Alberta Pregnancy Pathways - Alberta Health Services
Alberta Pregnancy PathwaysAdopted from Perinatal Services BC, 2015.While every attempt has been made to ensure that the information contained herein is clinically accurate and current, AHS acknowledges that many issues remaincontroversial, and, therefore, may be subject to practice interpretation.Developed by the Maternal Newborn Child & Youth Strategic Clinical Network – Version 4.2 September 2020
Revision ControlVersionRevision DateV-1.0V-2.0V-2.1V-2.2September 2016April 2017September 2017March 2018V-3.0September 2018V-3.1October 2018V-4.0January 2019V-4.1March 2019V-4.2September 2020Summary of RevisionsOriginal DocumentRefer to Summary of Revisions – separate documentRevisions based on provincial chart audit and staff evaluationRevisions to pathway formsClarification around sedation score and assessment criteriafor intrapsinal and intrathecal blocks and epidurals.Addition to initial newborn assessment completion guide –assessment of newborn palette to include palpation andvisualization.Clarification of assessment for motor block.Addition of safe swaddling to comfort or soothe and link toHealthy Families, Healthy Children video.Addition of supplementation volumes for breast fed infants.Pg 86 Supplementation volumes to refer to term babies only(not late preterm).Pg 90 Formula volume (for baby not breastfeeding) returnedto previous 30ml/kg/24 hours – follow hunger cues.Pg 108 Newborn stools 48-72 hours: 3 or more transitionalstools/day; 72 hours – 4-6 weeks: 3 or more stools/dayPg 104 Lab bilirubin or transcutaneous bilirubin measured onall infants within 24 hours of birth and prior to discharge.Updated Appendix 1 and 2 – Strategies for TeachingObstetrics to Rural and Urban Caregivers (STORC).Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020AuthorMNCY SCN Postpartum Newborn Working GroupUrsula Szulczewski, Manager, MNCY SCN Debbie Leitch, Executive Director, MNCY SCNTMDebbie Leitch, Executive Director, MNCY SCNTMDebbie Leitch, Executive Director, MNCY SCNTMDebbie Leitch, Executive Director, MNCY SCNTMDebbie Leitch, Executive Director, MNCY SCNTMDebbie Leitch, Executive Director, MNCY SCNTMJolene Willoughby, Coordinator, Education andConsultation, APHPPage 2 of 157
TABLE OF CONTENTSINTRODUCTION TO ALBERTA POSTPARTUM AND NEWBORN CLINICAL PATHWAYS6ACKNOWLEDGEMENTS7POSTPARTUM CLINICAL PATHWAY8INTRODUCTIONPHYSIOLOGICAL HEALTH: VITAL SIGNSPHYSIOLOGICAL HEALTH: PAINPHYSIOLOGICAL HEALTH: LOCHIAPHYSIOLOGICAL HEALTH: PERINEUMPHYSIOLOGICAL HEALTH: ABDOMINAL INCISIONPHYSIOLOGICAL HEALTH: RH FACTORPHYSIOLOGICAL HEALTH: BREASTSPHYSIOLOGICAL HEALTH: BREASTS (NON-BREASTFEEDING WOMEN)PHYSIOLOGICAL HEALTH: ELIMINATION (BOWEL FUNCTION)PHYSIOLOGICAL HEALTH: ELIMINATION (URINARY FUNCTION)PHYSIOLOGICAL HEALTH: EPIDURAL/SPINAL SITEPHYSIOLOGICAL HEALTH: SENSORY/MOTOR BLOCKADE (POST NEURAXIAL ANESTHESIA/ANALGESIA ONLY)PHYSIOLOGICAL HEALTH: HEALTHY EATINGPHYSIOLOGICAL HEALTH: ACTIVITIES/RESTINFANT FEEDING: BREASTFEEDINGINFANT FEEDING: BREAST MILK SUBSTITUTE, FORMULA ONLYPSYCHOSOCIAL HEALTH: BONDING AND ATTACHMENTPSYCHOSOCIAL HEALTH: EMOTIONAL STATUS AND MENTAL HEALTHPSYCHOSOCIAL HEALTH: SUPPORT SYSTEMS/RESOURCESLIFESTYLE: FAMILY FUNCTIONLIFESTYLE: FAMILY PLANNING/SEXUALITYLIFESTYLE: HEALTH FOLLOW-UP IN COMMUNITYLIFESTYLE: SUBSTANCE USECOMMUNICABLE DISEASES: HEPATITIS BCOMMUNICABLE DISEASES: HEPATITIS CCOMMUNICABLE DISEASES: HERPES SIMPLEXCOMMUNICABLE DISEASES: HIVCOMMUNICABLE DISEASES: RUBELLACOMMUNICABLE DISEASES: VARICELLA ZOSTERCOMMUNICABLE DISEASES: INFLUENZA AND ILIKEY REFERENCESRESOURCES FOR BOTH HEALTH CARE PROFESSIONALS AND FAMILIESRESOURCES FOR HEALTH CARE PROFESSIONALSRESOURCES FOR PARENTSAPPENDIX 1: ABBREVIATION DEFINITIONSDeveloped by the Maternal Newborn Child & Youth SCN Version 4.2 – September 7505254555657585960616263Page 3 of 157
