Asymptomatic Carriage And Transmission Of SARS-CoV-2: What .
Can J Anesth/J Can Anesth (2020) 1729-xREVIEW ARTICLE/BRIEF REVIEWAsymptomatic carriage and transmission of SARS-CoV-2: Whatdo we know?Patients asymptomatiques du SARS-CoV-2 et transmission duvirus : Où en sont nos connaissances?. Paula Meyler, MD, FRCPC . Michelle Mozel, MSc .Susan Lee, MAS, MD, FRCPCTonia Tauh, MD, FRCPC . Richard Merchant, MD, FRCPCReceived: 29 April 2020 / Revised: 21 May 2020 / Accepted: 25 May 2020 / Published online: 2 June 2020Ó Canadian Anesthesiologists’ Society 2020AbstractPurpose Risktohealthcareworkerstreatingasymptomatic patients infected with severe acuterespiratory syndrome coronavirus 2 (SARS-CoV-2) in theoperating room depends on multiple factors. This reviewexamines the evidence for asymptomatic or presymptomatic carriage of SARS-CoV-2, the risk oftransmission from asymptomatic patients, and the specificrisks associated with aerosol-generating procedures.Protective measures, such as minimization of aerosolsand use of personal protective equipment in the setting oftreating asymptomatic patients, are also reviewed.Source We examined the published literature as well asSocietal guidelines.Principal findings There is evidence that a proportion ofthose infected with SARS-CoV-2 have detectable viralloads prior to exhibiting symptoms, or without everdeveloping symptoms. The degree of risk of transmissionfrom asymptomatic patients to healthcare providers willdepend on the prevalence of disease in the population,which is difficult to assess without widespread populationscreening. Aerosol-generating procedures increase theodds of viral transmission from infected symptomaticpatients to healthcare providers, but transmission fromS. Lee, MAS, MD, FRCPC (&) P. Meyler, MD, FRCPC M. Mozel, MSc T. Tauh, MD, FRCPC R. Merchant, MD,FRCPCDepartment of Anesthesia and Perioperative Medicine, RoyalColumbian Hospital, 330 E Columbia, New Westminster, BCV3L 3W7, Canadae-mail: suze.lee@utoronto.caDepartment of Anesthesiology, Pharmacology, andTherapeutics, UBC Faculty of Medicine, Vancouver, BC,Canada123asymptomatic patients has not been reported. Techniquesto minimize aerosolization and appropriate personalprotective equipment may help reduce the risk tohealthcare workers in the operating room. Some societalguidelines recommend the use of airborne precautionsduring aerosol-generating procedures on asymptomaticpatients during the coronavirus disease pandemic,although evidence supporting this practice is limited.Conclusion Viral transmission from patients exhibiting nosymptoms in the operating room is plausible and efforts toreduce risk to healthcare providers include reducingaerosolization and wearing appropriate personalprotective equipment, the feasibility of which will varybased on geographic risk and equipment availability.RésuméObjectif Le risque encouru par les travailleurs de la sante traitant des patients asymptomatiques infecte s par lesyndrome respiratoire aigu se ve re du coronavirus 2(SARS-CoV-2) en salle d’ope ration de pend de plusieursfacteurs. Ce compte rendu examine les donne es probantesconcernant la pre sence asymptomatique ou pre symptomatique du SARS-CoV-2, le risque de transmissiondes patients asymptomatiques, et les risques spe cifiquesassocie s aux interventions ge ne rant des ae rosols. Nouspassons e galement en revue diffe rentes mesures deprotection, telles que la minimisation des ae rosols etl’utilisation d’e quipements de protection individuelle, dansun contexte de traitement de patients asymptomatiques.Source Nous avons examine la litte rature publie e ainsique les directives socie tales.Constatations principales Selon certaines donne esprobantes, une proportion des personnes infecte es par leSARS-CoV-2posse dentdeschargesviralesde tectables avant la pre sence de symptômes, voire meˆme
Risk of asymptomatic transmission of COVID191425Figure 1 Examples ofcontrolling exposure to COVID19 in the operating room usingthe Centers for Disease Controland Prevention Hierarchy ofControls model31 to implementfeasible and effective controlstrategies to protect healthcareworkers from occupational risk.Control methods at the top arepotentially more effective andprotective.sans manifestation de symptômes. Le degre de risque detransmission des patients asymptomatiques aux travailleursde la sante de pendra de la pre valence de la maladie dansla population, une donne e difficile à e valuer sans de pistagege ne ralise . Les interventions ge ne rant des ae rosolsaugmentent le risque de