2011 Annual Report - CHNOLA
2011 Annual ReportThe Cancer Program and LaNasa Greco Centerfor Cancer and Blood Disorders
ResourcesOur Team ofMedical ProfessionalsFinancialChildren’s Hospital Main Number.(504) 899-9511Oncology Department. (504) 896-9740Oncology Department Fax . (504) 896-9758Oncology Unit – inpatient. (504) 896-9442Oncology – outpatient clinic. (504) 896-9848Neurosurgery Department. (504) 896-9568Social Services Department. (504) 896-9367Surgery Department. (504) 896-9478Orthopaedics Department. (504) 896-9569Medical Records/Tumor Registry. (504) 896-9585Administration . (504) 896-9450Diagnostic Radiology. (504) 896-9565Lolie C. Yu,MD, DivisionChiefPathology Department.(504)896-9873Director,BoneProgramMarrow TransplantProgram,Bone MarrowTransplant. (504)896-9740Lolie C. Yu,MDChildren’sHospital/LSUMCCancer CommitteeChairman.(504)896-9741Professorof Pediatrics,Cancer ProgramLiaison.(504)896-3977LSU Health Sciences CenterEvans Valerie, MDLSU CCOP/Children's Oncology Group(COG) Principal InvestigatorCancer Information/ResourcesAmerican Cancer Society.(800) ACS-2345American Cancer Society,Renee V. Gardner, MDNew Orleans Chapter. (504) 469-0021Director, Sickle Cell ClinicsNational Cancer Institute .1-800-4CANCERProfessor of Pediatrics,Health SciencesCenterCancerLSUInformationWebsitesAmerican Cancer Society,. www.cancer.orgNational Cancer Institute.www.cancer.govChildren’s Hospital, New Orleans. www.chnola.orgNational ChildhoodJaime Morales,MDwww.curesearch.orgCancer Foundation.Pediatric oncologist, Children's HospitalCancer Care.www.cancercare.orgCancer stantProfessorof Pediatrics,National Children’sLSU Health Sciences CenterCancer Society.www.children-cancer.comMedicaid – Enroller .(504) 896-9152Office of Family Security. (504) 599-1700Social Security. (800) 772-1213Children’s Hospital AssistanceProgram (CHAP).(504) 894-5166American Cancer Society . (504) 469-0021Leukemia/Lymphoma Society .(504) 887-0945Optimist Leukemia Foundation . .(800) 685-9611J.L Foundation. (225) 698-1010National Children’s Cancer Society . .(314) 241-1600Cancer Recovery Fund . (717) 564-4100First Hand Foundation .(816) 201-1569Cancer Association of Greater New Orleans .(504) 733-5539Total Community Action .(504) 304-6676Kids Kicking Cancer.(504) 455-7754HousingCori Morrison, MDPediatricChildren's(504)HospitalRonald McDonaldHouse .oncologist,.468-6668ProfessorAmerican CancerAssistantSociety PatrickF. of PediatricsTaylor Hope Lodge. (504) 219-2202Hotels – medical rates list availablein Social Services DepartmentWishesA Child’s Wish . (504) 367-9474Make-A-Wish .Pinki K. Prasad, MD (504) 846-9474A Special Wish .(614)575-9474Assistant Professor of PediatricsSupportCandlelighters. (800) 366-2223Sperm Bank Reproductive Services. (504) 454-7973Camp Challenge . (504) 347-2267Sunshine Kids . (713) 524-1264Caps for Kids. (504) 891-4277Maria C. Velez, MDPediatric oncologist, Children’s HospitalAssociate Professorof Pediatrics, PediatricRehabilitation shipVia Link (24 hour counseling).(800)Program749-2673Director,LSUHealth Sciences CenterAngel’s Place (RespiteCare).(504)455-2620COPELINE - Suicide Prevention.(800) 273-8255Children’s Hospital Behavioral Health Unit,Calhoun Campus.(504) 896-7200Family Service of GNO. (504) 822-0800Mental HealthDeathCompassionate Friends.(504) 454-5078Seasons – The Center for Caring . (504) 834-1453St. Joseph Hospice.(504) 734-0320Serenity Hospice. (504) 366-3996
2011 Annual ReportThe Cancer Program and LaNasa Greco Centerfor Cancer and Blood DisordersTable of ContentsFrom the Chairperson. 2About the Cancer Committee. 4Cancer Committee Members. 5Advances in the Treatment of High Risk Neuroblastoma: A 10-year Review . 6Our Support Services.12Support Services Program Highlight: Caps for Kids.15Did you Know?.16Cancer Conference.17Cancer Statistics.18Analytic Cases.19Cancer Registry.20Histology.21Community Outreach Program and Hematology/Oncology Program. 22Bone Marrow/Hematopoietic Stem Cell Transplant Program.23About the La-Nasa Greco Center forCancer and Blood Disorders.24Treatment Protocols. 30Publications. 34Glossary. 39About Children’s Hosiptal. 401