APPENDIX 2A: STORC E-LEARNING MODULES – AHSAPPENDIX 2B: STORC E-LEARNING MODULES – COVENANT HEALTH6466POSTPARTUM CLINICAL PATH67POSTPARTUM CLINICAL PATH:69A GUIDE TO COMPLETION69POSTPARTUM CLINICAL DOCUMENTATION1.0 BIRTH SUMMARY2.0 CLINICAL OBSERVATION3.0 MATERNAL ASSESSMENT70717274NEWBORN CLINICAL PATHWAY76NEWBORN CLINICAL PATHWAY77ABOUT THE NEWBORN NURSING CARE PATHWAY:CLINICAL OBSERVATIONSINFANT FEEDING: BREASTFEEDINGSCREENING/OTHER: NEWBORN METABOLIC SCREENINGSCREENING/OTHER: VITAMIN KPHYSIOLOGICAL HEALTH: HEADPHYSIOLOGICAL HEALTH: NARESPHYSIOLOGICAL HEALTH: EYESPHYSIOLOGICAL HEALTH: EARSPHYSIOLOGICAL HEALTH: MOUTHPHYSIOLOGICAL HEALTH: CHESTPHYSIOLOGICAL HEALTH: ABDOMEN/UMBILICUSPHYSIOLOGICAL HEALTH: SKELETAL/EXTREMITIESPHYSIOLOGICAL HEALTH: SKINPHYSIOLOGICAL HEALTH: NEUROMUSCULARPHYSIOLOGICAL HEALTH: GENITALIAPHYSIOLOGICAL HEALTH: ELIMINATION – URINEPHYSIOLOGICAL HEALTH: ELIMINATION – STOOLBEHAVIOURAL ASSESSMENTHEALTH FOLLOW-UP: SAFETYHEALTH FOLLOW-UP: NEWBORN CAREREFERENCES FOR HEALTH CARE PROFESSIONALS AND PARENTSRESOURCES FOR HEALTH CARE PROFESSIONALSRESOURCES FOR PARENTSAPPENDIX 1: ABBREVIATION DEFINITIONSAPPENDIX 2A: STORC E-LEARNING MODULES – AHSAPPENDIX 2B: STORC E-LEARNING MODULES – COVENANT 109113114115116118119120122INITIAL NEWBORN ASSESSMENT RECORD123Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 4 of 157
INITIAL NEWBORN ASSESSMENT RECORD: A GUIDE TO COMPLETION125INTRODUCTION1.0 BIRTH INFORMATION2.0 VITAL SIGNS3.0 MEDICATION4.0 PHYSICAL OBSERVATIONS5.0 COMPLETION126127127128128132NEWBORN CLINICAL PATH133INFANT FEEDING RECORD135NEWBORN CLINICAL PATH & INFANT FEEDING RECORD: A GUIDE TO COMPLETION136INTRODUCTION137ABOUT THE NEWBORN NURSING CARE PATHWAY1371.0 BIRTH SUMMARY – REFER TO NEWBORN INITIAL ASSESSMENT, DELIVERY RECORD, AND OTHER PERTINENT DOCUMENT TO2.0 CLINICAL OBSERVATION3.0 INTAKE AND OUTPUT SUMMARY4.0 NEWBORN ASSESSMENT5.0 INFANT FEEDING RECORD138139140141143MATERNAL POSTPARTUM AND NEWBORN CLINICAL PATHS144CASE SCENARIO #1144BIBLIOGRAPHY154ASSIST WITH COMPLETIONDeveloped by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 5 of 157
INTRODUCTION TO ALBERTA POSTPARTUM AND NEWBORN CLINICAL PATHWAYSCurrently, 50 hospitals in Alberta provide obstetrical service. There are variances in practices related toassessment, management (for both normal and complex conditions), documentation, healthcare providerskills, patient expectations, and education provided between facilities and communities. As a result, theneed for provincial, evidenced-based pregnancy clinical pathways has been identified as a provincial priorityby the Maternal Newborn Child & Youth (MNCY) Strategic Clinical Network (SCN ), as well as the ProvincialCommunity and Rural Maternal Services Steering Committee.Pregnancy clinical pathways fall into 5 categories:1.2.3.4.5.Birth: Ready or NotPregnancyLabor and BirthPostpartum and Newborn CareCommunity Postpartum Resources and CareThe AHS Normal Postpartum and Newborn nursing pathways were adapted to the Alberta context withpermission from Perinatal Services, BC. The pathways have been trialed, implemented, evaluated and willcontinue to be as required.The pathways support continuity of care between care providers by promoting consistencies in assessmentand documentation, thereby reducing the variation in practice. It provides the nurse, caring for the motherand newborn from 0-72 hours of age, with evidenced-based knowledge and references related to expectednormal assessment findings and care practices that signal mother/baby readiness for