE SUPPLY AND DEMAND FOR PRIMARY CARE PRACTITIONERSTHROUGH 2020 2 (2013), http://1.usa.gov/1oVpTi4.September 25, 20145
Public CitizenInside JobFurther, because the RUC is not an official federal advisory committee, it is exemptfrom federal transparency requirements. Even the codes that serves as thefoundation for Medicare Part B payments is owned by the AMA and hidden frompublic view. Very little information about the procedures associated with the codesis publicly available. This leaves the public in the dark about a process thatdetermines how a significant percentage of their tax dollars are being allocated.Several former CMS administrators and a prominent public health expert who wasinfluential in developing the current Medicare Part B physician payment systemhave criticized this arrangement for its self-dealing nature.The RUC is a “political process, not a scientific process. And if you don’t think it’spolitical, you only have to look at the motivation of why AMA wants this job,” saidWilliam Hsaio, a professor at the Harvard University School of Public Health whosework formed the foundation of the current Medicare Part B physician paymentsystem. 11 That committee’s work was performed in an unbiased fashion in whichmedical specialties were prohibited from wielding influence. The frameworkdeveloped by Hsaio and other researchers at Harvard was funded by the federalgovernment, which explicitly prohibited medical societies from participating due topotential conflicts of interest. In the end, however, the AMA still gained control overthe process.Because of its influential role in setting health care prices, the function performed bythe RUC should be performed by CMS. The work of the CMS or another committee ofunbiased experts should be accompanied by greatly enhanced transparency andother safeguards against self-interested decision-making.Criticisms of the RUC Absence of Transparency: Despite its public function, the RUC is exempt from regulations that governgovernment committees. The RUC’s proceedings are conducted behind closed doors and its results andprocesses are largely hidden from the public.Self-Regulating: The RUC is an industry managed, industry funded committee whose recommendations arelargely decisive in determining Medicare payments to physicians. Historically, its recommendations areaccepted about 90 percent of the time, though the rate has declined slightly in recent years.Membership imbalance: The RUC’s composition is overwhelmingly stacked in favor of specialists and againstprimary care givers.Effects:- The RUC’s recommendations contribute to higher Medicare payments to specialists.- The RUC’s recommendations likely lead to higher costs for privately funded health care services.- The RUC’s upward pressure on payments to specialists contributes to the shortage of primary care physicians.11 Haley Sweetland Edwards, Special Deal: The Shadowy Cartel of Doctors that Controls Medicare,WASHINGTON MONTHLY (July/August 2013), http://bit.ly/1vbX1Xr.September 25, 20146
Public CitizenInside JobI. Background on Medicare’s Relative Value-BasedPayment SystemIn 1992, the Health Care Financing Administration (“HCFA”) (which became theCenters for Medicare and Medicaid Services in 2001) overhauled its system forpaying physicians who treat patients enrolled in Medicare Part B. Prior to 1992,Medicare Part B payments were determined largely through a system in whichproviders were paid a set amount for each patient they discharged. 12 However,beginning in the 1980s, the HCFA began to explore other payment systems,eventually arriving at a system that would pay physicians per procedure rather thanper patient treated.As part of the transition, the HCFA funded a study examining the feasibility ofimplementing what is now known as a resource-based relative value system. 13 Thestudy was conducted by Harvard School of Public Health researchers, who workedwith the AMA to randomly distribute surveys to members of 33 medical specialtysocieties. 14 These physicians were unaware that their responses would form thefoundation for a new system for physician payments under Medicare Part B. Themethodology used to develop the new payment system was transparent andsubjected to high levels of academic peer review. 15 The HCFA barred medicalspecialty societies from administering the study due to potential conflicts ofinterest. 