Pulmonary Hypertension Final 2.ppt - Cdn.ymaws
3/4/2016 Objectives Pharmacist Objectives: Treatment of Pulmonary Hypertension – Identify the pathophysiology, clinical presentation, and diagnostic criteria for pulmonary hypertension – Review treatment goals and strategies for each pulmonary hypertension functional class – Discuss new and emerging therapies for the treatment of pulmonary hypertension Janet Job PGY-1 Pharmacy Practice Resident Memorial Regional Hospital March 12, 2016 www.fshp.org 3 Disclosure Objectives Technician Objectives: The speaker cannot identify any potential conflict of interest and has no relationships that should be disclosed – Discuss the clinical presentation of pulmonary hypertension – Recognize medications used for the treatment of this disease state – Identify dosage forms and administration for pulmonary hypertension therapies 2 4 1
3/4/2016 Epidemiology Definition The age-standardized death rate in the USA ranges between 4.5 and 12.3 per 100,000 population Women accounted for 61% of all pulmonary hypertension hospitalizations in 2001-02 and 63% in 2009-2010 Over the past decade, death rates for black patients were approximately 40% higher than white patients Pulmonary hypertension (PH) pulmonary arterial hypertension (PAH) Abnormal elevated pressures in the pulmonary vasculature which often results in right ventricular failure Characterized by different pathological lesions in the pulmonary vasculature depending on the underlying cause Pulmonary Hypertension Surveillance: United States 2001 to 2010. CHEST Journal. Available at: spx?articleid 1857526. Accessed January 13, 2015. Pulmonary Hypertension Fact Sheet. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/dhdsp/data statistics/fact sheets/fs pulmonary hypertension.htm. Accessed January 13, 2015. 5 7 Haeck ML, Vliegen HW. Diagnosis and treatment of pulmonary hypertension. Heart. 2015;101(4):311-9. Prevalence Pathophysiology Age-Standardized Death Rates of Pulmonary Hypertension as Any Cause of Death Among All Ages by State, 2010 Ohm’s Law – – – – Change in pressure flow x resistance Ppa - Ppv CO x PVR Ppa (CO x PVR) Ppv The Ppv is estimated by the pulmonary capillary wedge pressure (PCWP) Ppa (CO x PVR) PCWP Pulmonary hypertension mean pulmonary artery pressure (mPAP) 25 mmHg at rest Pulmonary Hypertension Fact Sheet. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/dhdsp/data statistics/fact sheets/fs pulmonary hypertension.htm. Accessed January 13, 2015. 6 Key Ppa mean pulmonary arterial pressure Ppv mean pulmonary venous pressure CO right-sided cardiac output PVR pulmonary vascular resistance 8 2
3/4/2016 Pathophysiology Signs and Symptoms Ppa (CO x PVR) PCWP Increased flow: Atrial/ ventricular septal defects Patent ductus arteriosus Liver cirrhosis Increased pulmonary vascular resistance: Idiopathic PAH Connective tissue disease HIV infection Congenital heart disease Pulmonary emboli Interstitial lung disease Hypoventilation syndromes Parenchymal lung disease RIGHT VENTRICULAR FAILURE Increased pulmonary venous pressure: Mitral valve disease Left ventricular systolic or diastolic dysfunction Constrictive pericarditis Restrictive cardiomyopathy Pulmonary venous obstruction (eg, pulmonary veno-occlusive disease) Dyspnea Fatigue Chest pain Syncope Peripheral edema Palpitations 9 11 Haeck ML, Vliegen HW. Diagnosis and treatment of pulmonary hypertension. Heart. 2015;101(4):311-9. Pathogenesis Clinical Classification 1. Pulmonary Arterial HTN (PAH) 3. PH Owing to Lung Diseases and/or Hypoxia Idiopathic PAH Heritable PAH Drug- and toxin-induced PAH Persistent PH of newborn Associated with: CTD HIV infection portal hypertension CHD schistosomiasis chronic hemolytic anemia 1’. PVOD and/or PCH 2. PH Due to Left Sided Heart Disease 10 Gaine S. Pulmonary hypertension. JAMA. 2000;284:3160–3168. Systolic dysfunction Diastolic dysfunction Valvular disease COPD ILD Other pulmonary disease with mixed restrictive and obstructive pattern Sleep disordered breathing Alveolar hypoventilation disorders Chronic exposure to high altitude Developmental abnormalities 4. CTEPH 5. PH with Unclear Multifactorial Mechanisms Hematologic disorders Systemic disorders Metabolic disorders Others Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34-41. 3
