Decreased Partial Pressure Of Oxygen Hypoxemia
HypoxemiaTroy Schaffernocker, MDHypoxemic Respiratory FailureDecreased PartialPressure of Oxygen Occurs at altitude Barometric pressure and altitude have addramaticti effectff t on oxygen tensionti Oxygen tension of inspired air:9 Sea level 150 mm Hg9 Denver 130 mm Hg9 Mt. Everest 43 mm HgEffect of Barometric Pressure andAltitude on Oxygen Mechanisms of hypoxemia:9 Decreased partial pressure of oxygen9 Impaired diffusion9 Ventilation/perfusion mismatch9 Shunt9 Hypoventilation1
Impaired Diffusion Interstitial lung disease9 Thickened interstitium impedes diffusion of oxygenfrom the alveolus to the capillary EarlEarly in cocourserse of ILDILD, hhypoxemiapo emia usuallys all notsignificant except during states of increasedoxygen demand (exercise) Combination of impaired diffusion and increasedtransit time of blood through alveolar capillaries(due to increased cardiac output from exercise)results in hypoxemiaVentilation/Perfusion The adequacy of gas exchange in the lungsis determined by the balance betweenpulmonary ventilation and capillary bloodflow. Expressed as the ventilation-perfusion(V/Q) ratio.Clinical Situation of Low V/Q(Shunt) V/Q 0 is represented by true right to leftshunting (intracardiac defect) with venousadmixture of blood.9 Alveoli completely bypassed Any situation where alveoli are filled (notventilated):9 Blood, pus, water9 Alveolar hemorrhage, pneumonia, CHF, ARDS Atelectasis of lungClinical Situations of High V/Q(Increase Deadspace) Pulmonary embolism PhysiologicPh i l i ddeadd space as seen iin COPD9 Normal response is to increase minuteventilation2
Hypoventilation Results in hypoxemia that is alwaysassociated with hypercapnia (by definition) Normal physiologic response to PaCO2 isto increase minute ventilation and thusalveolar ventilationNormal Arterial Blood 4-47344734-4734-4734-4734-47A – a PO2(mm Hg)4-177-2110-24102414-2717-3121-3425-38All values related to FIO2 21% at sea levelAdapted from Intermountain Thoracic SocietyManual, 1984 44-45Hypoxemia:Diagnosis and Monitoring Arterial Blood Gas (ABG)AlAlveolarl OxygenOTensionTiAlveolar-arterial (A-a) Oxygen GradientOxygen Content and DeliveryPulse OximetryVariation in ABGsVariationPaO2(mm Hg)PaCo2(mmHg)Mean132.595 Percentileth /- 18 /- 4Range2 – 370 - 12Represents variation over a 1-hour period in 26clinically stable ventilator dependent patientsFrom Hess D, Agarwal NN. J Clin Monitor 19923
Alveolar Oxygen Tension(A-a) Gradient Determined by the alveolar gas equation: (Barometric pressure – H2O vaporpressure)FiOp)py2 – PaCO2/Respiratoryquotient9 (BP – WVP)FiO2 – PaCO2/0.8 (760 – 47)0.21 – 40/0.8 150 – 50 100 mm Hg Normal if hypoxemia is due tohypoventilation (e.g. narcotic overdose) orlow atmospheric O2 (e.g. high altitude).(A-a) Gradient Partial pressure of oxygen in the alveolusminus partial pressure of oxygen in an artery.9 [FIO2 * (Barometric pressure - water vapor) (1 25*PCO2)] - PaO2(1.25*PCO2)] At Room Air9 [150 - (1.2 * PCO2)] - PaO2 A-a Gradient– Normal 8 - 12 mmHg– Increases with age - Age/4 4 High if hypoxemia is due to V/Q mismatch(e.g. Pulmonary Embolus), ImpairedDiffusion (e.g. ILD), or Shunt (e.g. ASD)Oxygen Saturation &Oxygen Delivery Remember oxygen content (CaO2) is amore important management measurethan PaO29 ([Hb] * %Sat * 1.34 ml/g) (PaO2 *0.003) Oxygen delivery the key parameter9 CaO2 * Cardiac output (CO)4
Pulse OximetryNasal Cannula Uses the differential absorbance of light byoxyhemoglobin and deoxyhemoglobin to estimate theoxygen saturation Caveats:1-6 LPM*1L 24%*2L 28%*3L 32%*4L 36%*5L 40%*6L 44%9 Detection of Acute Hypoxemia may be slow9 Does not measure ventilation9 Ambient light9 Electromagnetic Radiation9 Severe Anemia9 Hypoperfusion9 Hypothermia9 Venous Congestion9 Nail PolishAdvantages and Disadvantages ofthe Nasal CannulaOxygen DeliveryDevicesAdvantages: Comfortable Able to communicate Patient can eat andtake oral medications. Easy to use at home.Disadvantages: Nasal obstructionmay impede gasflow. May cause nasalmucosal drying (canbe humidified withsterile water)5