discharge. Variancesfrom the expected normal serve as key decision points for the nurse related to care options andinterventions.The pathways will continue to be reviewed, updated, and revised annually (or as required) so health careproviders may have the most current evidenced-based information readily available to support them in theirpractice.Unlike the original rollout of the pathway in September of 2016, a “paper” document will not be part ofsubsequent versions however, the most current and up-to-date documents, tools, and resources may beaccessed the MNCY SCN webpage 5.aspx.Questions or commentary about the pregnancy pathways may be directed to:maternalnewbornchildyouth.scn@ahs.ca.Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 6 of 157
ACKNOWLEDGEMENTSThe Maternal Newborn Child and Youth (MNCY) Strategic Clinical Network (SCN ) would like to acknowledgethe Pregnancy Pathways Committee and Working Group members for their contributions to the development,update, and revision of these pathways.Committee gWilsonRadhaChariSherylScottCommittee illoughbyKimBrunetWoodLaureenMcPeakMaureen cutive Director - MNCY, SCN Director- Maternal Child and Ambulatory Care Services - Red DeerManager - Obstetrics - Grande PrairieObstetrician/Gynecologist - Women’s Health - Calgary ZoneObstetrician/Gynecologist- Women’s Health - Edmonton ZonePostpartum/Newborn Pathways Project ManagerFamily Physician - Calgary ZoneClinical Educator- South Health Campus- CalgaryClinical Informatics Lead - Clinical Knowledge, Clinical ManagementArea Manager - Prenatal Community Services- CalgaryMidwife - CalgaryClinical Lead - Clinical Knowledge, Content ManagementManager- Labor, Delivery, Postpartum - Rockyview General Hospital - CalgaryFamily Physician - ProvostObstetrician/ Gynecologist - Medicine HatMedical Officer of HealthPatient Family AdvisorObstetrical Educator - North Zone - High LevelDirector- Nutrition Services - Child Health Strategy - EdmontonProgram Manager - Maternal Health - Public Health - EdmontonDirector - Healthy Children and Families - Population/Family HealthAssistant Scientific Director - MNCY, SCN Coordinator - Alberta Perinatal Health ProgramObstetrician/Gynecologist - Associate Zone Medical Director - Central ZoneManager – Obstetrics - South Health Campus - CalgaryA very special thank you goes to the following people for their significant contribution of expertise, time, and passion, to ensurenursing staff everywhere in Alberta, have access to evidenced based information to guide their practice.Suzanne KoopmansClinical Educator - Obstetrics Red Deer Regional HospitalAngela CurranObstetrics Lead - Central ZoneNora LandonStaff Nurse - Red Deer Regional HospitalVicki TougasManager - Obstetrics - LethbridgeJennifer WeinkaufStaff Nurse - Grande PrairieUrsula SzulczewskiManager, MNCY SCN (Document maintenance – updates/revisions)Christine HallAdministrative Assistant to Debbie LeitchAdministrative Assistant to Sandi SebastianTara TymDeveloped by the Maternal Newborn Child & Youth Strategic Clinical Network , 2016.Adapted with permission from Perinatal Services BC, Postpartum and Newborn Nursing Care Pathways, 2011.While every attempt has been made to ensure that the information contained herein is clinically accurate and current, AHS acknowledges that manyissues remain controversial, and, therefore, may be subject to practice interpretation.Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 7 of 157Note: Where current Zone or Site protocols exist, adherence to those specific protocols would supercede this document; Physician judgment wouldalso take precedence. Where required, patient education is tailored to the patient’s specific needs.