3/4/2016 Unexplained dyspnea and/or suspected pulmonary hypertension Drug and Toxin Induced PAH Definite Aminorex Fenfluramine Dexfenfluramine Toxic rapeseed oil Benfluorex Likely Amphetamine L-tryptophan Methamphetamines Possible Cocaine Phenylpropanolamine St. John’s Wort Chemotherapeutic agents SSRI’s Pergolide Unlikely Oral contraceptives Oestrogen Cigarette smoking Group 2 (Left Heart Disease) or Group 3 (Pulmonary disease) likely? History- Symptoms- SignsECG-lab tests- pulmonary function test- 6 minute walk test- HRCT- MRI- ECHO YES Segmental perfusion defects Ventilation perfusion scan Consider Group 4 (CTEPH) or group 1 (PVOD) MPAP 25 mmHg; PCWP 15 mmHg Right heart catheterization PAH Search for other causes Start treatment Regular follow-up (ECG – 6MWT – exercise testing – lab tests- ECHO- RHC) 13 15 Haeck ML, Vliegen HW. Diagnosis and treatment of pulmonary hypertension. Heart. 2015;101(4):311-9. Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34-41. Diagnosis Functional Assessment: PAH PH is commonly diagnosed at a late stage of the disease and is associated with poor survival 6-minute walk test Chest X-Ray ECG CT scan Pulmonary function test ECHO Right heart catheterization 14 Haeck ML, Vliegen HW. Diagnosis and treatment of pulmonary hypertension. Heart. 2015;101(4):311-9. Treat underlying disease and check for progression Class I Class II Class III Class IV Patients with PH but without resulting limitation of physical activity Ordinary physical activity does not cause undue dyspnea or fatigue, chest pain, or near syncope Patients with PH resulting in slight limitation of physical activity They are comfortable at rest. Ordinary physical activity causes undue dyspnea or fatigue, chest pain, or near syncope Patients with PH resulting in marked limitation of physical activity They are comfortable at rest. Less than ordinary activity causes undue dyspnea or fatigue, chest pain, or near syncope Patients with PH with inability to carry out any physical activity without symptoms. These patients manifest signs of right-heart failure. Dyspnea and/or fatigue may even be present at rest. Discomfort is increased by any physical activity Rubin LJ. Diagnosis and management of pulmonary arterial hypertension: ACCP Evidence-Based Clinical Practice Guidelines. Introduction. Chest. 2004;126:7S-10S. 16 4
3/4/2016 Treatment Goals Treatment: PAH Specific Measures Vasoreactivity test positive Alleviate symptoms Decrease progression of disease Improve functional class, exercise capacity, and quality of life Improve pulmonary hemodynamics Prolong survival Calcium channel blocker Vasoreactivity test negative ERA (FC II, III, and IV) PDE-5 Inhibitors (FC II, III, and IV) Prostacyclin analogues (FC III and IV) In case of inadequate response In case of inadequate response 17 Balloon atrial septostomy Lung transplantation Surgical therapy Pulmonary endarterectomy in case of appropriate selected CTEPH patients Sequential combination therapy In case of inadequate response 19 Mclaughlin VV, Gaine SP, Howard LS, et al. Treatment goals of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D73-81. Haeck ML, Vliegen HW. Diagnosis and treatment of pulmonary hypertension. Heart. 