Paul P. Drake, Esq. Grossman, Furlow, & Bayó, LLC
Paul P. Drake, Esq. Grossman, Furlow, & Bayó, LLC p.drake@gfblawfirm.com (850) 385-1314
Paul P. Drake, J.D.* In private practice representing health care professionals and regulated entities in Florida licensing and regulatory matters. Mr. Drake does not represent the Department of Health or any regulatory board and he is not providing legal advice in this presentation. *Mr. Drake disclosed no financial relationships to commercial interests whose products or services are directly related to the subject matter of this presentation.
Organization Licensees Department of Health Boards Laws and Rules
GOVERNOR Surgeon General/Secretary Department of Health Health Care Boards and Practitioner Regulation Secretary Agency for Health Care Administration Medicaid Facility Regulation
Total Licensees (as of 2018): MD: 83,394 DO: 9,988 PA: 9,371 AA: 356 O/SUR: 555 PMC: 259 New Categories of Licensure Medical Expert Witness 1,919 Osteopathic Expert Witness 1,604
Department of Health (DOH) provides the centralized administration of health care regulation for: licensing complaints investigations enforcement public records The decision on whether a physician is licensed or disciplined is determined by the boards.
Practice standards & regulatory limitations and requirements are reflected in laws and rules which are subject to change every year. Most laws impacting your practice are located in the following statutes: Chapter 456, F.S. : framework for licensure & discipline of all health care professions. Chapters 458/459, F.S.: Medicine/Osteopathic Medicine Practice Acts. (M.D., PA, AA) Chapter 465, F.S.: Pharmacy Practice Act Dispensing Practitioners Chapter 893, F.S.: Controlled Substances (PDMP) Chapter 120, F.S.: Administrative Procedures Act Hearings, Rulemaking & Declaratory Statements
Neither boards nor licensees can change laws outside of the legislative process, but laws often authorize regulatory boards to create RULES to implement the new law. Changes to rules may occur several times throughout the year. Practicing physicians, public, state and local medical societies participate in the process in rule making hearings and workshops. Individual physicians may be able to change the impact of a rule on their specific practice through the waiver/variance process.
RULES for all health care professions are found in the Florida Administrative Code (FAC). Rule sections are indexed by subject. Rule sections impacting your practice: Rule 64, F.A.C.: Department of Health Rule 64B8, F.A.C.: M.D. Rule 64B15, F.A.C.: D.O.
Chapter 458, Florida Statutes Chapter 459, Florida Statutes Chapter 456, Florida Statutes Rule Chapters 64B8 and 64B15, Florida Administrative Code
These chapters are the allopathic and osteopathic medical practice acts, which govern the practice of medicine in the State of Florida. Define practices of allopathic and osteopathic medicine. Grant the Boards of Medicine and Osteopathic Medicine the authority to promulgate rules regarding the practice of medicine. Provides common grounds for disciplinary action. Address standards for specific areas of practice.
Each Board is composed of members appointed by the Governor and confirmed by the Senate. Elected to 4 year terms. Headquarters are located in Tallahassee, FL. Websites: http://flboardofmedicine.gov http://flboardofosteopathicmedicine.gov
Attempting to obtain or obtaining a license to practice medicine or osteopathic medicine by knowing misrepresentation. Being convicted or found guilty, regardless of adjudication, of a crime in any jurisdiction which directly relates to the practice of medicine or osteopathic medicine or to the ability to practice medicine or osteopathic medicine. A plea of nolo contendere shall create a rebuttable presumption of guilt to the underlying criminal charges.
Failing to keep legible, as defined by department rule in consultation with the board, medical records that identify the licensed physician or physician extender and supervising physician by name and professional title who is or are responsible for rendering, ordering, supervising, or billing for each diagnostic or treatment procedure and that justify the course of treatment of the patient, including, but not limited to, patient histories; examination results; test results; records of drugs prescribed, dispensed, or administered; and reports of consultations and hospitalizations.
Making deceptive, untrue, or fraudulent representations in or related to the practice of medicine or employing a trick or scheme in the practice of osteopathic medicine.