From the ChairpersonLolie C. Yu, MD,Professor Pediatrics,Cancer Committee Chairman,Pediatric Hematology/Oncologymanagement, research, community outreach andquality improvement. Only 17 percent of cancer programs in the country were given this award.We also received the 2011 Clinical Trial ProgramAward (CTPA) by ASCO for having a high quality clinical cancer research program. Awardees are selectedbased on patient accrual rates, accrual of minorityand underrepresented populations, and innovativetechniques in overcoming barriers to participationin clinical trials. Notably, we were one of only 6 programs in the country who received the award.As the survival rate for pediatric cancer patientsincreased which is now in the range of 80 percent,we are acutely aware that these survivors will requirecontinued monitoring especially for late effects, either from their treatments or from their disease. Tothat end, we recruited Dr. Pinki Prasad.She joined our group in April 2011 and she’s one ofa few pediatric experts in the country who have been2011 was very busy for our Pediatric Hematology-Oncology and Hematopoietic Stem Cell Transplant(HSCT) program, but it was alsovery rewarding. We were recognized by the American Society of Clinical Oncology (ASCO) & AmericanCollege of Surgeons, Commission of Cancer (ACoS,CoC) for providing quality care to cancer patients.We received the 2011 Outstanding AchievementAward (OAA) from the American College of Surgeons,CoC, for having demonstrated a commendation levelof compliance with seven standards that representsix areas of cancer program activity: cancer committee leadership, cancer data management, clinicalCancer Program: A Year of EventsDr. Lolie Yu receiving the CTPA award from Dr. George Sledge (R),President of ASCO and Dr. Robert Comis of the Coalition of CancerCooperative Group. Picture was taken by Todd Buchanan during theASCO 2011 meeting in Chicago.2The second annual CureSearch Walk washeld in April 2011 and deemed a totalsuccess.
trained to provide a comprehensive care for pediatriccancer survivors. Through her efforts, we received a 100,000 Hyundai Hope grant for the developmentof our survivorship clinic. This clinic will provide services to patients who have survived their cancer andthe focus would be to determine if they have developed any late effects. These late effects could be inthe form of cardiac, endocrine, psychosocial or neurocognitive changes. Dr. Prasad together with otherdisciplines, will be part of this program.Last April, we had our second Curesearch Walkand as before, it was a total success. Mayor MitchLandrieu and his lovely wife, Cheryl, were again ourhonorary guests and we are very grateful that theycontinued to support this endeavor. We were ableto raise close to 90,000. All of these monies will beused for research of childhood cancer.I have mentioned only a couple of significantevents that have taken place but as you read thisreport, it will feature all the activities and events thathave occurred in late 2010 to August 2011 with ourPediatric Hematology-Oncology & HSCT programand with our patients.In addition, we have included an article on the advances & significant improvements with the care ofHigh Risk Neuroblastoma patients over the last 10years at Children’s Hospital.We will continue our commitment to provide thebest care for our patients through participation inhigh quality clinical trials through the Children’s Oncology Group and other NCI-sponsored studies. Itmust be noted that for most if not all patients, clinicaltrials provide the best means for accessing a newcancer therapy.Children’s Hospital Cancer Committee members shown with theOutstanding Achievement Award (OAA) presented by the American Collegeof Surgeons, Commission on Cancer a cancer program that provides qualitycare to patients.3
