Factsheet 44 NHS Services - Compassehub
Factsheet 44NHS servicesSeptember 2019About this factsheetThis factsheet contains information about NHS ‘primary care’ services –services you approach in a non-emergency situation when you first havea health problem.It looks at services to help you identify: if you need to see a GP services provided by a GP and services you access via your GP services from your local pharmacy how the NHS helps you manage a long term condition that can betreated and managed but not cured NHS screening programmes and services for older adults.Age UK produces other factsheets on NHS services – these includefactsheet 5, Dental care: NHS and private treatment; factsheet 61, Helpwith health costs and factsheet 66, Resolving problems and making acomplaint about NHS care.The information in this factsheet is applicable in England. If you are inScotland, Wales or Northern Ireland, please contact Age Scotland, AgeCymru or Age NI for their version of this factsheet. Contact details can befound at the back of this factsheet.Contact details for any organisation mentioned in this factsheet can befound in the Useful organisations section.Page 1 of 36
Contents1 National Health Service42 NHS Constitution – your rights43 Equality Act 2010 and age discrimination54 Accessible Information Standard65 Local NHS services65.1 Primary and secondary care services66 Non GP services to help if you are unwell76.1 Getting help when feeling unwell76.2 Serious or life-threatening illness or injury87 GP services97.1 Registering with a GP practice97.2 Arranging to see a GP117.3 Removing a patient from the practice list137.4 Helping to improve GP services137.5 Help with hearing difficulties147.6 Help with mental health needs147.7 Referral for a physical or mental health condition157.8 Chiropody, physiotherapy and other services167.9 Falls Prevention Services177.10 Supporting people with long-term conditions187.11 Supporting people to maintain their independence187.12 Personal health budgets198 NHS services for older people198.1 Over-60s – free prescriptions198.2 Over-60s – free NHS sight tests198.3 Over-65s – free seasonal flu jab208.4 Over-65s – free jab against pneumonia208.5 Shingles vaccination20Age UK factsheet 44NHS servicesSeptember 2019Page 2 of 36
8.6 NHS screening programmes219 Help with health costs2210 Services at your local pharmacy2310.1 Reporting unwanted side effects from medication2411 End of life care2512 Complementary therapies2713 Accessing your health records2713.1 Access to medical records of a deceased person2814 Resolving problems and making a complaint2915 Health and social care organisations30Useful organisations32Age UK35Support our work35Age UK factsheet 44NHS servicesSeptember 2019Page 3 of 36
1National Health ServiceThe fundamental principle of the NHS is that no one should be denied orcharged for necessary emergency NHS treatment.You can consult a GP and apply to register with a GP, regardless ofnationality and residential status. You must pay NHS prescriptioncharges unless you are in a group exempt from these charges. Seesection 9 for information on exemptions.Non-urgent NHS hospital care is only free if you are living here lawfullyand are ‘ordinarily resident’ in the UK. ‘Ordinarily resident’ is a legal termthat broadly means living here voluntarily, for a properly settled purposefor the time being. If you meet these requirements, access to hospitaltreatment is based on clinical need. If there are doubts about meetingordinary resident requirements, your case must be judged on its merits.If visiting the UKYou may have to pay if you need non-urgent hospital treatment.Hospitals must follow The National Health Service (Charges to OverseasVisitors) Regulations 2015 and supporting guidance.The rules vary depending on whether you live in an European EconomicArea (EEA) country or Switzerland and your healthcare is paid for by theUK via a UK-issued S1 form registered with relevant authorities; you area visitor from an EEA country with a valid European Health InsuranceCard; or are a visitor from a non-EEA. You can read about your rights atwww.nhs.uk/ by searching ‘visiting or moving to England’.2NHS Constitution – your rightsThe NHS Constitution establishes the principles and values of the NHSin England. It sets out the rights that patients, members of the publicand NHS staff are entitled to, and the responsibilities they owe eachother to ensure the NHS operates effectively and fairly.NHS organisations, the independent and voluntary sector who provideNHS services, and local authorities with a public health duty are requiredby law to take account of the Constitution when purchasing anddelivering services.An example of a patient right is: ‘You have the right to be giveninformation about test and treatment options available to you, what theyinvolve and the risks and benefits.’An example of a patient responsibility is ‘Please follow the course oftreatment you have agreed and talk to your clinician if you find it difficult.’You can order a copy of the NHS Constitution – the NHS belongs to usall (ref 2900013) from DH publications or download a copy itution-for-englandAge UK factsheet 44NHS servicesSeptember 2019Page 4 of 36