Simple MaskLOW FLOW DeviceNon-Rebreather MaskLOW FLOW Device5-8 LPM* 5-6L 40%15 LPM*6-7L 50%g should remain 1/3-1/2 fullBagafter the patient takes a deepbreath7-8L 60%*7-8L 60% Flow should be set at 5 L/minor more in order to avoidrebreathing exhaled carbondioxide (CO2)Least used mask do tounpredictable FI02 percentage(easier to use Venti Mask)Partial Rebreather Mask15 LPMNO Valvesg should remain 1/3-1/2 full afterBagthe patient takes a deep breathDelivers 60%-80% oxygen Must have all values removedto be considered a PartialRebeather MaskValvesDelivers 90%-100% oxygen Must have all 3 valvesFace TentAdvantages: Designed forpatients with facialtrauma or surgerythat cannot wear aregular mask ornasal cannula.Disadvantages: Clumsy and uncomfortable Variable FIo2 due poor mask seal6
Low-Flow Oxygen DeliveryDeviceNasal CannulaResevoirCapacity(mL)50Simple Face mask150 -250Mask -resevoir bag750 -1250PartialR ebreatherNonrebreatherOxygenFlow(L/min)1Venturi Mask (Venti Mask)ApproximateFIO20.21 -0.2420.24 -0.2830.28 -0.3440.34 -0.380.3850.38 -0.4260.42 -0.465-100.40 -0.605-70.35 -0.755-100.40 -1.03-15 LPM24%-50% (set on base of mask)Set FIo2 with percentagemarkings on the base ofmask and adjust the oxygenflowmeter the the appropriateLPMEstimated based on tidal volume of 500 mL, RR of 20 and I:E of 1:2From Shapiro BA, et al 1991Venturi Mask and Bernoulli’sPrincipleCool Aerosol Mask High Flow Oxygen Delivery with HighParticulate Humidity9 Hydration of airways for tenacioussecretions9 Treatment of Airway Edema9 Accommodate HighLiter Flow of HighFlow Systems Bernoulli’s Principle : Pressure isleast where the velocity of flow isthe greatest. As FI02 and entrained room aircombine and flow through theconstricted opening of the Venturidevice the flow velocity to thepatient increases greatly. By changing the opening size andoxygen flow the FIo2 can be varied.7
HFNCHFNC (High Flow Nasal Cannula) Principle: In the past O2Delivery by nasal routewas limited by the abilityto humidify and warm theinspired gas. Provides adequatelywarmed and humidifiedgas Provides more “washout” of thenasopharyngeald ddeadspace. Greater flow matches thepatient’s naturalinspiratory flow. High flow can be titratedto potentially providepositive distendingpressure for lungrecruitment. CONTRAINDICATIONS9999Unable to protect their airwayInability to adequatelyventilateFacial traumaSignificant epistaxis (Nosebleed) or patients with nasalcomplications COMPLICATIONS/PRECAUTIONS9999Nasal dryness, edema orbleedingDrying mucous, mucousplugging or airwayinflammationSinusitisInappropriate or interruptedoxygen flow may causehypoxemia and orhypercapniaRoca et al Respiratory Care 2010Dewan et al Chest 1994Spence et al Journal of Perinatology 2007O2 DeliveryNon-invasive Ventilation CPAP9 Continuous Positive Airway Pressure BiPAP/Bilevel9 Bilevel Positive Airway Pressure Best Evidence9 COPD Exacerbations9 CHF (Congestive Heart Failure) withPulmonary EdemaWettstein et al Respiratory Care 20058