16In 1991, during the transition to the new system, the HCFA received a letter fromthe AMA in which the organization offered to assume responsibility for maintainingand updating the newly established physician payment system at no cost to thegovernment. The HCFA granted this request, giving the AMA and the newly formedRUC authority over a process from which it was explicitly excluded just a few yearsbefore. 17 Some have suggested that the AMA was granted control over this processbecause President George H.W. Bush was wary of giving a government agency direct12 NATIONAL BIPARTISAN COMMISSION ON THE FUTURE OF MEDICARE, MEDICARE FROM THE START TO TODAY(June 1998), http://1.usa.gov/1oc9SVC.13 PETER BRAUN AND NANCY MCCALL, RTI INTERNATIONAL, METHODOLOGICAL CONCERNS WITH THE MEDICARERBRVS PAYMENT SYSTEM AND RECOMMENDATIONS FOR ADDITIONAL STUDY: A REPORT BY STAFF FROM RTIINTERNATIONAL FOR THE MEDICARE PAYMENT ADVISORY COMMISSION 2 (December 2011),http://1.usa.gov/1uEZXab,14 Id.15 Id.16 Id.17 Id.September 25, 20147
Public CitizenInside Jobcontrol over health care pricing. 18 The AMA spends approximately 7 million eachyear maintaining the RUC. 1918 Haley Sweetland Edwards, Special Deal: The Shadowy Cartel of Doctors that Controls Medicare,WASHINGTON MONTHLY (July/August 2013), http://bit.ly/1vbX1Xr.19 Peter Whoriskey and Dan Keating, How a Secretive Panel Uses Data that Distorts Doctors’ Pay,WASHINGTON POST (July 20, 2013), http://wapo.st/1rS6qi7.September 25, 20148
Public CitizenInside JobII. Components of a Medicare Part B Physician PaymentThe system developed by the Harvard researchers was implemented in 1992. Itcreated three inputs to value each medical service provided by Medicare: physicianwork, practice expenses, and malpractice expenses (described below). Each servicewas valued relative to all other services. The rationale was that prices for medicalcare in a well-functioning market should be based on the value of the resourcesneeded to provide that care. 20Work RVUs, which are currently the most heavily weighted of the threecomponents, are designed to capture the relative time and intensity of effortassociated with a given procedure. In measuring work RVUs, the RUC considers “thetime it takes to perform the service; the technical skill and physical effort; therequired mental effort and judgment; and stress due to the potential risk to thepatient” as the primary factors that influence work RVU valuation. 21Practice expense RVUs are designed to measure the costs associated withmaintaining a medical practice. 22 There are two inputs that determine the value of apractice expense RVU: direct practice expenses and indirect practice expenses.Direct practice expenses concern those for clinical labor, medical supplies, andmedical equipment. Indirect practice expenses concern administrative labor, officeexpenses, and all other expenses. 23 Practice expense RVUs are derived from datacollected through an AMA-sponsored survey and through practice-based reportingof expenses. 24Malpractice expense relative value units are based on malpractice insurancepremium data collected from commercial and physician-owned insurers. 25 Thesevalues are generated by CMS without input from the AMA. 2620 PETER BRAUN AND NANCY MCCALL, RTI INTERNATIONAL, METHODOLOGICAL CONCERNS WITH THE MEDICARERBRVS PAYMENT SYSTEM AND RECOMMENDATIONS FOR ADDITIONAL STUDY: A REPORT BY STAFF FROM RTIINTERNATIONAL FOR THE MEDICARE PAYMENT ADVISORY COMMISSION 2 (December 2011),http://1.usa.gov/1uEZXab,21 Overview of the RBRVS, AMERICAN MEDICAL ASSOCIATION (viewed July 29, 2014),http://bit.ly/1zrE3L8.22 42 C.F.R. 405, 410, 411, et al, Medicare Program; Revisions to Payment Policies Under thePhysician Fee Schedule, Clinical Laboratory Fee Schedule & Other Revisions to Part B for CY 2014;Final Rule, (December 2013).23 Id.24 Id.25 Id.September 25, 20149