Having a license or the authority to practice medicine revoked, suspended, or otherwise acted against, including the denial of licensure, by the licensing authority of any jurisdiction, including its agencies or subdivisions. The licensing authority’s acceptance of a physician’s relinquishment of license, stipulation, consent order, or other settlement offered in response to or in anticipation of the filing of administrative charges against the physician shall be construed as action against the physician’s license.
Applies to all “Health Care Practitioners” Grants regulatory authority to the Department of Health (DOH) DOH provides legal, investigative and prosecutorial services to the Boards Issuance of license and examination services Additional grounds for disciplinary action
Being found guilty of filing a false complaint with DOH against a licensee Aiding and abetting unlicensed practice of a health care profession Failing to perform a legal obligation placed upon a licensee (This includes not paying student loans) Failing to report in writing within 30 days after being convicted or entering a nolo plea to a crime Performing or attempting to perform services on the wrong patient, a wrong site procedure, a wrong procedure, or an unauthorized procedure
§456.035: Address of Record §456.036: Active and Inactive Status; Delinquency §456.053: Patient Self-Referral §456.054: Kickbacks Prohibited §456.057 Ownership of Patient Records
Contain all the rules promulgated by the Boards of Medicine and Osteopathic Medicine, including: Grounds for disciplinary proceedings and disciplinary guidelines. Standards for the Use of Controlled Substances for Treatment of Pain or Weight Loss Standards of Practice for Physicians Practicing in Pain Management Clinics Standards for Office Surgery and Surgical Facilities Practice Utilizing Telemedicine Medical Records
Suspension or Permanent Revocation Restriction of Practice Probation (Conditions) Fine up to 10,000 per Count Reprimand or Letter of Concern Corrective Action (Including Refund of Fees) Costs!!!
“Government in the Sunshine” Public hearings/workshops and notices of public agency action. Strict notice provisions. Board committee agendas and meeting materials available on-line in advance of meetings. Board minutes available on-line after the meeting.
Impact of “Government in the Sunshine”: Licensure information is on-line for public to access. Discipline information is on-line for public to access. And it never goes away. Physician profiles are on-line for public to access.
Regulation is complex with changes in laws and rules throughout the year. A Florida physician needs internet skills to protect patients and his or her practice. DOH and Boards cannot send individual letters to each licensee explaining the impact on that licensee’s particular practice each time there is a change. Legislature, DOH and Board websites allow you to track changes to current laws and rules as well as on-going changes.
Accessing Information (Continued) Laws and rules Practitioner Profiles Apply for a license Declaratory statements/Waivers/Variances Renewal/CME Annual Reports
Subscription service Professionals Resource Network (PRN) Registration/Inspection (Office Surgery/PMC) Board/Committee meetings Contact information Forms Helpful links.
INVESTIGATION PROBABLE CAUSE LITIGATION BOARD ACTION APPEAL
INSURANCE CARRIERS MUST HMOs MUST HOSPITALS MUST SOMETIMES, COLLEAGUES MUST PLAINTIFFS MUST PATIENTS MAY COMPETITORS DO
FSMB Consumers Internally Generated Law Enforcement Code 15 Reports (AHCA) Notices of Intent to Initiate Medical Malpractice Litigation Nursing Home Surveys Closed Medical Malpractice Claims Florida Birth Related Neurological Injury Compensation Association (NICA) Hospital Discipline Reports (Peer Review) Self Reports
The Department of Health’s Consumer Services Unit receives and reviews complaints. They determine the priority status of complaints prior to referring the complaint to investigations. The investigation involves interviews with the patient, the physician, witnesses and other involved parties. In most cases it also includes review of patient records.
Standard of Care Impairment Fraud Background Probationer Disruptive Physician Background Screening Sexual Misconduct Compliance
The Disciplinary Process is controlled by Section 456.073, Florida Statutes. The process starts with the filing of a legally sufficient complaint. The department, for the boards under its jurisdiction, shall cause to be investigated any complaint that is filed before it if the complaint is in writing, signed by the complainant, and legally sufficient.