PostpartumClinicalPathwayDeveloped by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 8 of 157
IntroductionCompletion of the STORC (Strategies for Teaching Obstetrics to Rural and Urban Communities) educational modules, developed andmaintained by the Alberta Perinatal Health Program, are a recommended pre-requisite to successful implementation of the Alberta PregnancyPathways.About the Postpartum Nursing Care Pathway:The Postpartum Nursing Care Pathway identifies the goals and needs of postpartum women. It is the foundation for documentation on thePostpartum Clinical Path (for Vaginal and Caesarean Delivery). To ensure all of the assessment criteria are captured, they have been organized inalphabetical order into these main sections: Physiological HealthInfant FeedingLifestylePsychosocial HealthCommunicable DiseasesWhile the maternal assessment criteria are presented as discrete topic entities, it is not intended that they be viewed as separate from oneanother. For example, the maternal physiological changes affect her psychosocial health. To assist with this, cross-referencing is usedthroughout the document (will be seen as “Refer to ”). This is also evident when referencing to newborn criteria in the Newborn Nursing CarePathway. The mother and newborn are considered to be an inseparable dyad, with the care of one influencing the care of the other. Anexample of this is with breastfeeding as it affects the mother, her newborn, bonding and attachment.In this document, assessments are entered into specific periods; from immediately after birth to 7 days postpartum and beyond. These areguidelines and are used to ensure that all assessment criteria have been captured. Once the woman is in her own surroundings, assessments willbe performed based on individual nursing judgment in consultation with the mother.Underlying Principles: Patient and Family centered care empowers and prepares women for motherhood.Clinical practice is based on research and best evidence and supported through knowledge translation strategies.Pregnancy is considered normal, but dynamic, and risk assessment and management is integral to each phase.Health Care Providers have access to knowledge, tools, and resources and are prepared to support the woman and family through bothnormal and variant pathways.Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 9 of 157
Collaborative relationships between all members of the health care team across the continuum, locally and provincially, support accessto required levels of care or support.Trauma informed care supports all pregnancy pathways.Statement of Women-Centered Care:The Postpartum Nursing Care Pathway assumes that informed decision making is used when care is offered. As stated by the Canadian NursesAssociation Code of Ethics for Registered Nurses, “Informed consent is based on both a legal doctrine and an ethical principle of respect for anindividual’s right to sufficient information to make decisions about care, treatment and involvement in research.”The United Nations states that gender is a primary determinant of health. Health Canada recognizes the potential biases women experience inhealth care where “women’s health is determined not only by their reproductive functions, but also by biological characteristics that differ fromthose of men (sex), and by socially determined roles and relationships (gender)”.The framework of Women-Centered Care is used which respects women’s diversity, supports the way women provide for their health needs inthe social, cultural and spiritual context of their experience, addresses the barriers to access services, and places the women and her newborn atthe center of care that was used. It also assures that women, their partners and families are treated with kindness, respect and dignity, even ifthey differ from the caregiver’s recommendations. In certain circumstances (such as maternal mental health or child maltreatment) nursingjudgment and/or reporting requirements may override a woman’s decision.Referring to a Primary Health Care Provider (PHCP):Prior to referring to a Primary Health Care Provider (PHCP) an appropriate postpartum nursing assessment will be