transmission virale des patientssymptomatiques infecte s aux travailleurs de la sante , maisla transmission de patients asymptomatiques n’a pas e te rapporte e. Les techniques visant à minimiserl’ae rosolisation et les e quipements de protectionindividuelle adapte s pourraient eˆtre utiles pour re duire lerisque des travailleurs de la sante en salled’ope ration. Certaines directives re gionales et nationalesrecommandent le recours à des pre cautions contre latransmission par voie ae rienne durant les interventionsge ne rant des ae rosols pratique es sur des patientsasymptomatiques pendant la pande mie de coronavirus,bien que les donne es probantes appuyant cette pratiquesoient limite es.Conclusion La transmission virale des patientsasymptomatiques en salle d’ope ration est plausible et lesefforts visant à re duire le risque pour les travailleurs de lasante comprennent la re duction de l’ae rosolisation et leport d’e quipements de protection individuelle adapte s,deux mesures dont la faisabilite variera en fonction durisque ge ographique et de la disponibilite des e quipements.Keywords SARS-CoV-2 asymptomatic carrier COVID19 transmissionevidence on the risk of asymptomatic spread of severeacute respiratory syndrome coronavirus 2 (SARS-CoV-2)to HCWs, particularly in locations such as the operatingroom where aerosol-generating procedures (AGPs) areroutinely performed.Historical contextSevere acute respiratory syndrome coronavirus 2 is not thefirst pathogenic coronavirus to jump from its animal host tohumans. Of the seven known human coronaviruses, fourcause mild symptoms similar to the common cold and threeothers can cause severe illness in humans.2 Severe acuterespiratory syndrome (caused by SARS-CoV), Middle Eastrespiratory syndrome (caused by MERS CoV) andCOVID-19 (caused by SARS-CoV-2) all result fromhighly transmissible viruses whose natural reservoir is inbats. Several factors are associated with pathogen spilloverfrom animal hosts to humans and establishment ofsustained spread in humans, such as changes in humanbehaviour, new technologies and industry, changes in landuse, increased international travel, microbial adaptation,inadequate public health measures, and sharing ourenvironment with domestic or wild animals.3,4 Given thatthese factors are unlikely to change, we can expect to seemore outbreaks of emerging infectious diseases in thefuture.5SARS-CoV-2 mechanism and timing of infectionThere have been over 5,600,000 confirmed cases ofcoronavirus disease (COVID-19) and 355,000 deathsworldwide to date (27 May 2020).1 There is concern thatviral transmission may occur from patients exhibiting nosymptoms, which might pose a risk to healthcare workers(HCWs). In this review, we summarize the availableRespiratory viruses, like SARS-Cov-2, are known to spreadby direct contact, such as touching an infected person or asurface infected with virus-containing droplets expelled byan infected person.6 Current recommendations to preventthe spread of SARS-CoV-2, such as frequent hand washingand keeping at least a 2-m distance, would be effective123
1426with droplet-borne transmission. Recommendations topractice good hand hygiene, physical distancing, andisolation of infected patients to prevent transmission arecommon across respiratory viruses and organizationalguidelines. There has been controversy, even before theemergence of SARS-CoV-2, over whether respiratoryviruses, including coronaviruses (e.g., MERS), caneffectively spread via the airborne route and whethercontact and droplet precautions are sufficient to preventtransmission.7 The World Health Organization (WHO)recommends droplet and contact precautions for avianinfluenza and MERS, while the Centers for Disease Controland Prevention takes a more conservative approach,recommending airborne precuations.7 The WHO doesrecommend additional airborne precautions for novelacute respiratory viruses until transmission patterns canbe observed. There is some evidence that SARS-CoV-2 canspread via aerosols, with virus particles found at distances[ 2 m from the source for up to three hours.8-10 Theinfectivity of these viral particles, however, remains to bedetermined.The median incubation period for SARS-CoV-2 hasbeen estimated to be 5.1 days, with 97.5% of patientsdeveloping symptoms within 11.5 days, which is similar toSARS-CoV.11 The upper end of this incubation periodforms the rationale for public health recommendations toself-isolate for 14-days after exposure. Several studies haveshown that viral loads are highest shortly after