Public CitizenInside JobTable 1: Components of a Relative Value Unit, the Foundation for a Physician Paymentunder Medicare Part B, Calendar Year 2014ComponentDescriptionWork RVUTime; technical skill; physicaleffort; mental effort; stress due topatient riskClinical labor; medical supplies;medical equipment;administrative labor; officeexpenses; other expenses.Costs related to malpracticeinsurance premiumsPractice Expense RVUMalpractice RVUPercentage ofTotal RVU50.9 percent44.8 percent4.3 percentSource: RVS Update Process, American Medical Association 1 (2014).To determine the total physician payment, the values of these three components areadjusted for geography (called the “geographic cost price index”), added togetherand multiplied by a CMS-determined conversion factor, to determine the paymentrate for a given procedure. [See Figures 1 and 2 below.]Figure 1: Formula for Determining Physician Payment per ProcedurePhysician Payment [(Work Relative Value Unit * Geographic Adjustment) (Practice Expense RelativeValue Unit * Geographic Adjustment) (Malpractice Expense Relative Value Unit * GeographicAdjustment)] * CMS-Determined Conversion FactorFor example, code 64755, which refers to an incision of stomach nerves, has work,practice expense, and malpractice RVU values of 15.05, 7.98, and 3.07, respectively.If the procedure were performed in the Washington, D.C., area, the geographicadjustments for work, practice expense, and malpractice expense, would be 1.05,1.202, and 1.205, respectively. For calendar year 2014, the conversation factor is 35.8228. 27Washington, D.C., physicians would be paid 1,042 for administering this procedure,as shown in Figure 2:26 AMA Specialty Society Relative Value Scale Update Committee, AMERICAN ACADEMY OF ORTHOPEDICSURGEONS (viewed July 31, 2014), http://bit.ly/1k9eGtO.27 The Medicare Physician Payment Schedule, AMERICAN MEDICAL ASSOCIATION (viewed July 28, 2014),http://bit.ly/1rYoaYU.September 25, 201410
Public CitizenInside JobFigure 2: Steps for Determining Physician Payment for Code 64755 (Incision of StomachNerves)Determine Geographically Adjusted Relative Value Unitsfor Work, Practice and MalpracticeRelativeComponent ValueUnitGeographicallyAdjustedRelative ValueUnitsGeographicAdjustmentAdd Adjusted Relative Value Units andMultiply by Conversion FactorGeographicallyAdjustedRelative ValueUnitsWork15.05x1.05 15.802515.8025Practice7.98x1.202 9.591969.59196Malpractice3.07x1.205 3.699353.69935 29.09381ConversionFactorx 35.8228Payment 1,042.22The RUC is primarily responsible for recommending work RVUs for new, revised, orpotentially misvalued codes. These codes, known as Current ProceduralTerminology codes (“CPTs”) are owned by the AMA. Medicare uses a coding asystem based on the AMA codes, but does not release detailed information about thecodes themselves. 2828 Overview of the RBRVS, AMERICAN MEDICAL ASSOCIATION (viewed July 29, 2014),http://bit.ly/1zrE3L8. See also Press Release, Centers for Medicare and Medicaid Services, New CMSCoding Changes Will Help Beneficiaries (October 6, 2004), http://go.cms.gov/1l7f8Uu.September 25, 201411
Public CitizenInside Job“The idea that 100 billion in federal spending is based on fixed prices thatgo through an industry trade association in a process that is not open to thepublic is pretty wild.”--Former CMS Administrator Thomas ScullyIII. Criticisms of the RUCCriticisms of the RUC can be divided into three categories: its lack of transparency,biased recommendations stemming from its self-regulatory status, and allegationsthat its role in inflating costs for specialized procedures has contributed to theshortage of primary care physicians.RUC Proceedings and Results Are Not Readily Available to the PublicThe process through which medical services are valued by the RUC is challenging tounderstand, in part because of its complexity but also because of a lack oftransparency on behalf of the AMA. The RUC has enormous power in setting healthcare prices, but most of its proceedings occur behind closed doors and withoutpublic scrutiny. Minutes from each of the RUC’s three annual meetings are not madepublicly available. Additionally, when the RUC votes each spring to assign work RVUvalues to CPT codes, the voting results are not released to the public. In what was arelatively recent change, the RUC started disclosing the vote totals, but they are onlyaccessible to those who have an AMA account and only a year after the votes occur.This and most of the AMA’s documentation about the RUC and its proceedingsrequire an account, which can be acquired on the AMA’s website by anybodypossessing an e-mail address.One critical piece of information that is not disclosed to anybody (including RUCmembers) is any indication of how each member of the RUC voted. (A list of the votetotals from the RUC’s 2013 meeting can be found in the Appendix.) Because of itsunofficial status, the RUC is exempt from rules governing official federal advisorycommittees. 29In 2011, a group of Georgia primary care physicians brought a lawsuit against theU.S. Department of Health and Human Services over its relationship with the AMAand the RUC process. In Fischer v. Berwick, the plaintiffs argued that because of therate at which CMS accepted the RUC’s recommendations, the RUC should beregulated under the Federal Advisory Committee Act (“FACA”). The FACA imposes29 Federal Advisory Committee Act, 5 U.S.C. §1-10 (2012).September 25, 201412