A complaint is legally sufficient if it contains ultimate facts that show that a violation of this chapter, of any of the practice acts relating to the professions regulated by the department, or of any rule adopted by the department or a regulatory board in the department has occurred. In order to determine legal sufficiency, the department may require supporting information or documentation.
The Department must notify you of the investigation. You have a right to submit a written response to the notice of investigation. You have a right to obtain a copy of the investigative file, and to submit a written response to the investigative file.
Upon completion of the investigation and pursuant to a written request by the subject, the department shall provide the subject an opportunity to inspect the investigative file or, at the subject's expense, forward to the subject a copy of the investigative file. The subject may file a written response to the information contained in the investigative file. Such response must be filed within 45 days, unless an extension of time has been granted by the department.
When the investigation is complete and legally sufficient, the Department will prepare and submit to the probable cause panel of the appropriate regulatory board an investigative report. The report shall contain the investigative findings and the recommendations of the department concerning the existence of probable cause. It will also include any expert opinion. The determination as to whether probable cause exists shall be made by majority vote of a probable cause panel of the board, or by the department, as appropriate. All proceedings of the panel are exempt from s. 286.011 until 10 days after probable cause has been found to exist by the panel or until the subject of the investigation waives his or her privilege of confidentiality
The Probable Cause Panel of the Board is provided with a complete investigative report, medical records expert opinions by agency consultants and any other pertinent material. The Panel determines whether the facts as developed indicate that a violation of the Practice Act or a Board Rule did occur. In lieu of a finding of probable cause, the probable cause panel, or the department when there is no board, may issue a letter of guidance to the subject. If the probable cause panel finds that probable cause exists, it shall direct the department to file a formal complaint against the licensee.
Send the case for further expert review. Outright dismissal. Closure with a Letter of Guidance Referred back to Legal for further review or further investigation Administrative Complaint Nolle Prosequi Reconsideration SAMPLE LETTER OF DISMISSAL
ESO/ERO SUBPOENA RECORDS DISCIPLINE INJUNCTIONS UNLICENSED ACTIVITY COMPELLED MENTAL & PHYSICAL EXAMINATIONS
Formal Hearing before an Administrative Law Judge. Facts in dispute. Eventually, the ALJ will prepare a Recommended Order to the Board for Final Action. Informal Hearing before the Board. You admit the facts and argue the law, or offer mitigating circumstances Settlement Stipulation Do nothing (Default)
Formal hearings are referred to the Division of Administrative Hearings for resolution. This process typically includes discovery, motions and formal depositions of each party’s expert witnesses. Approximately 85% of disciplinary cases are resolved by consent agreement or informal hearing before the Board without proceeding to formal hearing.
Minor fee disagreements and poor customer service are not considered professional misconduct. The Grounds for Discipline (Violations) for Florida physicians are located in Chapter 458 or 459 and Chapter 456, Florida Statutes as well as the appropriate administrative rules of the Boards of Medicine found in the Florida Administrative Code. (Rule 64B8 and 64B15, F.A.C.)
Disciplinary Penalties are determined by the Board after all due process is concluded. Penalties may include: Revocation or Denial of Licensure Suspension or Restriction of Practice Probation Administrative Fines (Up to 10,000 per count) Continuing Education Courses
Issuance of a Reprimand or Letter of Concern Corrective Action Refunds of Fees Remedial Education Only after patient is compensated or public protected may rehabilitation be provided Assessment of Costs for Investigation and Prosecution
Florida law prohibits the Boards and the Department of Health from issuing a license to or renewing the license of a health care practitioner who has been convicted of or has entered a plea of nolo contendere to a felony violation under chapters 409, 817, 893, federal drug or Medicare fraud laws or a similar felony offense in another jurisdiction, for a period of 5 to 15 years following completion of the criminal sentence, including any probation. Being terminated for cause from Florida Medicaid bars licensure or renewal until 5 years after a return to good standing Being on the OIG Exclusion list is also a bar to licensure or renewal.