performed. This may need tobe specific or global (physical, emotional, & psychosocial health, learning needs for self-care and care of her infant) in nature. In the interventionsections the nursing process will be referred to as Nursing Assessment.Resources:A list of key resources for both health care professionals and parents is listed at the end of this document.Timeframes:The first 2 hours following the third stage of birth (delivery of placenta) is the Period of Stability. The consensus symposium defined ‘The Periodof Stability’ as “maternal stability is generally attained within two hours following birth.” Other important timeframes identified by thedevelopment committee are: 2–24 hours, 24–72 hours, and 72 hours–7 days and beyond and are the reference points used in thisdocument.Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 10 of 157
NOTE: In order to capture key parent teaching/anticipatory guidance concepts, these concepts will be located in the 2–24 hour timeframe. It isat the individual nurse’s discretion to provide this information and or support earlier or later.Maternal Physiological Stability:The Postpartum Nursing Care Pathway recommends that the five (5) following criteria define postpartum physiologic stability for a delivery atterm. Vital signs stable (T, P, R, BP)Perineum intact or repaired as needed or abdominal dressing dry and intactNo postpartum complications requiring ongoing observation (e.g. hemorrhage)Bladder function adequate (e.g. has voided/Foley catheter draining)Skin-to-skin contact with babyPostpartum Pain and the Visual/Verbal Analogue Scale (VAS):Acute post-partum pain is a strong predictor of persistent depression after childbirth. Severity of acute postpartum pain, not mode of delivery, isindependently related to postpartum pain (2.5 fold increased risk) and depression (3.0 fold increased risk). In order to assess postpartum painand to improve maternal outcomes, the standardized method of using the Visual/Verbal Analogue Scale (VAS) is recommended. The painassessment incorporates a visual or verbal pain plus 4 pain assessment questions.For the purpose of these guidelines a verbal pain assessment will be incorporated.The following questions should be part of the maternal path assessment.1. Location: Where is the pain?2. Quality: What does the pain feel like?3. Onset: When did your pain start?4. Intensity: On a scale of 0 to 10 (with 0 no pain and 10 worst pain possible) where would your pain be? (Pain Scale is used onPostpartum Clinical Care Path)5. What makes the pain better?6. What makes the pain worse?Developed by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 11 of 157
Physiological Health: Vital SignsPhysiological AssessmentVITAL SIGNS:Assess: Vital signs History and risks How patient feels related to vital signsSuggested frequency for vital signs:Vaginal Birth: q15 x 4 (delivery room) q30 x 2 q4h x 2 q shift until dischargeSuggested frequency of vital signs forCesarean Birth with Spinal Anesthesia: q15 x 4 (recovery room) On arrival to unit q30 x 2 q4h x 24 hours q shift until dischargeCesarean Birth (General Anesthesia): q15 x 4 (recovery room) On arrival to unit q30 x 2 q1h x 2 q4h x 24 hours q shift until discharge*Variances, history, or risk factors maydictate more frequent observations.0 - 2 HoursPERIOD OF STABILITY (POS) 2 - 24 HoursNORM AND NORMALVARIATIONS: Asymptomatic Temp: 36.70C–37.90C BP: Systolic: 90–140 BP: Diastolic: 50-90 Resps: 12 -24, unlabored Pulse: 55 – 100 bpm SpO2: 92-100%NORM AND NORMALVARIATIONS: 24 - 72 HoursNORM AND NORMALVARIATIONS:o Refer to PERIOD OF STABILITY o Refer to PERIOD OF STABILITYClient Education/ AnticipatoryGuidance: To notify nurse if feelingunwellClient Education/AnticipatoryClient Education/AnticipatoryGuidance:Guidance:o Refer to PERIOD OF STABILITY o Refer to PERIOD OF STABILITYo Variances that may requireVariance:follow-upo Refer to PERIOD OF STABILITYVariance:Intervention: Refer to 0–24 hourso Refer to PERIOD OF Temperature: 380CSTABILITYVariance: Chills, headache, blurredvision, light headedness,palpitations febrile, labored/depressedrespirations, variant vitalsignsIntervention:o Refer to PERIOD OF STABILITYo Fever managementIntervention: Nursing Assessment Refer to appropriate PHCP,as requiredAssess woman’s understanding of: Her vital signsDeveloped by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 12 of 157 72 Hours - 7 Days(and beyond)NORM AND NORMALVARIATIONS:o Variances that may requirefollow-upClient Education/Anticipatory Guidance: Refer to 0–72 hours May experience increasein temperature with milkcoming down,engorgementVariance: Refer to 0–72 hoursIntervention: Refer to 0-72 hours