symptomonset, gradually decreasing over the ensuing 21 days.12-14Longer periods of viral shedding (up to 30 days) have alsobeen reported.15Evidence of asymptomatic/pre-symptomatic carriersThe prevalence of asymptomatic (never developssymptoms) or pre-symptomatic (tests positive prior tosymptom development) illness has been documented inseveral populations. Among 565 Japanese nationalsevacuated from Wuhan, China and tested for SARS-CoV2 by real time reverse transcriptase polymerase chainreaction (RT-PCR), 13 tested positive with four (30.8%;95% confidence interval [CI], 7.7 to 53.8) asymptomatic atthe time of testing.16 Of the 3,063 passengers on board thequarantined Diamond Princess Cruise ship who were testedfor SARS-CoV-2, 17.9% of those who tested positive wereasymptomatic (95% CI, 15.5 to 20.2).17 Residents of along-term skilled nursing facility with an early outbreak ofCOVID-19 were all screened for symptoms of illness andviral RNA. Of the 76/82 (93%) residents tested, 23 testedpositive of which 13 (57%) were categorized asasymptomatic at the time of testing.18 Seven days later,ten out 13 previously asymptomatic residents developed123S. Lee et al.symptoms and were reclassified as pre-symptomatic duringtesting. Twenty-four asymptomatic patients in Nanjing,China were characterized after testing positive throughscreening of close contacts. During hospitalized follow-up,five (20.8%) developed symptoms, 17 (70.8%) showedabnormal computed tomography (CT) scans, and seven(29.2%) had normal CT scans and did not developsymptoms.19 Both targeted testing for SARS-CoV-2 inhigh-risk Icelandic residents and general Icelandicpopulation screening for SARS-CoV-2 showedasymptomatic patients that tested positive for SARSCoV-2. In the 1,924 targeted-testing group, 7% had nosymptoms, while in the population screening group, 43% of10,797 Icelandic residents testing positive for the virusreported having no symptoms at the time of testing.20The available evidence across a range of populationsindicates that asymptomatic and pre-symptomatic patientscan test positive for SARS-CoV-2 at rates ranging from17.9% to 57% of those who test positive showing nosymptoms. Nevertheless, the overall prevalence ofasymptomatic carriers will depend on the distribution andhow widespread the disease is in a given population. Forexample, in the Icelandic population, where less than 1% ofthe population was positive for SARS-CoV-2 (and 43% ofthem reporting no symptoms) at the time of screening, thepoint prevalence of asymptomatic cases was 0.34%.20 Incontrast, in a highly infected environment like theDiamond Princess cruise ship where 20% of passengerseventually tested positive, 10% of all passengers and crewwere asymptomatic at the time of testing.17In a study of SARS-CoV-2 upper respiratory viral loadsin 18 patients, one asymptomatic patient was includedbecause of close contact with an infected patient. The viralload that was detected in the asymptomatic patient wassimilar to that in the symptomatic patients, which suggeststhe transmission potential of asymptomatic or minimallysymptomatic patients.21Cases of asymptomatic transmissionWhile symptomatic disease is frequently associated withinfectivity, there is speculation that for SARS-CoV-2, thelatent period (time from exposure to onset ofinfectiousness) may be shorter than the incubation period(time from exposure to onset of symptoms), leaving awindow of time when the patient is infectious but not yetexhibiting symptoms. This is supported by a study of viralloads in Chinese patients, which indicated that presymptomatic viral transmission likely occurred.13 Usingdata from infector-infectee pairs, the authors estimated thatviral transmission may have occurred two to three daysprior to symptom onset in up to 44% of patients, indicating
Risk of asymptomatic transmission of COVID19a transmission pattern more similar to seasonal influenzathan SARS-CoV. Of the 157 locally acquired infectionsidentified in Singapore, ten secondary cases (6.4%) werelikely acquired prior to the development of symptoms inthe index cases. Infections happened on average one tothree days before symptom onset in the index cases.22 Afamilial cluster was identified in Anyang, China where oneasymptomatic carrier never developed symptoms but testedpositive for the virus, and likely infected five familymembers.23 In a point-prevalence survey of a skillednursing facility in King County, Washington, 27 out of 48(56%) with positive tests were asymptomatic at the time oftesting. Given an estimated doubling