Profile Updates Continuing Professional Education Financial Responsibility NICA Reports of Sexual Misconduct Legible Prescriptions Reports of Abuse Failing to Supervise
Report actions in other jurisdictions Advertising as a Specialist Providing Information About Patients’ Rights Failing to Report Colleagues Failing to provide itemized patient bill Maintain mailing address in Board records Notice requirements for closing or relocating practice License renewal
The appropriate board, with those members, if any, who were on the Probable Cause Panel being excused, shall determine and issue the Final Order in each disciplinary case. Such order shall constitute final agency action. Any Settlement Agreement shall be subject to the approval of the Department.
HOW TO ACCESS: Summaries of law changes by year at: on/newest-legislation/index.html Summaries of rule changes and rule text at Board websites. Bill and statute text at www.leg.state.fl.us
Office Surgery Standards The Allopathic Board has amended its Office Surgery Rule, 64B8-9.009, F.A.C., to require EKGs for certain Level III office surgery patients. The new rule became effective on September 4, 2017. The Osteopathic Board also requires EKGs for certain Level III office surgery patients. This is found in Rule 64B15-14.007, F.A.C. Disciplinary Guidelines The allopathic board is in the process of creating a new level of supervision and now has indirect supervision (within 20 miles), direct supervision (on the premises) and immediate supervision (in the same room). All supervisors are required to be board certified. (64B8-8.0011(7), F.A.C.) The osteopathic board has completed a new rule prohibiting a licensee who has had his or her prescribing authority restricted from delegating prescribing authority to an APRN (new term) or to a PA. (64B1519.005(5), F.A.C.)
Record Keeping Effective March 8, 2018, Osteopathic physicians must meet new requirements for minimum content of medical records. Records must be in English, with sufficient detail to demonstrate why a particular course of treatment was undertaken, information must be sufficient to identify the patient, support the diagnosis, justify treatment and document the course and results of treatment accurately. Copies of any records or reports or other documentation requested, obtained and relied upon, from other health care practitioners must be included in the record. All entries made in medical records must be accurately dated and timed. (Office records only need to be dated.) Late entries are permitted, but must be identified as late entries and accurately dated and timed. (Not sure if time requirement for late entries applies to office records.) (64B15-15.004, F.A.C.)
Standard of Care for Office Surgery The allopathic board of medicine is currently working on a proposed rule change to the Office Surgery Rules that will require a surgeon who is unavailable to provide postoperative care to notify the patient of such lack of availability prior to performing an office surgical procedure. In addition, for any Level II, IIA, or III procedures, the surgeon must provide the patient, in writing and prior to the procedure, the name and location of the hospital where the surgeon has privileges to perform the same procedure or the name and location of the hospital where the surgeon or the facility has a transfer agreement.(64B8-9.009(2), F.A.C.) Advertising The allopathic board of medicine has added the American Board of Electrodiagnostic Medicine to the list of approved specialty boards recognized for the purposes of physician advertising. (64B8-11.001, F.A.C., effective February 26, 2018)
1. HB 21 (2018) addressing the prescribing of controlled substances was passed and signed into law with a general effective date of July 1, 2018. This bill amends §456.44, F.S. by expanding the required use of the Prescription Drug Monitoring Program (PDMP), increasing regulation on prescribers and dispensers, and amending criminal laws. The new law changes what are currently statutory standards for controlled substance prescribing (§456.44(3), F.S.) into standards for the prescribing of controlled substances for the treatment of chronic nonmalignant pain and creates standards of practice for treatment of acute pain (§456.44(4) & (5), F.S.).
The prescription of a Schedule II opioid for the treatment of acute pain will now be limited to a 3-day supply, but may be extended to a 7-day supply if deemed medically necessary by the prescriber. However, in such cases, the prescription must contain the words “ACUTE PAIN EXCEPTION” and the prescriber must document in the patient record the acute medical condition and lack of alternative treatment options that justify exceeding the 3-day limit. A prescription for a Schedule II opioid for the treatment of pain other than acute pain must contain the words “NONACUTE PAIN” and the 3 or 7 day limit will not apply.