Physiological Assessment0 - 2 HoursPERIOD OF STABILITY (POS) 2 - 24 Hours 24 - 72 Hours 72 Hours - 7 Days(and beyond)VITAL SIGNS:Assess woman’s capacity to: Identify variances and report if sherequires further medical assessment(s) Refer to: PainHISTORY OR RISK FACTORS THAT MAYIMPACT VITAL SIGNS:FREQUENCY:In addition to vital signmeasurement, assess for adequacy ofventilation when neuraxial analgesia isadministered and there are notspecific Anesthesia Orders:Respiratory rate, depth, oxygenation(SpO2 when appropriate) q1h X12 hours, then q2h X 12 hoursNOTE: Adequacy of ventilationassessment may be done withoutdisturbing a sleeping patient, unlessconcerns.*The following are in addition to the Norm and Normal Variations, Variances, and Interventions for Vital Signs as above.NORM AND NORMALVARIATIONS: Resps: 12 -24, regularrhythm, unlabored, normaldepth SpO2: 92-100%Client Education/ AnticipatoryGuidance: Neuraxial opioids maycause respiratorydepression To notify nurse if havingdifficulty with breathingNORM AND NORMALVARIATIONS:o Refer to PERIOD OFSTABILITYClient Education/AnticipatoryGuidance:o Refer to PERIOD OFSTABILITYVariance:o Refer to PERIOD OFSTABILITYIntervention:o Refer to PERIOD OFSTABILITYNORM AND NORMALVARIATIONS:o Refer to PERIOD OFSTABILITYClient Education/AnticipatoryGuidance:o Refer to PERIOD OFSTABILITYVariance:o Refer to PERIOD OFSTABILITYIntervention:o Refer to PERIOD OFSTABILITYVariance: Labored/depressedrespirations, tachypnea,bradypnea SpO2 92%Intervention: Nursing Assessment,increased monitoring Supplemental oxygenadministration (ifindicated) Elevate head of bedDeveloped by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 13 of 157NORM AND NORMALVARIATIONS:o Refer to PERIOD OFSTABILITYClientEducation/AnticipatoryGuidance:o Refer to PERIOD OFSTABILITYVariance:o Refer to PERIOD OFSTABILITYIntervention:o Refer to PERIOD OFSTABILITY
0 - 2 HoursPERIOD OF STABILITY (POS)Physiological Assessment 2 - 24 Hours 24 - 72 Hours 72 Hours - 7 Days(and beyond)VITAL SIGNS: Assess the Sedation Score when generalanesthesia or neuraxialanesthesia/analgesia is administered: q1h X 12 hours, then q2h X 12 hoursSedation Score0 Alert1 Sometimes drowsy2 Frequently drowsy, easy to arouse3 Somnolent, difficult to arouseS Normal sleep, easy to arouseDo not administer otherOpioidsRefer to appropriate PHCP,as requiredNORM AND NORMALVARIATIONS: Sedation Score - 0, 1 or SClient Education/AnticipatoryGuidance: Neuraxial opioids maycause drowsiness, sedationand respiratory depression Sedation precedes opioidinduced respiratorydepression; thereforeassessing the sedationscore can preventexcessive sedation orrespiratory depressionfrom developing.NORM AND NORMALVARIATIONS:o Refer to PERIOD OFSTABILITYClient Education/AnticipatoryGuidance:o Refer to PERIOD OFSTABILITYVariance:o Refer to PERIOD OFSTABILITYIntervention:Refer to PERIOD OF STABILITYNORM AND NORMALVARIATIONS:o Refer to PERIOD OF STABILITYClient Education/AnticipatoryGuidance:o Refer to PERIOD OF STABILITYVariance:o Refer to PERIOD OF STABILITYIntervention:o Refer to PERIOD OF STABILITYVariance: Altered level ofconsciousness, increasinglevel of sedation (SedationScore – 2, 3)Intervention: Nursing Assessment Refer to appropriate PHCPDeveloped by the Maternal Newborn Child & Youth SCN Version 4.2 – September 2020Page 14 of 157NORM AND NORMALVARIATIONS:o Refer to PERIOD OFSTABILITYClientEducation/AnticipatoryGuidance:o Refer to PERIOD OFSTABILITYVariance:o Refer to PERIOD OFSTABILITYIntervention:o Refer to PERIOD OFSTABILITY