The Cancer Committeespecific outlooks to view the patient as a whole andThe mission of the Cancer Committee is to monitor the care given to children with cancer and imple-offer suggestions and plans to improve care. Childment those ideas that will lead to improvement in thatpsychiatrists, psychologists, social workers, playcare. Since 1989, the Cancer Committee has actedtherapists, non-denominational pastoral workers andunder the aegis of the American College of Surgeons,rehabilitation specialists also bring to the table theirCommission on Cancer (ACoS, CoC), using guidelinesunique outlooks on the support of these children.This past year, we also worked closely with orga-established by them for pediatric cancer centers inthe United States. We remain an approved pediatricnizations such as the American Cancer Society andcancer referral center. We formally became the CenterLeukemia/Lymphoma Society. Such connections havefor Cancer and Blood Disorders in 2002 and have of-helped us to better reach out to the community at largefered, in that capacity, up-to-date treatment protocolsand initiate programs for cancer prevention and educa-and clinical trials which provide patients with the op-tion. They have also helped us better assist families inresettling into the post-Katrina environmentwith its attendant stresses and exigencies.Examples of joint efforts by the Hematology/Oncology Division and these organizations have included lodging of our patientsat the American Cancer Society’s HopeLodge, the provision of a grant that providestransportation vouchers for needy parentsand the Smile Program. The Smile Programis an endeavor which remains dear to ourhearts; it was developed by the AmericanCancer Society, and is designed to enablethe establishment of Big Brother/Sisterlike relationships between our patients,especially those with cancer, and medicalstudents at the Louisiana State UniversityHealth Sciences Center (LSUHSC). Suchrelationships have lasted, at times, beyondportunity to take advantage of the most advanced andthe tenure of the students at the medical schools;current therapies. It also affords them the opportunitylife-long bonds have been forged which sustain ourto learn of new advances as soon as they emerge.children for years afterwards.We also have been able to variably call upon theThe Cancer Committee is comprised of professionals who render care to children with cancer.services of anesthesiology, pharmacy, cardiology, oph-Together, they embody the multidisciplinary conceptthalmology, nursing and laboratory services to ensureof cancer treatment, i.e., taking a unified but com-greater quality control. Nursing staff has provided specialprehensive approach to care or “treating mind, bodyinsight into the problems that sometimes develop on theand soul.” As pediatric hematologists/oncologists,unit. They have been instrumental in carrying out somepediatric neurosurgeons, urologic and orthopaedickey projects on patient satisfaction, infection control andsurgeons, radiation oncologists, pediatric radiologistsanalgesic administration that have allowed us to come upand pathologists, these professionals combine theirwith creative solutions to problems seen in patient care.4
of children with cancer and other blood disorders.The Cancer Committee also oversees clinicalresearch activities, both those associated with ourChildren’s Hospital is closely affiliated with LSUHSChospital and those carried out through our affiliationand is one of its major teaching hospitals, providingwith the Children’s Oncology Group (COG), of whichhigh-quality education to all these individuals. Thewe have been a member institution since 1987. COGenvironment provided by Children’s Hospital has likelyis a national, collaborative pediatric cancer researchinfluenced the career choices of the LSUHSC medi-organization, sponsored by the National Cancercal students who, in high proportion, elect to pursueInstitute at the National Institutes of Health (NCI,a pediatric or med/peds residency. Education, inNIH). Over 90 percent of children who are diagnosedgeneral, remains an essential goal at Children’s Hos-with cancer in the United States, Canada and otherpital, with the Cancer Committee recently incorporat-countries throughout the world are enrolled in proto-ing programs on cancer prevention trials such as thecols for therapeutic, cancer control, epidemiology