The new law creates in §456.44(1)(a), F.S., a definition of the term “acute pain” to mean the normal, predicted, physiological, and time-limited response to an adverse chemical, thermal, or mechanical stimulus associated with surgery, trauma, or acute illness. This definition specifically does not include pain related to cancer, a terminal condition, palliative care or a traumatic injury with an Injury Severity Score of 9 or higher.* The new law also requires every person authorized by the DEA to prescribe controlled substances to complete a board-approved 2-hour continuing education course on prescribing controlled substances. The course must be completed by current DEA registrants by January 31, 2019 and at each subsequent renewal of licensure. At this point, the Boards of Medicine and Osteopathic Medicine have each approved course being prepared by the Florida Medical Association, the Florida Academy of Family Physicians and the Florida College of Emergency Physicians.** The new law also authorizes the Board of Medicine to adopt rules establishing guidelines for prescribing controlled substances for acute pain and creates a disciplinary violation for violating the guidelines established by rule. The boards are just starting the rulemaking process.
The new law also significantly amends the provisions of §893.055, F.S., dealing with the Prescription Drug Monitoring Program. Prescribers and dispensers, or their designees, are required to consult the PDMP before prescribing or dispensing a controlled substance for a patient who is 16 years-old or older. This requirement applies regardless of the purpose for the prescription, but does not apply to non-opioid Schedule V controlled substances. There is an exception for when the system is not functional or for when the practitioner is having technical difficulties. The reason must be documented in the patient’s record and the practitioner is limited to prescribing or dispensing no more than a 3-day supply of the controlled substance. A first time failure to consult the PDMP as required will receive a non-disciplinary citation, but any additional violation(s) will be subject to discipline. A dispenser’s willful and knowing failure to report to the PDMP is punishable as a misdemeanor!
Registration requirements for pain management clinics are also changed by the new law. Clinics that were not required to be registered as Pain Management Clinics because they met one of the exemptions set forth in §458.3265, F.S. or §459.0137, F.S., are still exempt from registration, but as of January 1, 2019, they must apply for and obtain a “Certificate of Exemption” from the Department of Health. The certificates must be renewed biennially and must be displayed prominently. If the clinic ceases to meet one of the exemptions, it is required to notify the Department of Health within 3 days and register or cease operations. Certificates are not transferable and a new certificate must be obtained if the clinic relocates or if the clinic’s claimed exemption changes.
If you are registered as a dispensing practitioner pursuant to §465.0276, F.S., the exception to the general prohibition against dispensing Schedule II or III controlled substances, which allows dispensing in connection with the performance of a surgical procedure, has been limited. A Schedule II opioid for acute pain is limited to a 3 or 7 day supply in compliance with §456.44(5)(a), F.S. A Schedule II for non-acute pain must be so identified on the Rx as set forth in §456.44(5)(b), F.S. (“NON ACUTE PAIN”) For traumatic injury with ISS of 9 or higher, must also prescribe emergency opioid antagonist. A Schedule III dispensed must not exceed a 14-day supply.
SB 182 (2019) addressing the medical use of marijuana was passed and was signed into law with a general effective date of March 18, 2019. This bill amends §381.986, F.S. by, among other things, redefining the term “medical use” to include the possession, use, or administration of marijuana in a form for smoking. The bill also requires a qualified physician to submit specified documentation to the Board of Medicine and the Board of Osteopathic Medicine upon determination that smoking is an appropriate route of administration for a qualified patient.
HB 23 (2019) addressing telehealth was passed and signed into law. This bill amends §456.47, F.S. by, among other things, defining “telehealth” and “telehealth provider,” authorizing telehealth providers to use telehealth to perform patient evaluations, and authorizing certain telehealth providers to use telehealth to prescribe certain controlled substances under very specified circumstances. (Signed June 25, 2019/Effective July 1, 2019) New provision §456.47(2)(b), F.S.: “A telehealth provider may use telehealth to perform a patient evaluation. If a telehealth provider conducts a patient evaluation sufficient to diagnose and treat the patient, the telehealth provider is not required to research a patient's medical history or conduct a physical examination of the patient before using telehealth to provide health care services to the patient.”