3Equality Act 2010 and age discriminationThe Equality Act 2010 protects you from being unfairly discriminatedagainst. It applies to anyone over the age of 18 and to all public services.It means it is unlawful for the NHS, without good and sufficient reason, toprovide inferior services or refuse to provide them solely because of oneof the Act’s eight ‘protected characteristics’.NoteThe Equality Act 2010 ‘protected characteristics’ are age, disability,gender reassignment, marriage and civil partnership, pregnancyand maternity, race, religion and belief, sex, and sexual orientation.Under the Act, discrimination means unfairly treating you differentlybecause of your age. The law only intends to prevent harmful orunjustifiable use of age, including a ‘stereotypical view’ of a particularage group. It does not intend to prevent differential treatment wherethere is ‘objective justification’.Cancer screening and flu vaccination programmes are examples ofwhere there may be objective justification for the NHS to offer a serviceto a certain gender or people within certain age ranges.Other situations where the Act applies to the NHS include: When a GP, consultant or other health professional discussestreatment options with you or makes a ‘best interests’ decisionabout treatment or care. Your age can play a part but staff should takeaccount of your ‘biological’ age, not simply your ‘chronological’ age (yourage in years).If there are treatments for conditions such as cancer that are lesssuccessful or less well tolerated as people get older, the doctor shoulddiscuss this openly when explaining treatment options. When providing NHS services or considering treatment options. Anexample of ‘Unjustifiable discrimination’ would be to stereotype someoneof a particular chronological age. When designing or providing a service (such as at a GP practice orout-patients clinic). An example of age discrimination would be wherestaff treat you differently on the basis of your age or take a stereotypicalview of people of a particular age.You can often clarify and resolve a situation by discussing it with staffconcerned. The law means that if necessary, you can take NHSorganisations, clinicians or managers to court on grounds of agediscrimination. You can speak to the Equality Advisory Support Servicehelpline if you think you have been discriminated against.For more information, see factsheet 79, Equality, discrimination and thePublic Sector Equality Duty.Age UK factsheet 44NHS servicesSeptember 2019Page 5 of 36
4Accessible Information StandardThe Accessible Information Standard aims to make sure that when youhave a disability or sensory loss, you receive information you can accessand understand, as well as the communication support you need, whenengaging with NHS or social care staff. This means staff must:Ask if you have communication or information needs relating to adisability or sensory loss, and if so what they are.Record your needs in your electronic and paper records.Alert/flag/highlight them, so your needs and how best to meet them are‘highly visible’ whenever staff access your records.Share details of your information and communication needs withproviders of NHS and social care services who have permission to seethem, and make sure they keep your records secure.Act by taking steps to ensure you get information you can access andunderstand and by arranging communication support.For NHS services, it is likely your GP will ask about and record yourinformation and communication needs in your GP record. When referringyou for an outpatient appointment or other NHS services, this informationshould be ‘highly visible’ to the receiving department, who transfer it toyour hospital record, making it ‘highly visible’ and act upon it.This might mean they send correspondence or information in large print,easy read, Braille or audio format or by email or arrange for a lip readeror British Sign Language Interpreter to be available for your appointment.For information contact your GP practice, Action on Hearing