orFreshStart program, a comprehensive approach to thebiology trials through COG. It is our stance that a highcessation of smoking during pregnancy and after de-percentage of our patients should participate in suchlivery. We are involved in providing information to thetrials in order to advance our knowledge of childhoodfamilies of children in Louisiana through our Web site,cancer and to provide the patients with the latest ad-addressing their concerns about long term environ-vances in treatment and knowledge about the processmental and toxic hazards that might be encounteredof their diseases. It is acknowledged that clinical trialupon their return to New Orleans and its environs.We hope that this annual report of the Children’sparticipation has been associated with improved sur-Hospital Cancer Committee will provide you with infor-vival overall after diagnosis of cancer.mation about the oncology and hematology servicesWe regularly have residents, fellows and otherallied health specialists in attendance at our meetings.available at Children’s Hospital. Further informationThis provides an opportunity to educate them regard-can be obtained by calling the Division of Hematology/ing the interactions and intricacies involved in the careOncology at (504) 896-9740.Cancer Committee MembersLolie C. Yu, MD, Professor ofPediatrics, Cancer CommitteeChairman, Pediatric Hematology/OncologyEvans Valerie, MD, Physician Liason,Pediatric SurgerySimone Bienvenu, RN, QualityAssessment & ImprovementRachel Bufkin, CTR, Cancer RegistrarKay Casey, MSW, Social ServicesDepartmentRandall D. Craver, MD, Pathology/Laboratory DepartmentOfelia Crombet, MD, PediatricHematology/Oncology FellowMatthew Fletcher, MD, PediatricHematology/Oncology FellowCheryl Fourcade, American CancerSocietyRenee V. Gardner, MD, Professor ofPediatrics, Hematology/OncologyCherie Hadley, RN, Pediatric NurseCoordinatorMarie-Louise Haymon, MD,RadiologyCheric Hadle, RN, PediatricHematology/Oncology NurseCoordinatorWendy Huval, RHIA, Director ofMedical RecordsAmy Lee, Child Life SpecialistJaime Morales, MD, AssistantProfessor of Pediatrics, Hematology/OncologyCori A. Morrison, MD, AssistantProfessor of Pediatrics, Hematology/OncologyJennifer Mullinax, MD, Hematology/Oncology FellowPinki Prasad, MD, Assistant ProfessorPediatricsLisa Patterson, RN, Bone MarrowTransplant Nurse CoordinatorMary Perrin, Vice-President, HospitalOperationsMurial Roberts, Clinical TrialsJay Schwab, Pharmacy55Stephanie Sonnier, Clinical TrialsMatthew Starks, MD, Pathology/Laboratory DepartmentRoxanne Stegall, Social ServicesDepartmentMaria C. Velez, MD, AssociateProfessor of Pediatrics, Hematology/OncologyClaudette Vicks, RN, PediatricHematology/Oncology NurseCoordinatorJennifer Walgamotte, MedicalRecords CoordinatorPeggy Williams, LSCW, SocialServices DepartmentLynn Winfield, RN, Nurse ManagerEllen L. Zakris, MD, RadiationOncology
Advances in the Treatment of High-RiskNeuroblastoma: a 10-year ReviewJennifer Mullinax, MDa ; Cruz Velasco, PhDb; Lolie Yu, MDaLouisiana State University Health Science Center and Children’s Hospital, New Orleans aLouisiana State University School of Public Health, New Orleansbcategorized as low, intermediate, and high risk diseasebased on several factors including the stage of disNeuroblastoma is the most common extracranialease, age of the patient, MYCN amplification, histolotumor in childhood and is the third most common magy, and DNA ploidy. Both the stage of the disease andlignancy in childhood overall. It is a cancer of the symrisk category are used to guide therapy. In general, lowpathetic nervous system, and tumors most frequentlyrisk disease includes patients with stage I and II disoriginate from the adrenal glands, but can arise fromease without any unfavorable biologic features (MYCNnerve tissue anywhere along the sympathetic chain.amplication, unfavorable histology, DNA index 1); inNeuroblastoma can exhibit varying degrees of differentermediate risk disease includes patients with stage IIItiation. Undifferentiated neuroblastoma is composeddisease with favorable histology and infants