Public CitizenInside Joborganizational and procedural requirements on committees that provide advice tothe federal government, including requirements that the committees remainunbiased, open their meetings to the public, and provide records of their meetingsand reports. The law applies to advisory committees “established or utilized” byfederal agencies. 30 The plaintiffs argued that the RUC was operating as a de factoadvisory committee to the federal government, and therefore its proceedings shouldbe subject to greater levels of transparency and accountability. The case wasdismissed on jurisdictional grounds.The Self-Regulation Authority Granted to the RUC Fails to Ensure UnbiasedRecommendationsAfter the RUC votes, it sends its recommendations to CMS. CMS is not required toaccept the RUC’s recommendations. In fact, the RUC is insistent that its role in theprocess is only to exercise its right to petition the government. 31 However, studieshave demonstrated that CMS accepts RUC recommendations at overwhelminglyhigh rates. A 2012 article in Health Affairs reported that between 1994 and 2010,CMS accepted the RUC-recommended work RVU values nearly 90 percent of thetime. 32The degree to which CMS accepts the RUC-recommended values has contributed tothe belief that the RUC has become a self-regulating industry group. Two additionalbut related drivers of this criticism are how the RUC collects its data and the resultsof the RUC’s reviews of new, revised, and potentially misvalued codes.Time Values Submitted by Physicians to the RUC Often Are Vastly InflatedThe RUC’s process for collecting the physician time data that drives work RVUvaluations is controversial. The time value assigned to a given procedure is derivedfrom estimates provided to the RUC from surveys that are administered by medicalspecialty societies. Physicians are aware that their survey responses will have directimplications for their payment under Medicare.One unnamed specialist group’s survey, reported upon by the Wall Street Journal,included language advising that returning the survey was “important to you andother physicians because these values determine the rate at which Medicare and30 Id.31 The RVS Update Committee, AMERICAN MEDICAL ASSOCIATION (viewed July 28, 2014),http://bit.ly/1nRbdiQ.32 Miriam J. Laugesen, Roy Wada, and Eric M. Chen, In Setting Doctors’ Medicare Fees, CMS AlmostAlways Accepts the Relative Value Update Panel’s Advice on Work Values, 31 HEALTH AFFAIRS 965, 965972 (2012).September 25, 201413
Public CitizenInside Jobother payers reimburse for procedures.” 33 This stands in stark contrast to how thefirst round of data collection that was conducted by the Harvard researchers. Thosesurveys were distributed to a random sample of physicians who had identifiedthemselves as members of a specialty but were not necessarily members of therelevant specialty society or the AMA. 34Several analyses of Medicare data have revealed that time values submitted byphysicians are often inflated. A 2013 story in the Washington Post revealed that timeestimates for colonoscopies were sometimes inflated by as much as 100 percent. 35In one example, the Washington Post reported on a physician who was able to billthe government for procedures that would have required him to work an average of26 hours a day for a year, based on the RUC-influenced values used by CMS. Thedoctor, in reality, worked only nine to 10 hours per day. 36A review by the Wall Street Journal revealed that the time value used for carpaltunnel surgery was overestimated by between 28 and 32 percent. 37 A 2006 study byRTI International, a think tank, used surgery logs to compare RUC-reported times toactual time needed to perform the procedure. The researchers discovered that theRUC-reported times were longer by as little as 30 minutes and as much as twohours. 