SB 732 (2019) addressing Office Surgery was passed and signed into law. This bill amends portions of chapters §456, 458, and 459, F.S. (Signed June 25, 2019/Effective January 1, 2020) DOH must now issue an emergency order upon finding that a physician is not meeting practice standards set by boards and such noncompliance creates a danger to the public. Office facilities where liposuction involving removal of more than 1000cc of supernatant fat, Level I, or Level II surgeries are performed, must register unless licensed pursuant to chapter 390 or 395, F.S.
SB 732 (2019) (cont.) By January 1, 2020, each registered office must identify a designated physician responsible for office’s compliance with office health and safety requirements of statute and rules. Designated physician must have full, active, and unencumbered license and practice at the office. DOH shall inspect annually, and the inspections may be unannounced (except physician owned pain clinics holding pain clinic registration exemptions.) Pursuant to current Board rules, inspections must be announced. DOH may suspend or revoke registration for failure of any of its physicians, owners, or operators to comply with statute or rules.
HB 831(2019) addressing Electronic Prescribing was passed and signed into law. This bill amends portions of §456.42 and 456.43, F.S., requiring health care practitioners to electronically generate and transmit prescriptions for medicinal drugs upon license renewal or by July 1, 2021. (Signed June 18, 2019/Effective January 1, 2020)
(a) Has been convicted of, or entered a plea of guilty or nolo contendere to, regardless of adjudication, a felony under chapter 409, chapter 817, or chapter 893, or a similar felony offense committed in another state or jurisdiction, unless the candidate or applicant has successfully completed a pretrial diversion or drug court program for that felony and provides proof that the plea has been withdrawn or the charges have been dismissed. Any such conviction or plea shall exclude the applicant or candidate from licensure, examination, certification, or registration unless the sentence and any subsequent period of probation for such conviction or plea ended: For felonies of the first or second degree, more than 15 years before the date of application. For felonies of the third degree, more than 10 years before the date of application, except for felonies of the third degree under s. 893.13(6)(a). For felonies of the third degree under s. 893.13(6)(a), more than 5 years before the date of application; (b) Has been convicted of, or entered a plea of guilty or nolo contendere to, regardless of adjudication, a felony under 21 U.S.C. ss. 801-970, or 42 U.S.C. ss. 1395-1396, unless the sentence and any subsequent period of probation for such conviction or plea ended more than 15 years before the date of the application; (c) Has been terminated for cause from the Florida Medicaid program pursuant to s. 409.913, unless the candidate or applicant has been in good standing with the Florida Medicaid program for the most recent 5 years; (d) Has been terminated for cause, pursuant to the appeals procedures established by the state, from any other state Medicaid program, unless the candidate or applicant has been in good standing with a state Medicaid program for the most recent 5 years and the termination occurred at least 20 years before the date of the application; or (e) Is currently listed on the United States Department of Health and Human Services Office of Inspector General’s List of Excluded Individuals and Entities. This subsection does not apply to an applicant for licensure or renewal of licensure, certification, or registration who was arrested or charged with a felony specified in paragraph (a) or paragraph (b) before July 1, 2009.
Medical Records of Deceased Physician; Retention; Time Limitations Handling of Patient Records Upon Termination of Practice Patient Records; Costs of Reproduction; Timely Release Written Records; Minimum Content; Retention Maintenance/Ownership of Patient Records
Written records shall contain, at a minimum, the following information about the patient: Patient histories; Examination results; Test results; Records of drugs prescribed, dispensed or administered; Reports of consultations; and Reports of hospitalizations.