less thanalmost entirely of neuroblasts which histologically ap18 months with stage IV disease; and high risk diseasepear as sheets of small, round, blue cells sometimesincludes patients either Stage IIIor IV and with any of the unfavorable biologic features. Childrenwith low risk disease do very well.Most of these children are curedby surgery alone. Some cases onlyrequire observation with the tumorundergoing spontaneous regression or maturation. Children withlow risk disease have a 98-99%4-year overall survival (2). Childrenwith intermediate risk disease alsodo very well. They are treated witha combination of surgery and chemotherapy and achieve a 3-yearoverall survival rate of 96% (3).Children with high risk disease,however, continue to have pooroutcomes in spite of intense mulFigure 1. Neuroblasts with Homer-Wright pseudorosettes (1).timodality therapies. Until recently,the overall survival rate was apforming Homer-Wright pseudorosettes (see Figure 1).proximately30-40%;however, the use of immunotherIt has the potential to mestastisize to the lymph nodes,apy has increased the 2-year disease-free survival tobone, bone marrow, and skin. There are approximatelyabout 65% and 2-year overall survival to 85% (4).650 new cases of neuroblastoma diagnosed each yearNeuroblastomain the United States, and most children present prior to5 years of age.Outcomes of neuroblastoma are variable and dependent on the extent of the disease. Neuroblastoma isMaterials and MethodsA 10-year retrospective analysis of medical recordsfrom 2001 to 2011 was performed for children diag6
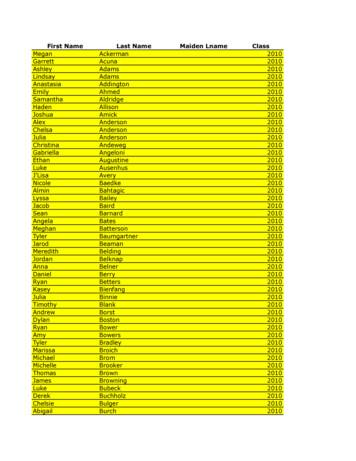
rently undergoing treatment with chemotherapy, norelapses have occurred in this group.Of the eighteen patients with high risk disease,fourteen patients underwent transplant and four patients did not. Of the four patients who did not receivea transplant, one had progressive disease and threerelapsed during induction. Of the fourteen patientswho received a transplant, none experienced relapseor progression of disease prior to transplant. Of thesefourteen patients, six relapsed after transplant andeight did not. Those patients who did not relapse arealive and remain without evidence of disease recurrence. Seven of these eight patients received optimalduration of therapy with isotretinoin and/or other immunotherapy; the eighth patient began treatment withisotretinoin, but had to stop one week into therapydue to side effects. Of the six patients who relapsed,only two tolerated immunotherapy at optimal dosing, one tolerated six cycles of isotretinoin but at areduced dose (secondary to side effects), one beganisotretinoin but had to stop after one week (secondaryto side effects), one relapsed a few weeks after beginning immunotherapy, and one relapsed at 4 months onimmunotherapy. The only patient who remains alive inthis group was one of the two patients who toleratedimmunotherapy at adequate dosing with optimal duration; however, this patient recently relapsed again andcontinues to battle her disease.distribution of neuroblastomaPatients from 2001-2011Low RiskDisease22%High Risk Disease56%Intermediate RiskDisease22%nosed with neuroblastoma at Children’s Hospital ofNew Orleans. Both clinic charts and electronic medicalrecords were reviewed.ResultsFrom October 18, 2001 to October 18, 2011, 35patients were identified as receiving treatment for neuroblastoma at Children’s Hospital of New Orleans. Ofthese 35 patients, 32 medical records were availablefor review. Of the 32 patients whose medical recordswere available, 7 were identified as having low riskdisease (22%), 7 with intermediate risk disease (22%),and 18 with high risk disease (56%).All seven patients with low risk disease underwentsurgical resection only followed by observation. Onepatient relapsed 6 months after diagnosis; this patientsubsequently underwent a second resection and isnow currently receiving salvage therapy with chemotherapy. The other six patients are alive without evidence of disease recurrence at last follow-up.Of the seven patients with intermediate risk disease,five underwent