Physiological Health: PainPhysiological AssessmentPAIN:Assess: Pain using a visual/verbal analogue painscale (VAS) and pain assessmentquestions:o Location: Where is your pain?o Quality: What does your pain feel like?o Onset: When did your pain start?o Intensity: On a scale of 0 (no pain) to10 (worst pain possible) how would yourate your pain?o What makes pain better?o What makes pain worse? Effectiveness of comfortmeasures/analgesiaAssess woman’s awareness of: Comfort measures and/or analgesia(including doses, frequency andeffectiveness) Increased pain may increase risk ofdeveloping chronic pain and/ordepressionRefer to: Newborn Nursing Care Pathway: VitalSigns Newborn Nursing Care Pathway: Behavior Breastfeeding Abdomen/Fundus0 - 2 HoursPERIOD OF STABILITY (POS)NORM AND NORMAL VARIATIONS: Pain is tolerable with/without analgesiaand/or non-pharmacological pain reliefmeasures Pain does not impact daily living, such aswalking, mood, sleep, interactions withothers and ability to concentrate After painsClient Education/Anticipatory Guidance: When and how to report pain level Importance of pain management Current recommendation re: cautious useof Codeine when breastfeeding After pains are normal and a sign ofuterine involutionVariance: Pain impacts daily living, such as walking,mood, sleep, interactions with others andability to concentrate Pain scale 4 for vaginal birth and 5 forcesarean birth that is not relieved bycurrent analgesia and/or nonpharmacological pain relief measuresIntervention: Pain scale 4 for vaginal birth and 5 forCesarean section requires furtherevaluation and management of pain Nursing Assessment Follow specific Zone guidelines for painmanagement, as required Refer to appropriate PHCP, as requiredDeveloped by the Maternal Newborn Child & Youth SCN 2 - 24 HoursNORM AND NORMALVARIATIONS:o Refer to PERIOD OF STABILITYClient Education/AnticipatoryGuidance:o Refer to PERIOD OF STABILITYVariance:o Refer to PERIOD OF STABILITYIntervention:o Refer to PERIOD OF STABILITYVariance – Spinal Headache: Postdural (Spinal) headache(headache worsens whenpositioned upright andimproves when supine)Intervention – Spinal Headache: Further evaluation andmanagement of spinalheadache Follow specific Zoneguidelines for painmanagement, as required Refer to AnesthesiologistVersion 4.2 – September 2020Page 15 of 157 24 - 72 HoursNORM AND NORMALVARIATIONS: Level of pain isdiminishingClient Education/Anticipatory Guidance: Refer to PERIOD OFSTABILITY Confer with PHCP re:pain managementafter hospitaldischargeVariance: Refer to PERIOD OFSTABILITYIntervention: Follow specific Zoneguidelines for painmanagement, asrequired Refer to PERIOD OFSTABILITY 72 Hours - 7 Days(and beyond)NORM AND NORMALVARIATIONS: Refer to 0–72 hoursClient Education/Anticipatory Guidance: Refer to 0–72 hours After pains begin tosubside after about3-5 daysVariance: Refer to 0–72 hoursIntervention Refer to 0–72 hours
Physiological Health: Abdomen/FundusPhysiological AssessmentABDOMEN/FUNDUS:Assess: Fundus for involutiono Palpate fundus with 2nd handsupporting uterus just above symphysis(woman in supine position, kneesflexed, and empty bladder)Assess woman’s understanding of: Normal involution progressionAssess woman’s capacity to: Self-check for involution progression Identify variances that may require furthermedical assessmentRefer to: Lochia Pain Elimination - Urinary Function Vital Signs0 - 2 HoursPERIOD OF STABILITY (POS)NORM AND NORMAL VARIATIONS: Fundus firm, central /- 1 fingerabove/below umbilicus Use minimum pressure to assessfundal height for Cesarean Birth Absence of S & S of infectionClient Education/Anticipatory Guidance: Importance of emptying her bladderfrequently Woman able to demonstrate palpation(if she desires)Variance – Fundus: Uterus – boggy, soft, deviated to oneside (due to retained products,distended bladder, uterine atony,bleeding) Elevated 1 finger above umbilicusIntervention – Fundus: Massage uterus (if boggy) Ensure empty bladder May require further interventions –e.g. intravenous, uterotonicmedication(s), catheterization ofbladder Nursing Assessment Refer to appropriate PHCP, as requiredVariance – Infection: Infection S & S: T 380C, elevated pulse,chills, anorexia, nausea, fatigue,lethargy, pelvic pain, foul smellingDeveloped by the Maternal Newborn Child & Youth SCN 2 - 24 HoursNORM AND NORMALVARIATIONS: Refer to PERIOD