2015;101(4):311-9. Treatment Goals Vasoreactivity Test for PAH Vasoreactivity testing with: Achieve modified New York Heart Association functional class I or II 6-min walk distance 380 m Normalization of right ventricular size and function on ECHO Decreasing or normalization of B-type natriuretic peptide (BNP) Hemodynamics with right atrial pressure 8 mm Hg and cardiac index 2.5 mg/kg/min – Epoprostenol IV 2-10 ng/kg/min – Adenosine IV 50-250 mcg/kg/min – NO inhaled 10-80 parts per million for 5 minutes Positive response defined as decrease in the pulmonary artery pressure 10 mmHg, a pulmonary artery pressure of 40 mmHg, and an unchanged or increased cardiac output 18 Mclaughlin VV, Gaine SP, Howard LS, et al. Treatment goals of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D73-81. Calcium Channel Blocker Dose Nifedipine 120-240 mg Diltiazem 540-900 mg Amlodipine 2.5-40 mg Agents are titrated every 2-4 weeks to clinical effect Verapamil should be avoided due to negative inotropic effects 20 Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med. 1992;327(2):76-81. 5
3/4/2016 Vasoreactivity Test for PAH Vasoreactivity Test for PAH Long term response to CCB in idiopathic PAH (at least 1 year) Long term response to CCB in non- idiopathic PAH (at least 1 year) In the overall population, 16 PAH patients [2.4% (95% CI 1.2–3.6)] were considered longterm CCB responders: – n 557 – Positive response 10% of IPAH patients Less severe disease at baseline – 12 [9.4% (95% CI 4.4–14.5)] with anorexigen use – 2 [1.6% (95% CI 0–3.8)] with HIV infection – 1 [0.7% (95% CI 0–1.9)] with PoPH – 1 [0.6% (95% CI 0–1.8)] with CTD 12.6% 6.8% Sitbon O, Humbert M, Jaïs X, et al. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation. 2005;111(23):3105-11. 21 Vasoreactivity Test for PAH Montani D, Savale L, Natali D, et al. Long-term response to calcium-channel blockers in non-idiopathic pulmonary arterial hypertension. Eur Heart J. 2010;31(15):1898-907. 23 PAH: Evidence Based Medicine Limitations of Clinical Trials Response in non-idiopathic PAH – Small number of patients – 6.5% of patients had an acute response to vasoreactivity testing (n 43) Sufficiently powered clinical trials uncommon Low prevalence of disease – Short duration 1.6% 12.2% High costs associated with extended length studies to achieve sufficient power 1.3% – Endpoints 10.1% 6MWD- the most common primary endpoint 0% – Established predictor of survival – Consistent relationship has not been observed between change from baseline in 6-MWD and survival, PAH-associated hospitalization, or PAH therapy escalation 13.4% n 663 Montani D, Savale L, Natali D, et al. Long-term response to calcium-channel blockers in non-idiopathic pulmonary arterial hypertension. Eur Heart J. 2010;31(15):1898-907. 22 24 Ryan JJ, Rich JD, Maron BA. Building the case for novel clinical trials in pulmonary arterial hypertension. Circ Cardiovasc Qual Outcomes. 2015;8(1):114-23. 6
3/4/2016 Treatment Prostacyclin Analogues Prostacyclin Analogues Prostacyclin analogues – – – – Epoprostenol (Flolan , Veletri ) Treprostinil (Remodulin , Tyvaso , Orenitram ) Iloprost (Ventavis ) Selexipag (Uptravi ) Endothelin-1 receptor antagonists (ERAs) – Ambrisentan (Letairis ) – Bosentan (Tracleer ) – Macitentan (Opsumit ) Drug Route of Usual Starting Dose and Administration Titration Schedule Half-life Adverse Effects Epoprostenol (Flolan , Veletri ) Veletri- room temperature stable Continuous infusion via central IV line; place catheter 2 ng/kg/min increased by 1-2 ng/kg/min every 15 minutes until dose limiting side effects occurs 2.7 min Central line infections, flushing, N/V, hypotension, headache, flulike symptoms, jaw pain 1.25 ng/kg/min increased by 1.25 ng/kg/min weekly for first 4 weeks then 2.5 ng/kg/min thereafter 4 hours Headache, N/V, infusion site reactions and pain, flulike symptoms, jaw pain Treprostinil Continuous (Remodulin ) infusion via central IV line or continuous SC infusion PDE-5 inhibitors – Sildenafil (Revatio ) – Tadalafil (Adcirca ) cGMP inducer – Riociguat (Adempas ) 25 27 