38The RUC Process for Evaluating New, Revised, and Potentially Misvalued Codes ProducesHighly Skewed ResultsWhether due to its evaluations of how much time it takes to complete a procedureor other less quantifiable factors that make up the work component of the relativevalue formula, results of the RUCs recommendations in reviewing codes suggest thatit is not a fair arbiter.33 Anna Wilde Mathews and Tom McGinty, Physician Panel Prescribes the Fees Paid by Medicare, WALLSTREET JOURNAL (October 26, 2010), http://on.wsj.com/1mV1nIj.34 PETER BRAUN AND NANCY MCCALL, RTI INTERNATIONAL, METHODOLOGICAL CONCERNS WITH THE MEDICARERBRVS PAYMENT SYSTEM AND RECOMMENDATIONS FOR ADDITIONAL STUDY: A REPORT BY STAFF FROM RTIINTERNATIONAL FOR THE MEDICARE PAYMENT ADVISORY COMMISSION 4 (December 2011),http://1.usa.gov/1uEZXab,35 Peter Whoriskey and Dan Keating, How a Secretive Panel Uses Data that Distorts Doctors’ Pay,WASHINGTON POST (July 20, 2013), http://wapo.st/1rS6qi7.36 Id.37 Anna Wilde Mathews and Tom McGinty, Physician Panel Prescribes the Fees Paid by Medicare, WallStreet Journal (October 26, 2010), http://on.wsj.com/1mV1nIj.38 NANCY MCCALL, JERRY CROMWELL AND PETER BRAUN, RTI INTERNATIONAL, VALIDATION OF PHYSICIAN SURVEYESTIMATES OF SURGICAL TIME USING OPERATING ROOM LOGS (2006), http://bit.ly/XhicbK.September 25, 201414
Public CitizenInside JobThe RUC, at the request of CMS, has evaluated the work RVU values of new, revised,or potentially misvalued codes. New codes are reviewed and assigned work RVUvalues when the AMA’s CPT Editorial Panel has determined that a medical service isdifferent enough from an existing service to warrant an entirely new code. Revisedcodes are those in which the CPT Editorial Panel has determined that the medicalservice that corresponds to an existing code has been slightly modified, whichprompts a reevaluation of the work RVU. Finally, potentially misvalued codes arethose that CMS or the RUC have determined could have values that are no longerconsistent with medical practices.New and revised codes have been reviewed annually since 1992. Potentiallymisvalued codes were reviewed in five year intervals between 1995 and 2010, andhave been reviewed annually in more recent years.In order to identify potentially misvalued codes, CMS uses a variety of screens andfilters, as well as through comments submitted to proposed rule makings. Section3134 of the Patient Protection and Affordable Care Act outlines several (but not all)of the criteria available to CMS to determine which codes are potentially misvalued.They are: Codes (and families of codes as appropriate) for which there has been thefastest growth in use;Codes (and families of codes as appropriate) that have experiencedsubstantial changes in practice expenses;Codes for new technologies or services within an appropriate period (suchas three years) after the relative values are initially established for suchcodes;Multiple codes that are frequently billed in conjunction with furnishing asingle service;Codes with low relative values, particularly those that are often billedmultiple times for a single treatment;Codes that have not been subject to review since the implementation ofthe RBRVS;And such other codes determined to be appropriate by the Secretary. 39Interestingly, Section 3134 also exempts the new criteria from the provisions of theFederal Advisory Committee Act. In 2014, Congress passed the Protecting Access toMedicare Act, which provides additional guidance for determining which codes can39 The Patient Protection and Affordable Care Act, H.R. 3950, 111th Congress, Section 3134.September 25, 201415
Public CitizenInside Jobbe selected for review. Given advances in medical technology and increasedfamiliarity with existing procedures, a reasonable assumption would be that whenpotentially misvalued codes are reviewed, the result would be a decrease in workRVU values. However, this has not been the case, either with the annual reviewprocess or the five year review process.Results of Five Year Reviews (1995 to 2010)Congress passed legislation in 1990 that required CMS to review the
Public Citizen Inside Job September 25, 2014 5 In theory, the total amount spent paid by CMS to physicians participating in Medicare Part B is a fixed pieIn general. , if adjusting the underlying framework that determines physician pay
1. What is job cost? 2. Job setup Job master Job accounts 3. Cost code structures 4. Job budgets 5. Job commitments 6. Job status inquiry Roll-up capabilities Inquiry columns Display options Job cost agenda 8.Job cost reports 9.Job maintenance Field progress entry 10.Profit recognition Journal entries 11.Job closing 12.Job .