Loss, or TheRoyal National Institute of Blind People.55.1Local NHS servicesPrimary and secondary care servicesPrimary care services are often your first point of contact when youneed healthcare. They include services available at a GP practice orwalk-in centre, community pharmacy, and NHS services provided bydentists or high street opticians.Secondary care services are usually, but not always, hospital-based.They include out-patient clinics, planned and emergency hospitaltreatment and associated diagnostic services, for example radiology.Commissioning NHS servicesNHS England and Clinical Commissioning Groups (CCGs) areresponsible for buying (commissioning) NHS services from GPs, dentistsand hospitals. For more information about their role see section 15.Age UK factsheet 44NHS servicesSeptember 2019Page 6 of 36
66.1Non GP services to help if you are unwellGetting help when feeling unwellIt is not always necessary to contact your GP practice when you feelunwell. Other services can help you decide whether you need to see adoctor or to put your mind at rest. These include: your local pharmacist NHS 111 NHS walk-in centre minor injuries unit or urgent care centre.Local pharmacistA pharmacist can help with sore throats, colds, and other aches andpains by suggesting non-prescription medicines to ease symptoms andadvise whether you need to see a doctor. As experts on medicines, theycan answer questions about non-prescription remedies you want to buyor prescription items you take.To find out about your nearest late-opening pharmacy, call NHS 111 orvisit NHS website: www.nhs.uk/service-searchNHS 111NHS 111 is a confidential, free 24-hour telephone line operating inEngland. It provides a single point of access if you are worried about anurgent medical concern, a dental problem or seeking advice in a non-lifethreatening situation. You can access the service online by visitinghttps://111.nhs.uk/Depending on your symptoms, NHS 111 staff may tell you how to lookafter yourself at home or recommend you see a pharmacist or GP. Theymay decide to connect you to a doctor or health professional who maythen suggest 111 staff book you an appointment at your GP surgery.If the problem is more serious, they may advise you go to your nearestwalk-in centre, minor injuries unit, or Emergency department. If veryserious, staff can send an ambulance directly.Note999 is the number to call in serious, life-threatening situations.Age UK factsheet 44NHS servicesSeptember 2019Page 7 of 36
Urgent treatment centres (walk-in centre or minor injury unit)The NHS offers a mix of services able to help in urgent but not lifethreatening situations. Each offers a different level of service. By the endof 2019, they will all be called ‘urgent treatment centres’.NHS walk-in centreThese centres open seven days a week from early morning until lateevening. Often in town centres and usually run by experienced nurses,they treat minor illnesses and injuries. You do not need an appointment.Minor injuries units and urgent care centresThese are for patients with non-life-threatening injuries. Often located inhospital grounds, they treat broken bones, minor burns, head and eyeinjuries, insect and animal bites.Emergency and out of hours dental servicesCall NHS 111 to find out where to access NHS treatment in anemergency or out-of-hours. If you have a usual dentist, the practicewebsite or out-of-hours message often explains how to accessemergency care.6.2Serious or life-threatening illness or injuryIf your illness or injury is serious or life-threatening, call 999 or go to yournearest Emergency department. Life-threatening situations include: loss of consciousness persistent severe chest pain heavy blood loss that cannot be stopped medicine overdose signs indicating a stroke. These include weakness on one side of yourface making your eye or mouth droop; inability to lift both arms at thesame time; difficulties in speaking or understanding what is said.Waiting time targetsThe aim is for 95 per cent of patients attending the Emergencydepartment to be admitted, transferred or discharged within four hours ofarriving. NHS England publishes waiting time figures and they takeaccount of waits at Emergency departments and minor injury units.Hospitals are encouraged to publish their own figures.If you attend an Emergency department or spend a night on a ward, thehospital should ask you the Friends and Family Test question, describedin section 7.4.Age UK factsheet 44NHS servicesSeptember 2019Page 8 of 36