Treatment Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary 26 Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119. Prostacyclin Analogues Drug Route of Usual Starting Dose and Administration Titration Schedule Halflife Treprostinil (Tyvaso ) Oral Inhalation 3 inhalations (total of 18 mcg) 4 4 hours times daily increased by 3 inhalations 4 times a day every 12 weeks until target or max dose 9 inhalations (54 mcg) 4 times daily is reached; space doses by 4 hours Headache, flushing, nausea, cough, throat irritation Treprostinil (Orenitram ) Oral Taken with food 0.25 mg BID or 0.125 mg TID; titrate 0.25 or 0.125 mg BID/TID every 3-4 days Headache, diarrhea, nausea, flushing, jaw pain 4 hours Adverse Effects 28 7
3/4/2016 Prostacyclin Analogues Drug Route of Usual Starting Dose and Administration Titration Schedule Half-life Adverse Effects Iloprost (Ventavis ) Oral Inhalation 2.5 mcg 6-9 times per day (no more frequently than every 2 hours); increase to 5 mcg 6-9 times per day (max 45 mcg) 20-30 min Flushing, hypotension, headache, flu-like symptoms, trismus, cough 200 mcg BID; increase the dose by 200 mcg BID at weekly intervals to the highest tolerated dose up to 1600 mcg BID 6.2-13.5 hours Selexipag (Uptravi ) Oral tablet Prostacyclin Analogues Due to epoprostenol short half life, interrupting drug delivery may lead to rebound PH or death** Selexipag metabolized via CYP2C8 Dose adjustments Headache, diarrhea, jaw pain, nausea, myalgia, vomiting, flushing, rash, arthralgia – Epoprostenol: No renal or hepatic dose adjustments necessary – Oral treprostinil: Mild hepatic impairment, initiate at 0.125 mg BID, Moderate hepatic impairment, avoid use – Selexipag: Moderate hepatic impairment, start dose at 200 mcg once daily and increase dose by 200 mcg once daily at weekly intervals 29 31 Prostacyclin Analogues: Cost Comparison GRIPHON Trial GRIPHON (PGI2 Receptor agonist In Pulmonary arterial HypertensiON) – Event driven, Phase III, randomized double-blind trial comparing selexipag to placebo Patient Population Number of Patients Primary Endpoint Results PAH, age 18-75 yrs; 20% treatment naïve; 47% monotherapy; 33% combination therapy 1,156 Time to first morbidity/mortality Selexipag decreased time to M/M by 40% (HR 0.60; 99% CI: 0.46, 0.78) vs. placebo (log- rank p 0.0001) 30 Sitbon O, Channick R, Chin KM, et al. Selexipag for the Treatment of Pulmonary Arterial Hypertension. N Engl J Med. 2015;373(26):2522-33. Epoprostenol – 0.5 mg vial: 19.44 – 1.5 mg vial: 46.94 Flolan – 0.5 mg vial: 22.43 – 1.5 mg vial: 54.17 Veletri – 0.5 mg vial: 27.07 – 1.5 mg vial: 45.50 Remodulin – 1 mg/mL: 1474.00 – 2.5 mg/mL: 3685.00 – 5 mg/mL: 7370.00 – 10 mg/mL: 14740.00 Tyvaso – 0.6 mg/mL: 585.00 Orenitram – 0.125 mg (10): 58.50 – 0.25 mg (10): 117.00 – 1 mg (10): 468.00 – 2.5 mg (10): 1170.00 Iloprost – 10 mcg/mL (1 mL): 128.40 – 20 mcg/mL (1 mL): 128.40 Selexipag – 200 mcg (60): 11208.00 – 1600 mcg (60): 17424.00 32 8
3/4/2016 Endothelin-1 receptor antagonists (ERAs) Endothelin-1 receptor antagonists (ERAs) Endothelin Receptor Antagonists (ERAs) Drug Route of Administration Usual Starting Dose and Titration Schedule Halflife Adverse Effects Bosentan (Tracleer ) Oral tablet 62.5 mg twice daily for 4 weeks then increase to 125 mg twice daily; if 40 kg, dose remains 62.5 mg twice daily 5 hours Respiratory tract infections, peripheral edema, headache, anemia, cheat pain, syncope; BBW for hepatotoxicity and teratogenicity Ambrisentan Oral tablet (Letairis ) 5 mg daily then increase to 10 mg daily 9-15 hours Peripheral edema, headache, nasal congestion, flushing; BBW for hepatotoxicity and teratogenicity Macitentan (Opsumit ) 10 mg daily (max) 48 hours Nasopharyngitis, bronchitis, anemia. Headache Oral tablet Ambrisentan and bosentan metabolized via CYP2C9 and 3A4 pathways Macitentan metabolized via CYP3A4 Dose adjustments – Bosentan: Not recommended in moderate-severe hepatic impairment – Ambrisentan: Not recommended in moderate-severe hepatic impairment – Macitentan: No adjustments for renal or hepatic dysfunction REMS Program – Tracleer Access Program [TAP] – Letairis Education and Access Program [LEAP] – Opsumit 33 35 Endothelin-1 receptor antagonists (ERAs): Cost Comparison SERAPHIN Trial Study with an Endothelin Receptor Antagonist in Pulmonary Arterial Hypertension to Improve Clinical Outcome (SERAPHIN) Bosentan – 62.5 mg (30): 4932.00 – 125 mg (30): 4932.00 Ambrisentan – 5 mg (30): 8842.73 – 10 mg (30): 8842.73 Macitentan – 10 mg (15): 4311.00 34 36 Pulido T, Adzerikho I, Channick RN, et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369(9):809-18 9
3/4/2016 PDE-5 inhibitors PDE-5 inhibitors: Cost Comparison Revatio PDE-5 Inhibitors Drug – IV Route of Usual Starting Dose Administration and Titration Schedule Halflife Adverse Effects Sildenafil (Revatio ) Oral tablet IV bolus Oral: 5 mg or 20 mg TID (4-6 hours apart) IV: 2.5 or 10 mg TID 4 hours Epistaxis, headache, dyspnea, flushing, NAION, hearing loss Tadalafil (Adcirca ) Oral tablet 40 mg once daily 35 hours Headache, myalgias, nasopharyngitis, flushing, respiratory tract infections, hypotension, hearing or vision loss 10 mg/12.5 mL (12.5 mL): 251.24 – Oral Suspension 10 mg/mL (112 mL): 6561.89 – Tablets (Revatio Oral) 20 mg (90): 3281.09 Adcirca – 20 mg (60): 3002.40 37 39 PDE-5 inhibitors cGMP Inducer Sildenafil and tadalafil metabolized via CYP3A4 Dose adjustments cGMP Inducer Drug – Sildenafil: No dose adjustments necessary – Tadalafil: Mild or moderate renal impairment, start with 20 mg once daily. Severe renal impairment, avoid use. Mild or moderate hepatic impairment, consider starting dose of 20 mg once daily Route of Administration Riociguat Oral tablet (Adempas ) IV bolus Contraindicated with nitrates and riociguat 38 Usual Starting Dose and Titration Schedule Half-life 1 mg TID; 12 hours Increase dosage by 0.5 mg at 2 week intervals as tolerated; MAX 2.5 mg TID Adverse Effects Cost Headache, dyspepsia/gastritis, dizziness, nausea, diarrhea, hypotension, vomiting, anemia, gastroesophageal reflux, and constipation 0.5-2.5 mg tablets (42): 4585.56 40 10
3/4/2016 Combination Therapy cGMP Inducer Dose adjustments: Not recommended in patients with severe renal and hepatic impairment Contraindicated with nitrates and PDE-5 inhibitors REMS Program – Adempas 41 Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and 43 Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119. Combination Therapy Combination Therapy Recommended in patients who do not show an adequate response to single agent treatment – The majority of PAH patients will eventually receive combination therapy In case of inadequate clinical response with double combination therapy, triple combination therapy should be attempted In WHO-FC IV patients initial combination therapy may also be considered Combination therapy can either include an: – ERA PDE-5 inhibitor – Prostacyclin ERA – Prostacyclin PDE-5 inhibitor/sGC stimulator Galiè N, Corris PA, Frost A, et al. Updated treatment algorithm of pulmonary arterial hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D60-72. 42 Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary 44 Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119. 11