surgical resection and two underwentbiopsy only. All seven patients received chemotherapywith one patient also receiving isotretinoin for prolonged clearance of disease. While one patient is cur-DiscussionOur patient population had a slight female predominance (females 53%, males 47%) and a slightly highermedian age at diagnosis (28.4 months versus 19months) compared to the national data (5) (see Figures2 and 3 below). On the other hand, the age distribution of our patient population is representative of thenational data with 25% of patients presenting priorto one year of age; 84% presenting prior to five yearsof age; and 100% of patients presenting prior to tenyears of age. Over half of our patients presented withhigh risk disease, with about 50% of those experiencing relapse.Our patients with low risk and intermediate riskdisease had very good outcomes. Only one patient ofseven with low risk disease experienced relapse, whilenone of the patients with intermediate disease re7
0Comparison of affected malesand femalesmedian age at diagnosisFigure 2.Figure 2.603050254020301520101050Males0FemalesAge in MonthsNationalChildren’s Hospital30lapsed. Our results are similar to the national data that25surgeryalone (partial or full resection) for low risk disease is sufficient given the overall excellent outcomes20of these patients, while reserving chemotherapy andother salvage treatment only for those who experience15progression or recurrence of disease (2).Given the excellent outcomes of patients with inter10mediate disease, recent studies have evaluated theoutcomesof patients with intermediate disease when5treated with reduced chemotherapy. These studies0 shown a 3-year overall survival rate of 96% inhavespite of the reduction of chemotherapy (3). Our patients also had excellent outcomes without progressionor recurrence of disease. Studies by the Children’sOncology Group are currently underway to evaluatefurther reduction of cytotoxic therapy in this group ofpatients.Patients with high risk disease have a worst outcome when compared to those with low or intermediate risk disease. Therefore, a multimodality approachto treating patients with high risk disease is warrantedand includes chemotherapy, surgery, autologous stemcell transplant, radiation, isotretinoin, and immunotherapy. Patients first undergo induction therapy withintensive chemotherapy using a combination of agentsincluding platinum agents, cyclophosphamide, doxoru-bicin, and etoposide. Surgical resection is also part ofinduction therapy and can be done either at diagnosiswhen feasible or after neoadjuvant chemotherapy.In 1999, Dr. Katherine Matthay, et al published results of a study comparing myeloablative therapy withautologous stem cell transplant versus chemotherapyalone as consolidation therapy. Results showed thatpatients who undergo stem cell transplant have improved outcomes attaining a 3-year event free survivalof 34% compared to a 3-year event free survival of22% for patients who received chemotherapy alone(6). Therefore, myeloablative therapy with autologousstem cell transplant has since become the standard ofcare.Neuroblastoma is a radiosensitive tumor. Childrentreated with a combination of chemotherapy and radiation had improved outcomes when compared to treatment with chemotherapy alone (5). Given the long-termside effects as TBI, radiation is now administered onlyto primary and refractory metastases; and since patients with low and intermediate risk disease have superior outcomes without radiation, radiation is currentlyreserved only for the treatment of high risk disease andfor recurrent or refractory disease.The majority of children with high risk neuroblastoma relapse in spite of achieving complete clinical8