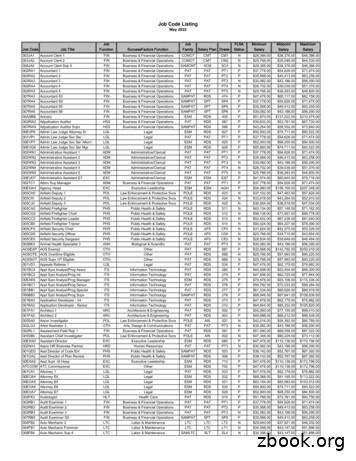
Job Code Listing May 2022 Job Code Job Title Job Function SuccessFactors Function Job Family Salary Plan Grade FLSA Status Minimum Salary Midpoint Salary Maximum Salary. Job Code Listing May 2022 Job Code Job Title Job Function SuccessFactors Function Job Family Salary Plan Grade FLSA Status Minimum Salary Midpoint Salary
delete job tickets. Click the add new job ticket button to add a new job. Existing job tickets can be cloned into new jobs by using the clone job button. Click the edit button to edit the Job's key information found in the Specs window, such as the client contact, job name/title, project, job type, start date, or profit center. Click the delete
September: 2013 33,391.18 9/24/2013 October: 2013 33,391.18 10/24/2013 December: 2013 65,031.50 12/20/2013 January: 2014 33,099.37 1/23/2014 February: 2014 33,099.37 2/24/2014 March: 2014 33,099.37 3/24/2014 April: 2014 31,662.23 4/25/2014 May: 2014 31,662.23 5/22/2014 June: 2014 31,662.24 6/26/2014 392,881.03
September 2014—September 2015 Fall Semester 2014 Monday, September 1 Labor Day. College is closed Tuesday, September 2 Community Day - Full-time faculty returns to campus Wednesday, September 3 New student orientation Sunday, September 7 Last day to WITHDRAW with no financial penalty Monday, September 8 Fall semester begins, ESL Class Start
3. "Floral Design Workshops" 4. 2006 Master Gardener Trainee Class Roundup 5. "Back to Your Roots," the Southeastern Regional Master Gardener Conference Happy September 1 September 14 September 15 September 17 September 19 September 20 September 24 September 26 September
Outcome of Ergonomics Overall, Ergonomic Interventions: Makes the job Makes the job safer by preventing injury and illnessby preventing injury and illness Makes the job Makes the job easier by adjusting the job to the by adjusting the job to the worker Makes the job Makes the job more pleasantmore p
1. 2 Chr. 15-16, John 12: 27-50 2. 2 Chr. 17-18, John 13: 1-20. J U L Y ,1"0 1. Job 20-21, A ct s 10: 24-48 2. Job 22-24, A ct s 11 3. Job 25-27, A ct s 12 4. Job 28-29, A ct s 13: 1-25 5. Job 30-31, A ct s 13: 26-52 6. Job 32-33, A ct s 14 7. Job 34-35, A ct s 15: 1-21 8. Job 36-37, A ct s 15: 22-41 .