Purposes for keeping complete and accurate medical records: To serve as a basis for planning patient care and for continuity in the evaluation of the patient’s condition and treatment. To furnish documentary evidence of the course of the patient’s medical evaluation, treatment, and change in condition. To document communication between the practitioner responsible for the patient and any other health care professional who contributes to the patient’s care. To assist in protecting the legal interest of the patient, the hospital, and the practitioner responsible for the patient.
Both Boards have adopted rules in order
Paul P. Drake, Esq. Grossman, Furlow, & Bayó, LLC. p.drake@gfblawfirm.com (850) 385-1314 . Paul P. Drake, J.D.* In private practice representing health care professionals and regulated entities in Florida licensing and regulatory matters. Mr. Drake does not represent the Department of Health or any
Hon. Jean Hoefer Toal Hon. Daniel Pieper Hon. Kristi Harrington Julie Armstrong Don Michele Stinson Woodward Ferguson Joe Brockington, Esq. Sam Clawson, Esq. Paul Gibson, Esq. Matt Story, Esq. NEVADA Christopher Beecroft Hon. Timothy Williams Steven D. Grierson William Turner, Esq. James Armstrong, Esq. NEW YORK Hon. Douglas McKeon Hon. Barry .
corvel corporation daniel schwartz esq 1:30pm 2105986 hedrick, marchelle r erica tosh esq state bar of nevada dismissed the hartford alyssa m fischer esq 1:30pm 2105056 lide, tracy erica tosh esq mason dixon intermodal dismissed benchmark administrators matthew smith esq 2:00pm 2104580 rosas, jason erica tosh esq pc metro bottling co
SMITH EIBELER, LLC Christopher J. Eibeler, Esq. ID# 031772004 Kathryn K. McClure, Esq. ID# 037462004 Robert W. Smith, Esq. ID# 044341987 Meghan Chrisner-Keefe, Esq. ID# 21052011 Lisa Ackerly Hernandez, Esq. ID# 018402005 David J. Franzmathes ID # 309432019 101 Crawfords C
Manning Curtis Bradshaw & Bednar Dianna Cannon, Esq. Cannon Disability Law Patricia Christensen, Esq. Parr Brown Gee & Loveless Kate Conyers, Esq. Salt Lake Legal Defenders Tammy Georgelas, Esq., Co-Chair Parsons Behle & Latimer Tara Isaacson, Esq. Bugden & Isaacson, LLC Katherine Judd, Esq.
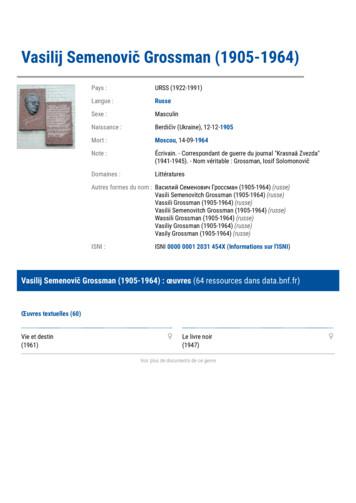
Documents sur Vasilij Semenovič Grossman (1905-1964) (20 ressources dans data.bnf.fr) Livres (17) Perekrestok versij (2017) Vasilij Grossman (2016) Vasilij Grossman v zerkale literaturnyh intrig (2016) Al fondo del nulla, il soffio della vita (2014)
Drake Tax’s program is available for download through the Drake Software Support website (Support.DrakeSoftware.com Downloads Drake Tax) and via CD (avail-able at an extra cost). All federal packages (1040, 1120, 1120S, 1065, 1041, 990, 706, and 709), Drake Documents, p
R8000 45 MHz, 50 kHz Drake R4245 4805 kHz, 5645 kHz, 50 kHz Drake R8B 45 MHz, 50 kHz Drake R8A 45 MHz, 50 kHz Drake R8 45 MHz, 50 kHz Drake
AutoCAD has a very versatile user interface that allows you to control the program in several different ways. At the top of the window is a row of menus. Clicking on the Home, Insert, or Annotate causes another selection of menus to appear. This new selection of commands is frequently called a Ribbon or a Dashboard. You can operate the program by clicking on the icons in these menus. Another .