remission after transplant. This suggests that chemotherapy-refractory minimal residual disease plays animportant role in recurrence and has led to researchin the use of isotretinoin and immunotherapy aftertransplant as maintenance therapy. Isotretinoin (13-cisretinoic acid) is a derivative of vitamin A which decreases proliferation and induces differentiation in neuroblastoma cells (see Figure 4). Patients who receiveisotretinoin after transplant achieve a 3-year event freesurvival of 46% compared to only 29% for those whoreceive no further therapy (6). Immunotherapy includesch14.18, granulocyte-macrophage colony-stimulatingfactor (GM-CSF), and interleukin-2 (IL-2) which can beused in combination with isotretonoin. Ch14.18 is amonoclonal antibody directed against disialoganglioside GD2 which is uniformly expressed in neuroblastoma cells and has limited expression in normal tissues. GM-CSF and IL-2 augment antibody-dependentcell-mediated cytotoxicity when used in combinationwith ch14.18 (4). Studies evaluating isotretinoin usedin combination with ch14.18, GM-CSF, and IL-2 showimproved outcomes for patients with high risk diseasewhen treated with immunotherapy achieving a 2-yearEFS of 66% (versus 46% without immunotherapy) anda 2-year OS of 86% (versus 75% without immunotherapy) (4).vascularization and thus leads to cell death. Zactima,or vandetinib, is another investigational drug; it is atyrosine kinase inhibitor which works by preventingtumor growth, and it also is an inhibitor of vascular endothelia
ASCO 2011 meeting in Chicago. The second annual CureSearch Walk was held in April 2011 and deemed a total success. Lolie C. Yu, MD, Professor Pediatrics, Cancer Committee Chairman, Pediatric Hematology/Oncology 2011 was very busy for our Pediat-ric Hematology-Oncology and He-matopoietic Stem Cell Transplant (HSCT) program, but it was also
Ashley Harris 2010 Blake Hartsook 2010 Denira Hasanovic 2010 Ella Heinicke 2010 Amber Heller 2010 . Ryan Coulson 2011 Dellanie Couture 2011 Emily Coy 2011 Allison Crist 2011 Kerrigan Crotts 2011 . Alexandra Hawks 2011 Trevor Heglin 2011 Marisa Heisterkamp 2011 Brett Heitkamp 2011 Caleb Helscher 2011
THIRD-PARTY FUNDRAISING TOOLKIT 200 Henry Clay Avenue New Orleans, LA (504) 896-9375 www.chnola.org CHILDRN 'S HOSPITAL CHILDRN 'S HOSPITAL. HIDRSDTHIRD PARTY TIT 17-58759 THIRD-PARTY FUNDRAISING TOOLKIT Welcome Thank you for your sincere interest in helping Children's Hospital. Please know that your support means the world to
Annual Report 2020 compared to our 2019 Annual Report. The total carbon footprint for printing CIMB Annual Report 2020 was 11,588kgCO2e, compared to 14,987kgCO2e for our 2019 annual report. The carbon footprint for the 3 books of CIMB Annual Report 2020 is 14.485kgCO2e. We are committed to reducing the environmental impact of our annual report .
2011 ktm 690 smc service repair manual 2011 ktm 250 sx-f,xc-f service repair manual 2011 ktm 65 sx service repair manual 2011 ktm 50 sx, sx mini service repair manual 2011 ktm 400/450/530 , service repair manual 2011 ktm 125 duke, service repair manual 2011 ktm 1190 rc8 r, service repair manual 2011 ktm 450 sx-f service repair manual
Rev. Proc. 2011-47,2011-42 IRB 520 - IRC Sec(s). 274, 09/30/2011 Revenue Procedures Rev. Proc. 2011-47, 2011-42 IRB 520, 09/30/2011, IRC Sec(s). 274 High-low per diem method for lodging meal and incidental expenses. Headnote: IRS hasupdated earlier guidance thatallows amount ofordinary and necessary business expenses of
and Meeting Schedules: 6: Annual Report Workgroup Next Steps: Next steps for FY18 report development: 1. HITAC full committee reviews report . FY18 Annual Report Draft discussed: March 1, 2019. FY18 Annual Report Draft discussed: Winter/Spring 2019. FY18 Annual Report completed as needed:
Annual Report Award 2011. [Lot.2] Sebanyak 200 perusahaan mengikuti ajang Annual Report Award 2011. Sebanyak 30 perusahaan ditetapkan sebagai pemenang berdasarkan 10 kategori penilaian. cara Annual Report Award 2011 (ARA 2011) telah digelar pada 18 September lalu. Sebanyak 30 perusahaan dari 10 kategori
Tulang Penyusun Sendi Siku .41 2. Tulang Penyusun Sendi Pergelangan Tangan .47 DAFTAR PUSTAKA . Anatomi dan Biomekanika Sendi dan Pergelangan Tangan 6 Al-Muqsith Ligamentum annularis membentuk cincin yang mengelilingi caput radii, melekat pada bagian tepi anterior dan posterior insicura radialis pada ulna. Bagian dari kondensasi annular pada caput radii disebut dengan “annular band .