7GP servicesGP practices in England must register with the Care Quality Commission(CQC). The CQC inspects practices regularly to ensure they meet itsstandards. To find out what a practice must do to meet these standardsand about how the CQC rates practices, visit the CQC website or readthe CQC booklet ‘What can you expect from a good GP practice’.A range of services and health professionalsGP practices offer services to prevent and treat illnesses and supportpeople with long-term conditions such as diabetes, heart disease,asthma and chronic obstructive pulmonary disease (COPD).Nurse practitioners, nurse consultants and specialist nurses frequentlywork alongside GPs and practice nurses. They can diagnose, treat andmanage a variety of health conditions. Some staff, due to their additionaltraining, can prescribe from a list of medicines. See section 7.10 forinformation about supporting people with long-term conditions.7.1Registering with a GP practiceYou do not need to be ‘ordinarily resident’ in England to receive NHSprimary medical care. Anyone may register and consult with a GPwithout charge but must pay NHS prescription charges, unless in anexempt group, for example, being aged 60 and over.For details of practices in your area, visit NHS website or call NHSEngland Customer Contact Centre.You have a right to choose your GP practice and it must accept you,unless there are reasonable grounds to refuse. It is not consideredreasonable to refuse registration because you do not have a proof ofaddress or personal identification at hand. The same applies if you arean asylum seeker, refugee, a homeless patient or an overseas visitor,whether lawfully in the UK or not.If the practice is refusing to register you, it must give reasons for itsrefusal in writing. It may refuse to register you because: it has no capacity to take on new patients may not be accepting patients who live outside its practice boundary in your particular circumstances, it may not be appropriate to registerwith a practice a long way from where you live.Each practice has a boundary, enclosing certain streets or postcodes.Practices are free to register new patients who live outside theirboundary, but it is for a practice to decide if it is clinically appropriate andpractical to register you in this way. Conditions for registering a patientliving outside a practice area are explained later in this section.If you cannot find a practice to accept you, ask NHS England to allocateyou one by calling their Customer Contact Centre.Age UK factsheet 44NHS servicesSeptember 2019Page 9 of 36
Choosing a practiceIf a practice is accepting new patients, collect a practice leaflet or look ontheir website. This explains how to register and more about the staff andservices they offer, including: name and qualifications of health professionals and support staff services such as special clinics for diabetics, health promotion activitiesand whether it supports trainee GPs opening hours how to make an appointment to see or speak to staff or for a home visit how to request a repeat prescription how to contact a doctor out-of-hours information for patients with disabilities or special language needs how to comment or complain about services.Identify and ask about things important to you, for example telephoneaccess to a GP or nurse, ease of parking or support for carers.Practices have a responsibility to ensure everyone who needs to usetheir practice can do so. If you have particular difficulties getting to thepractice, due to disability or caring responsibilities, discuss them with thepractice manager so they can do their best to address or resolve them. Ifyou are a carer, ask the practice to note this in your records. This canhelp your GP understand your needs better and support you and theperson you care for.The GP contract requires every patient to have a named, accountableGP who takes responsibility for co-ordinating their care. You can expressa preference for who you would like this to be and practices should makereasonable efforts to accommodate you. This does not mean this is theGP you must see each time you visit. New patients should know thename of their accountable GP within 21 days of registration.The practice should invite you for a new patient check to discuss yourgeneral health and where necessary, offer this through a home visit.Registering with a practice if you live in a care homeYour GP may be willing to continue to care for you if you movepermanently into a local care home. Otherwise you must register with anew practice. Care homes in some areas, have a nominated GP from alocal practice who is responsible for all residents. The aim is for you tohave a GP who becomes familiar with your health needs and for the carehome to build a relationship with the GP. You have the right to request toregister with a different practice.As a care home resident, you are entitled to the same range of servicesas people living in their own home. You should not be asked to pay forGP or NHS services the GP says you need.Age UK factsheet 44NHS servicesSeptember 2019Page 10 of 36