OFSTABILITY Rectus muscle intactClient Education/Anticipatory Guidance: Refer to PERIOD OFSTABILITY S & S of infectionVariance –Fundus and Infection: Refer to PERIOD OFSTABILITY Elevated beyond previousassessmentsIntervention –Fundus and Infection: Refer to PERIOD OFSTABILITYVariance –Diastasis Recti Abdominis: Evidenced by bulging orgaping in the midline ofabdomenIntervention –Diastasis Recti Abdominis:Version 4.2 – September 2020Page 16 of 157 24 - 72 HoursNORM AND NORMALVARIATIONS: Fundus firm, central,1–2 fingers belowumbilicus - goes downby 1 finger (1cm)breadth/dayClient Education/Anticipatory Guidance: Refer to 0–24 hoursVariance: Elevated beyondprevious assessments Refer to 0–24 hoursIntervention: Refer to 0–24 hours 72 Hours - 7 Days(and beyond)NORM AND NORMALVARIATIONS: Fundus central, firmand 2–3 fingers belowumbilicus Involuting anddescending 1 fingerbreadth (1 cm)/day.Fundus is not palpableat 7–10 dayspostpartum, returns topre-pregnant state at6 weeks postpartumClient Education/Anticipatory Guidance: Refer to 0–24 hoursVariance: Refer to 0–24 hoursIntervention: Refer to 0–24 hours
Physiological Assessment0 - 2 HoursPERIOD OF STABILITY (POS) 2 - 24 HoursABDOMEN/FUNDUS:and/or profuse l
table of contents introduction to alberta postpartum and newborn clinical pathways 6 acknowledgements 7 postpartum clinical pathway 8 introduction 9 physiological health: vital signs 12 physiological health: pain 15 physiological health: lochia 18 physiological health: perineum 19 physiological health: abdominal incision 20 physiological health: rh factor 21 physiological health: breasts 22
US intrauterine pregnancy: reproducible loss heart activity, failure increase CRL over 1 w or persisting empty sac at 12 w Ectopic pregnancy blood/urine hCG, gestational sac outside uterus Heterotopic pregnancy Intrauterine ectopic pregnancy Pregnancy of unknown location (PUL) No identifiable pregnancy on US with blood/urine hCG
Discuss prevalence of teenage pregnancy. 2. Discuss pregnancy screening in teen population. 3. Identify pregnancy risks associated with teenage pregnancy for the mother. 4. Discuss medical impacts associated with teenage pregnancy for the fetus/infant. 5. Discuss social implications of teenage pregnancy. 6. Discuss risk for repeat unintended .
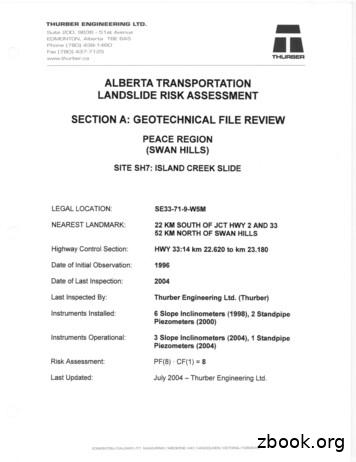
EDMONTON, Alberta TOE 6A5 Phone (780) 438-1460 Fax (780) 437-7125 www.thurber.ca ALBERTA TRANSPORTATION LANDSLIDE RISK ASSESSMENT MR THURBER . Alberta (83-0)." 5. Alberta Research Council, 1976. "Bedrock Topography of the Lesser Slave Lake Map Area, NTS 83 0, Alberta." 6. University and Government of Alberta, 1969. "Atlas of Alberta."
This means ensuring that the agencies, sectors and services involved are linked, and pathways between them forged, so that young people do not fall through the cracks of patchy provision and inconsistent or inappropriate signposting. Defining pregnancy pathways Comprehensive pregnancy pathways require SRE to be of high
4. Pre-pregnancy Obese Weight Range Weight Gain Grids for Twin Pregnancy (Rev. 1/13) 5. Pre-pregnancy Normal Weight Range (Twins) 6. Pre-pregnancy Overweight Range (Twins) 7. Pre-pregnancy Obese Weight Range (Twins) Source: IOM (Institute of Medicine) and NRC (National Research Council). 2009. Weight Gain During Pregnancy: Reexamining the .
Ectopic pregnancy-Right Tubal Pregnancy Blastocyst implants at abnormal site outside uterus Sites: Uterine tubes (tubal pregnancy) Ovary (ovarian pregnancy) Abdominal cavity (abdominal pregnancy) Intrauterine portion of uterine tubes (cornual pregnancy)
Wellness in Pregnancy Medications in Pregnancy Good nutrition in pregnancy Building blocks for a healthy pregnancy Weight gain in pregnancy . Laxatives (Peri-Colace, Dulcolax) Hemorrhoid relief: Tucks Preparation H with hyd
criminal case process; the philosophies and alterna-tive methods of corrections; the nature and processes of treating the juvenile offender; the causes of crime; and the role of government and citizens in finding solutions to America’s crime problems. 2. Develop, state, and defend positions on key issues facing the criminal justice system, including the treatment of victims, police-community .