time of 3.4 days (95%CI, 2.5 to 5.3) in that facility, viral shedding fromasymptomatic or pre-symptomatic residents likelycontributed to early transmission to other residents andstaff members.24Infection of HCWsHealthcare workers are at increased risk for infectionthrough occupational exposure to pathogens such asbacteria, fungi, viruses, and parasites.25 Healthcareproviders have been affected by SARS-CoV-2, with highreported rates of infection26 and death27 in the UK,although it is unclear how much nosocomial transmissionoccurred since frontline staff tested positive at similar ratesto non-clinical staff and deaths were not reported in ICUHCWs, possibly indicating that current infection controlpractices in the UK have been effective in limitingoccupationally acquired HCW infection. Nevertheless,HCWs have been found to be at higher risk for infectionwith respiratory pathogens in other settings, particularlythose who perform AGPs.28,29 A systematic review showedthat, compared with healthcare workers who did notperform aerosol-generating procedures, those whoperformed tracheal intubation had an increased risk ofcontracting SARS-CoV in the 2003 epidemic (odds ratio,6.6) than those who performed non-invasive ventilation(odds ratio, 3.1), tracheotomy (odds ratio, 4.2), and manualventilation before intubation (odds ratio, 2.8).29Nevertheless, the authors note very low quality in allincluded studies, study designs subject to recall bias, andfew clear reports of personal protective equipment (PPE)compliance. Low numbers of exposed HCWs also limit thegeneralizability of the study—in the meta-analysis for riskof HCW infection after tracheal intubation, two of the fourincluded studies had five or fewer HCWs in the exposedgroup. A separate study found that the protectionguidelines failed to thoroughly prevent the transmissionof SARS-CoV to HCWs in 2003 and that 9% of theinterviewed healthcare workers who had intubated patients1427contracted SARS. Nevertheless, the cause-effectrelationship between infection and intubation in thesehealthcare workers who contracted SARS was unknown.30Techniques to minimize risk to HCWs in the operatingroomSince asymptomatic transmission is possible with SARSCoV-2, and HCWs are at risk of infection, techniques tominimize risk in the operating room are needed. Currenttests for SARS-CoV-2 are not sensitive enough to eliminatethe possibility of asymptomatic carriers entering theoperating room. Therefore, other strategies, such as riskreduction through the hierarchy of controls model31 can beemployed (see Figure 1). Strategies include delayingelective surgery in patients at high risk for infection,substituting regional anesthesia for AGPs whenappropriate, reducing aerosolization, clearing aerosols,and providing appropriate PPE for HCWs.Preoperative testingThe American Society of Anesthesiologists (ASA) andAnesthesia Patient Safety Foundation jointly recommendpreoperative testing of all elective surgery patients wherethere is SARS-CoV-2 in the region.32 Patients testingpositive should be delayed for non-urgent surgery. Theycaution, however, that the low sensitivity of viral PCR testsmeans that up to 30% of patients may falsely test negative.Therefore, regardless of a negative test, additional riskreduction strategies are indicated, including airborne PPEwhen an AGP is planned.Reducing aerosolizationAerosol-generating procedures, such as intubation andmask ventilation, are thought to create small airborneparticles that can be suspended in air and travel longdistances.33 Under the assumption that asymptomatic andpre-symptomatic patients carrying SARS-CoV-2 have theability to generate aerosolized virus particles capable oftransmission to HCWs during AGPs, there may be ways toreduce the risk of aerosolization. These techniques includeavoiding mask ventilation if possible, reducing oxygenflows, having a good seal with the face mask through use ofa thenar eminence (‘‘VE’’) grip, and ensuring profoundparalysis prior to airway instrumentation.34 Aerosolizationrisk from coughing during extubation can be minimizedwith lidocaine, dexmedetomidine, remifentanil, andfentanyl.35123