3/4/2016 AMBITION Trial Supportive Therapy Randomized, multicenter study of first line ambrisentan and tadalafil combination therapy in subjects with pulmonary arterial hypertension Compared 2 treatment strategies Reduce salt and fluid intake Physical activity within symptom limit Vaccinations – Upfront combo (ambrisentan tadalafil) vs. monotherapy (ambrisentan or tadalafil) Event-driven trial – Influenza – Pneumococcal – 500 newly diagnosed patient with group 1 PAH who had class II or III symptoms compared the combination of 10 mg of ambrisentan and 40 mg of tadalafil with either agent alone Birth control – Pregnancy in patients with PAH has been associated with high mortality rates of 3050% – ERA’s may affect efficacy of oral contraceptives Smoking cessation Administration of oxygen Primary objective: time to clinical failure Secondary objectives: safety and tolerability, 6MWD at peak and trough levels 47 45 AMBITION TRIAL Supportive Therapy The combined regimen administered on average for eighteen months resulted in: Anticoagulation – In PAH there is evidence of coagulopathies with increased risk of thrombosis – Use of oral anticoagulation, in the absence of contraindications should be considered in PAH – CTEPH patients should receive lifelong anticoagulation – The role of NOACs is unknown – Reduction in the rate of clinical failure (18% vs. 31%) – Improved exercise capacity (49 vs. 24 meters) – Decreased hospitalizations Outcome Combination (n 253) Monotherapy (n 247) All cause deaths (%) 3.6 3.2 Hospitalization (%) 4 12 Improvement in 6-minute walking (m) 49.0 23.8 46 Diuretics – Recommended in the case of right sided decompensation Digoxin – May be helpful for inotropic support and maintenance of sinus rhythm Long term oxygen therapy 48 12
3/4/2016 Case Pharmacist Role RH is a 56 yo male who presents to the ED with cellulitis. The physician decides to admit the patient and start IV antibiotics. You proceed to complete a medication reconciliation and the patient reveals he is on an epoprostenol pump. What are some questions you should ask the patient? Avoidance of dosing errors – Dose/weight/concentration/rate Maintain appropriate par levels Nursing in-service 49 51 Macaulay TE, Covell MB, Pogue KT. An Update on the Management of Pulmonary Arterial Hypertension and the Pharmacist's Role. J Pharm Pract. 2015. Case Pharmacist Role Is the medication currently infusing? Which specialty pharmacy do you use to fill the epoprostenol? When does the pump need to be refilled? Medication Reconciliation Work with specialty pharmacy – Ensure medication is available Regulatory compliance (REMS) Medication Access 50 52 Macaulay TE, Covell MB, Pogue KT. An Update on the Management of Pulmonary Arterial Hypertension and the Pharmacist's Role. J Pharm Pract. 2015. 13
3/4/2016 Pharmacist Role References Patient assistance programs – Opsumit Voucher Program 30-day free trial – Adcirca 20 Co-pay Assistance Program – Letairis The Letairis Education and Access Program (LEAP) – Tyvaso Access Solutions and Support Team (ASSIST) Galiè N, Corris PA, Frost A, et al. Updated treatment algorithm of pulmonary arterial hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D60-72. Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119. Gaine S. Pulmonary hypertension. JAMA. 2000;284:3160–3168. Haeck ML, Vliegen HW. Diagnosis and treatment of pulmonary hypertension. Heart. 2015;101(4):311-9. Macaulay TE, Covell MB, Pogue KT. An Update on the Management of Pulmonary Arterial Hypertension and the Pharmacist's Role. J Pharm Pract. 2015. Pulido T, Adzerikho I, Channick RN, et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369(9):809-18. 53 55 Macaulay TE, Covell MB, Pogue KT. An Update on the Management of Pulmonary Arterial Hypertension and the Pharmacist's Role. J Pharm Pract. 2015. Pharmacist Role Side Effect Management Dose titration of prostanoids is limited by patient reported adverse effects Vasodilatory effects – Headaches Analgesics---AVOID NSAIDS – Flushing Cool cloths Lower room temperature References Diarrhea/N&V – Imodium/Lomotil – Antiemetics Central Line infections – Use of appropriate antimicrobial agent – Prostanoids may be temporarily infused through a dedicated peripheral line – Treprostinil may be given subQ – Nasal congestion Saline spray 54 Pulmonary Hypertension Fact Sheet. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/dhdsp/data statistics/fact sheets/fs pulmonary hypertensio n.htm. Accessed January 13, 2015. Pulmonary Hypertension Surveillance: United States 2001 to 2010. CHEST Journal. Available at: spx?articleid 1857526. Accessed January 13, 2015. Rubin LJ. Diagnosis and management of pulmonary arterial hypertension: ACCP Evidence-Based Clinical Practice Guidelines. Introduction. Chest. 2004;126:7S-10S. Ryan JJ, Rich JD, Maron BA. Building the case for novel clinical trials in pulmonary arterial hypertension. Circ Cardiovasc Qual Outcomes. 2015;8(1):114-23. Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34-41. Sitbon O, Channick R, Chin KM, et al. Selexipag for the Treatment of Pulmonary Arterial Hypertension. N Engl J Med. 2015;373(26):2522-33. 56 Macaulay TE, Covell MB, Pogue KT. An Update on the Management of Pulmonary Arterial Hypertension and the Pharmacist's Role. J Pharm Pract. 2015. 14
3/4/2016 Questions? 57 15
Pulmonary hypertension mean pulmonary artery pressure (mPAP) 25 mmHg at rest 8 Key Ppa mean pulmonary arterial pressure Ppv mean pulmonary venous pressure CO right-sided cardiac output PVR pulmonary vascular resistance. 3/4/2016 3 Pathophysiology Ppa (CO x PVR) PCWP 9
Symposium on pulmonary hypertension, pulmonary hypertension is defined as mPAP 20 mm Hg and its subgroup Pulmonary arterial hypertension (PAH) is defined as mPAP 20 mm Hg, PCWP 15 mm Hg and PVR 3 Woods Units. Table 1 : Haemodynamic definitions of pulmonary hypertension, 6th world symposium on pulmonary hypertension, Nice, France.
1.5 Persistent pulmonary hypertension of the newborn 1 . Pulmonary veno-occlusive disease (PVOD) and/or pulmonary capillary hemangiomatosis (PCH) 2. Pulmonary hypertension owing to left heart disease 2.1. Systolic dysfunction 2.2. Diastolic dysfunction 2.3. Valvular disease 3. Pulmonary hypertension owing to lung diseases and/or hypoxia 3.1.
Pulmonary hypertension occurs when there is a vasoconstriction of the pulmonary blood vessels. This leads to right to left shunting across the foramen ovale and ductus arteriosus and subsequent hypoxia. Pulmonary hypertension can be primary (rare) or secondary. Secondary pulmonary hypertension can occur with a number of conditions including:
Pulmonary hypertension is divided into 5 classifications, World Health Organization (WHO) groups 1 to 5, based on underlying cause.33 Recognizing the various origins of pulmonary hypertension is important in the ED because not all patients with pulmonary hypertension are treated in the same manner (Table 1). However, an individual may
with suspected pulmonary arterial hypertension, echocardiography is a key screening tool in the diagnostic algorithm. It provides an estimate of pulmonary artery pressure, either at rest or during exercise, and is useful in ruling out secondary causes of pulmonary hypertension. In addition, echocardiography is valuable in
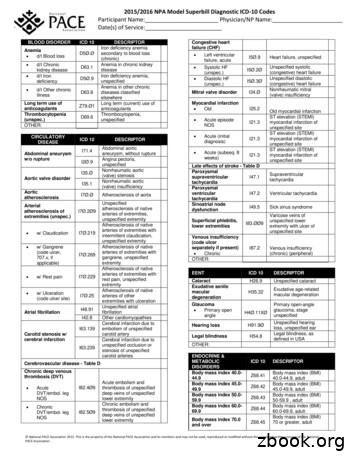
WHO ICD-11 MMS United States ICD-10-CM BA00 Essential hypertension BA00.0 Combined diastolic and systolic hypertension BA00.1 Isolated diastolic hypertension BA00.2 Isolated systolic hypertension BA00.Y Other specified essential hypertension BA00.Z Essential hypertension, unspecified Matching terms:
ICD 10 Table A- HYPERTENSION Hypertension: ICD 10 DESCRIPTOR Benign essential hypertension hypertension I1Ø Essential (primary) Essential hypertension hypertension I1Ø Essential (primary) Hypertensive heart disease:(unspecified) ICD 10
Kesehatan Mata berbasis teknologi pembelajaran modern. 2 2. Menyelenggarakan penelitian dasar, terapan dan inovatif dalam bidang Ilmu Kesehatan Mata untuk menunjang pengembangan pendidikan dan pelayanan. 3. Mendarmabaktikan keahlian yang diperoleh dalam bidang ilmu pengetahuan dan teknologi kepada masyarakat. 4. Mengupayakan usaha pemberantasan kebutaan sesuai dengan program WHO Vision 2020. 5 .