‘Out of area’ patient registration optionGP practices are free to register patients who live outside their practiceboundary. They can agree to accept your application but without anyobligation to offer home visits. You may want to consider this option ifyou are in relatively good health and move just outside your currentpractice boundary, or would like a practice close to your place of work.Before agreeing to your request, the GP must: be satisfied it is clinically appropriate and practical in your case, and make sure you understand the consequences of this type of registration.The practice should explain what happens during normal hours whenillness means you cannot reasonably be expected to visit the surgery.Your practice must monitor the effectiveness of this arrangement and ifyour health needs change, may consider whether it would be better toregister with a practice closer to home.Practices do not have to offer out of area registration - either withouthome visits or with home visits when needed - so an application may berefused. It applies only to GP practices based in and patients living inEngland, not in cross border situations with Scotland or Wales.Registering as a temporary residentIf you are going to live away from your usual address for up to threemonths, you can apply to be a temporary resident at a local practice.They are likely to accept you unless their list is full.If you become ill while staying with friends, approach their practice to seeif they are willing to treat you. If staying in a hotel, it may have anarrangement with a local practice. Otherwise, call NHS 111 and they canrecommend the most appropriate action to take.Changing your practiceYou do not need to tell your practice if you want to change or have foundanother one to accept you. You may wish to tell them as a courtesy.Once a new practice accepts you, your old practice transfers yourmedical records. These include your unique 10-digit NHS number,which eliminates errors that could occur with name only identification.7.2Arranging to see a GPExtended hours and out-of-hours servicesPractices may offer appointments before 8am, after 6pm and atweekends. In some areas, patients registered with several localpractices would see a GP at a local hub. When calling your practiceoutside its normal hours, you are usually redirected to their out-of-hoursservice. For non-urgent care, you can call NHS 111 for advice.Age UK factsheet 44NHS servicesSeptember 2019Page 11 of 36
Making an appointmentPractices have a system for booking appointments. GPs have a duty ofcare to ensure they offer services in a manner and time that meets yourclinical needs. There is usually a system that allows you to see a GP inan emergency when there are no appointments, or speak to a GP ornurse on the telephone at an agreed time.As well as booking an appointment by telephone, you can register for thePatient Online service or download myGP App to your smartphone ortablet. These online tools let you: book appointments with a GP of your choice or cancel appointments order repeat prescriptions (see section 10) view your GP record (clinical information) link to register as an organ donor (myGP App).Ask your practice receptionist to explain about my GP App or how toregister for online access. For general information go to NHS p-online-services/Making the most of your appointmentA typical appointment slot is 10 minutes. If you have complex or multipleissues to discuss, ask for a double appointment. Make sure your GPrecord identifies your need for information in a different format or help totake part in discussions due to disability or sensory loss. Make notes to remind you what you want to tell or ask the doctor about.Do not miss things out because you think they are trivial. GPs can onlywork with what you tell them, so let them decide what is significant. If worried about new symptoms, try to remember when you first noticedthem. Does there seem to be a pattern or certain times when they arebetter or worse? Could they be linked to changes in medication? If you do not understand the answer to your questions or any wordsused, ask for an explanation or for the answer to be written down. If going for test results and to discuss treatment, your doctor should tellyou if there is more than one treatment, about the pros and cons of eachand whether there are common side effects.Seeking a second opinionIf after discussing it with your GP, you have doubts about a diagnosis ortreatment, you can ask to be referred for a second opinion. You do nothave a right to a second opinion but GPs rarely refuse, unless they donot believe it is necessary.The referral may be to another GP in your practice or a consultant. Ifyour case is complicated or diagnosis unclear, your GP or consultantmay want a second opinion to ensure they explore all possible options.Age UK factsheet 44NHS servicesSeptember 2019Page 12 of 36