1428Innovative barrier techniques, such as plastic cubeboxes, screens, and tents, to reduce aerosolization duringairway management of patients with COVID-19 have beendescribed, but further research is required to prove efficacyor recommend routine use for asymptomatic patients,particularly if they hinder timely airway management, ashas recently been shown in a simulation study.36-38S. Lee et al.The ASA recommends the use of airborne PPE for allairway-related AGPs because asymptomatic patients maybe harbouring SARS-CoV-2.48 In contrast, the UnitedKingdom Association of Anaesthetists does not specificallyrecommend N95 masks for asymptomatic patients,although they acknowledge that as population diseaseburden increases, it might become necessary to treat allpatients as high-risk because of the threat of asymptomaticviral transmission.49,50Operating room ventilation and clearance of aerosolsSevere acute respiratory syndrome and MERSinvestigations found airborne disease transmissionthrough inefficient hospital ward ventilation systems.39Fortunately, most operating rooms, owing to their design inprotection of the surgical site, have air exchange rates thatadequately minimize deposition and floating time ofrespiratory virus particles (at least 9 per hour).40Operating room workers should know their local airexchange rates to determine when aerosolized particlesare likely to have been cleared, thus reducing the risk ofviral transmission to new members of the operating roomteam entering the room after an AGP has beenperformed.41Recommended PPEWhile PPE is important, it is only one of the protectivemeasures used to protect HCWs managing airways.42 Earlyin an epidemic, before viral transmission routes have beenwell characterized, PPE recommendations for HCWs canbe chaotic and evolving.43 During the 2003 SARSepidemic, most virus transmission to HCWs occurredbefore PPE was routine, or was associated with PPEbreaches. Once the epidemic subsided, the dangers ofexcessive PPE recommendations (e.g., increasedcontamination during doffing) were recognized, as wellas several instances where droplet precautions wereeffective in prevent
port d’e quipements de protection individuelle adapte s, deux mesures dont la faisabilite variera en fonction du risque ge ographique et de la disponibilite des e quipements. Keywords SARS-CoV-2 asymptomatic 5carrier COVID19 transmission There have been over 5,600,000 confirmed cases of coronavirus disease (COVID-19) and 355,000 deaths
Jan 01, 1994 · screening of asymptomatic persons for CAS using physical exam or carotid ultrasound.3 This recommendation was based on new evidence at the time, including the Asymptomatic Carotid Artery Study (ACAS), a RCT involving 1662 subjects with asymptomatic stenosis greater than 60%. Results of ACAS suggested that the overall benefit of treatment with .
The present guidelines are applicable to COVID-19 patients who have been clinically assessed and assigned as mild /asymptomatic cases of COVID-19. 2. Asymptomatic cases; mild cases of COVID-19 The asymptomatic cases are laboratory confirmed cases who are not experiencing any symptoms and have oxygen saturation at room air of more than 93%.
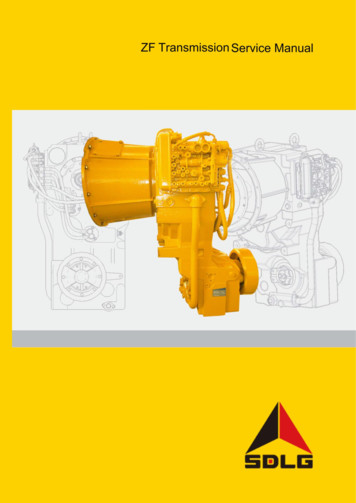
ZF Transmission Service Manual 5 2 Transmission System 2.1 Transmission Introduction 2.1.1 General Overview of the Transmission The ZF power gearshift transmission is composed of the hydraulic torque converter and rear-mounted countershaft transmission with multi-sheet friction clutch. The SDLG 938L、
Conditions of Carriage and the terms and conditions of other Carriers, and in any case where we have a legal liability to you in relation to your flight. 2.1.2 These Conditions of Carriage also apply to free of charge travel, staff travel concession tickets and reduced
dynamic response of railway and carriage under the high speed moving loads. Dynamic response of the rail and carriage due to action of multi-roller carriage was determined by means of the finite element method. Wu, and Thompson [10] have investigated vibration analysis of railway track with multiple wheels on the rail.
Carriage House, shown in Georgian Brick CARRIAGE . CertainTeed starter and CertainTeed hip and ridge required. See actual warranty for specific details and limitations. 6 51955.indd 6 1/23/18 2:22PM. ol ar
drill press position. 5. Unlock the carriage and headstock. Move the headstock to the middle of the way tubes. Then move the carriage between the head-stock and base mount (right side). 6. Tighten the headstock and carriage lo
“Am I My Brother’s Keeper?” Cain & Abel by Tintoretto. Everything can be taken from a man but the last of the human freedoms - to choose one’s attitude in an given set of circumstances, to choose one’s own way.--Auschwitz Survivor, Victor E. Frankl Human Gene Map. OnegShabbat Archives –Emanuel Ringleblum Remembrance: To record and to teach future Generations. The time has come to .