Home visitsThe practice leaflet or website explains criteria for home visits. Whilehaving a general policy, staff should make decisions on a case-by-casebasis, based on clinical need. Giving a full description of your conditionwhen you phone, helps the doctor decide if you need a home visit.7.3Removing a patient from the practice listA practice can make a written request to NHS England for you to beremoved from their list. This happens if you tell them you are movingoutside the practice boundary or relocating abroad. It can happen if thepractice believes your behaviour towards staff or other patients isunacceptable or your relationship with it has irrevocably broken down.If the practice intends to request to remove you from their list, it musthave given you a written warning in the previous twelve months prior torequesting your removal. This does not apply if you were violent,threatened staff or other patients and the police were informed; or if thepractice believed issuing of a warning was not reasonable or practical.The practice should provide you with specific reasons for wanting yourremoval, unless it reasonably believes the circumstance surrounding therequest mean it is not appropriate to give a specific reason, and therehas been an irrevocable breakdown in your relationship with the practice.If it is difficult to register with a new practice, contact NHS England fordetails of your Area Team. They can allocate you to a new practice.If you disagree with the reasons for your removal and believe you havebeen treated unfairly, complain to NHS England. See section 14 forinformation about making a complaint.7.4Helping to improve GP servicesPatient Participation GroupsGP practices must have a Patient Participation Group (PPG) and makereasonable efforts to make sure it is representative of the practicepopulation. PPGs bring the patients’ perspective into the practice so thatservices, plans and activities respond to patients’ needs and priorities.Providing feedbackGP practices should offer you the opportunity, after an appointment, torespond to the Friends and Family Test question: “how likely are you torecommend the practice where you’ve been treated to your friends orfamily if they needed similar treatment?” You can also provide feedbackon NHS website and Care Opinion.For more information, and-family-test-fft/Age UK factsheet 44NHS servicesSeptember 2019Page 13 of 36
7.5Help with hearing difficultiesIf hearing difficulties affect your daily life, make an appointment to seeyour GP. If there is no medical reason, such as an ear infection or buildup of wax, your GP can refer you to a local audiology department orspecialist provider for a hearing test.Audiology staff discuss the results with you and your options, includingwhether you would benefit from a hearing aid in one or both ears. NHShearing aids are provided on long term loan and new batteries are free. Ifyou want to buy a hearing aid privately, check the hearing aid dispenseris registered with the Health and Care Professions Council.NICE produce a patient version of its guidance NG98 Hearing loss inadults: assessment and management, go icAction on Hearing Loss provides information about hearing loss andaids. Hearing Link helps people manage hearing loss.NoteAction on Hearing Loss offer a telephone hearing check if you call0844 800 3838. It is not a medical diagnosis but aims to identifyhearing loss and if necessary, prompt you to visit your GP.7.6Help with mental health needsMental health issues are as important as physical illnesses and likephysical illnesses, respond better when diagnosed and treated early.It is important to speak to your GP if you experience periods of anxiety,low mood, poor sleep, or a loss of interest in things you used to enjoy onmost days of the week, and this goes on for two weeks or more. A rangeof treatments can help, depending on the severity of your symptoms.Talking treatments, such as counselling, help you understand andmanage your feelings and behaviour. They can really help when peopleare feeling low, anxious or out of sorts. They’re proven to work andresearch shows they can work particularly well for older people.Help is available through an NHS initiative called ‘Increasing Access toPsychological Therapy’ (IAPT).Find out more by speaking to your GP or search NHS website atwww.nhs.uk/service-search Then click on the ‘P’ tab, choose‘Psychological therapies (IAPT)’ and enter your postcode to find yournearest service. In many areas you can self-refer to your local serviceand do not need a GP referral.Age UK factsheet 44NHS servicesSeptember 2019Page 14 of 36
7.7Referral for a physical or mental health conditionIf you and your GP agree you should see a consultant about a physicalcondition, you have a right to choose a consultant-led team. For a mentalhealth condition, you have a right to choose the consultant or namedhealth care professional who leads the mental health team.You can choose to have your first outpatient appointment at a hospitalwhere that consultant works and be treated by their team. The hospitalmust be in England and can be an NHS hospital, or independent hospitaloffering suitable treatment that provides this service to the NHS.The consultant will not necessarily be present for this or futureappointments but retains overall clinical responsibility for your care.This choice is available in most circumstances but not if you need urgentor emergency care, for example if you have chest pains or cancer issuspected, or you are detained under the Mental Health Act 1983.If you are not offered a choice, despite further discussion with your GP,contact your local CCG to find out what choice should be available toyou. Search for your CCG on the NHS website.Choosing your hospital – practical and quality issuesYou can discuss your preferences and options with your GP, comparehospitals on the NHS website or read hospital inspection reportspublished on the CQC website. As we
NHS services September 2019 About this factsheet This factsheet contains information about NHS ‘primary care’ services – services you approach in a non-emergency situation when you first have a health problem. It looks at services to help you identify: if you need to see a GP services provided by
bunchberry dr nhs wms amb . burgundy ln nhs wms twl . burkwood dr nhs wms amb . burning tree st chs wms twl . burnock dr chs wms mbe . burr ridge rd nhs nms twl . burrwood ave nhs nms ang . burrwood st nhs nms ang . burt dr chs cms lce
of NHS Direct, and led the team preparing New Labour's first White Paper, The New NHS: Modern, dependable, which laid the foundations and structure for the current NHS reform programme. He was a member of the top management board of the NHS for 12 years, between 1988 and 2000. His earlier career included 23 years in NHS management,
NHS Long Term Plan Implementation Framework I 3 Introduction to the NHS Long Term Plan Implementation Framework 1.1 The NHS Long Term Plan, published in January 2019, set out a 10-year practical programme of phased improvements to NHS services and outcomes, including a
assessment tool called NHS Seeing ambulance services in a different light More than a patient transport service Key points NHS ambulance services face some of the most demanding performance targets in the world. Ambulance services answer approximately 7.5 million calls per year, 6 million of which receive an emergency response.
allowances are known as NHS Bursaries’1 and apply to courses qualifying students for certain professions (see Professions with training funded by NHS Bursaries). Students wishing to undertake these courses apply for an NHS bursary instead of Student Finance. NHS Bursaries are award
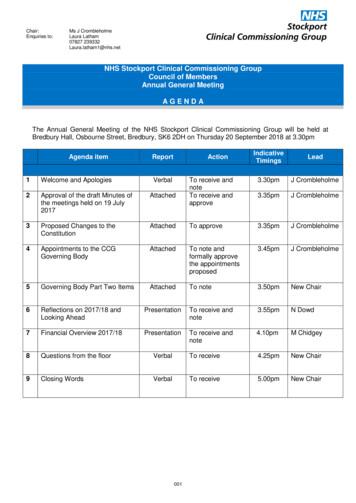
Dr Ranjit Gill . Chief Clinical Officer . NHS Stockport CCG . John Greenough . Lay Member . NHS Stockport CCG . Louise Hayes . Head of Communications and Engagement NHS Stockport CCG . Diane Jones . Director of Service Reform . NHS Stockport CCG . Dr Deborah Kendall .
Patient rights and NHS promises. 13. Part 4 - The things patients should do to help. 27. Part 5 - Rights and promises the NHS makes for NHS staff. 29. Part 6 - The things staff should do to help. 33. Part 7 - Telling the NHS
us88280731 astm d 4255/d 4255m 2015 us88281030 awwa c 706 1980 us88281031 awwa c 706 1972 us88281034 awwa c 707 1975 us88281036 awwa c 708 1996 us88281041 awwa c 710 2002 us88281044 awwa c 712 2002 us88281059 awwa c 901 1988 us88281060 awwa c 901 1978 us88281092 awwa d 103 1980 us88281099 awwa d 110 2004 us88281110 ansi/awwa d 130 1987 us88281120 ansi/awwa f 102 1991 us88281124 awwa c 104/a21 .