Non-invasive Ventilation Supportive Evidence9 Facilitation of weaning and extubation inCOPD9 Immunosuppressed Patients9 Extubation Failure in COPD or CHF9 Prevention of Respiratory Failure inAsthma9 PalliativeCPAP vs BiPAP/Bilevel A trial of BiPAP may be worthwhile in patientswho do not tolerate CPAP. This is particularlytrue for patients who seem likely to benefit from alow expiratory pressure:9 patients with discomfort caused by exhaling againstthe CPAP9 patients with mouth leaks despite optimization of theinterface9 and patients with musculoskeletal chest pain due tobreathing at a higher functional residual capacityBiPAP/Bilevel Bilevel positive airway pressure (BiPAP) is amode that delivers an inspiratory positive airwaypressure (IPAP) and expiratory positive airwaypressure (EPAP) The magnitude of the difference between IPAPand EPAP is directly proportional to the amountof tidal volume augmentation and the alveolarventilation. If using a ventilator9 Pressure Support PEEP IPAP9 PEEP EPAPNasal vs Full Face Mask Nasal9 Smaller9 Easy to fit9 CanC hhave significanti ifit leakl k throughthh mouthth Full Face9 Bulkier9 Aspiration Risk9 Claustrophobia9
Non-invasive VentilationHypoxemia Contraindications9 Respiratory Arrest9 Anatomically unable to fit mask9 Inability to protect airway9 Inability to manage secretions9 Inability to cooperate with therapy –poor mental status, agitation, etc9 Aspiration Risk9 Recent upper airway or upper GI surgeryOutpatientUse of supplemental oxygenRuthann Kennedy, RNMechanical Ventilation #1 Indication “If you think about it” Elective intubation is much safer thanemergent intubation Airway control in an unstable patient isbetter for the patient Being on the ventilator does not createventilator dependence – Severe illnesscreates ventilator dependenceIndications for OxygenResting room air saturation 88%PaO2 55 mmHgDesaturation SaO2 88% with exertionDuring sleep: desaturation PaO2 55mmHgor SaO2 88% PaO2 59 mmHg or SaO2 89% in thepresence of cor pulmonale, right heartfailure, hematocrit 55%. Marino ICU book10
Ordering OxygenMedicare Requirements1. Qualification of oxygen need2. Select DMEpp3. Written prescription Flow rate, instructions & length of therapy Example: Oxygen 2L/m with rest, and4L/m with exertion and sleep, length oftherapy -lifetime. Provide home andportable equipment1. Resting, Room Air Saturation 88%2 Desaturation 88% with exertion or sleep2.3. Improved saturation with the addition ofsupplemental oxygenExampleDocumentation requirements The desaturation must be obtained within 2days of hospital discharge or within 30days of outpatient testing Oxygen saturation 88%9 AT REST on room air9 Requires no further testing 56 year old patient with interstitial lungdisease presents with an initial room airSaO2 90%.90% While walking in the hallhall, thesaturation drops to 84%. With the additionof supplemental oxygen at 2 L/m, thesaturation increases to 95%.11
Pulse OximetryOxygen-Hgb Dissocation Curve Standard of care for the assessment ofoxygen saturation “Fifth” vitalit l signi Easily accessible Available from DME for patient useLimitations of Pulse Oximetry Digital injury, especially in conjunction withvasopressors Delay in the detection of acute hypoxemia Does not assess ventilation A significant drop in the PaO2 must occurbefore the saturation decreases (oxygenhemoglobin dissociation curve)Standard OxygenConcentrator Non-portable, compressed air (gas) Oxygen delivery customarily up to 5L/m Special concentrators can deliver 10L/m Requires electricity12
Compact Oxygen ConcentratorE cylinder Compressed air EclipseWeight is approximately18 pounds9 4 hour battery life or AC capable9 Continuous 0.5 – 3.0 L/m9 Pulse 0.5 – 6.0 L/mE tank(Compressed Oxygen) Tank Duration 5.7 hours with flow rate of 2L/mcontinuous. Commonly used in conjunction with wheeledcart “Portable” but not necessarily convenient fortransportation Tank itself weighs 4-5 lbs and is 25 inches tallConserving Device Reservoir Cannulas – Partial rebreatherdevices that store oxygen from exhalation9 Oximizer9 Oximizer Pendant Transtracheal oxygen Pulsed Delivery13
Oximizer Advantage: comfort and easy to use Disadvantage: cosmetic EExtendst d largerlthanth a nasall cannulal andd isiclearly visibleOximizer Pendant Appears like a standard nasal cannula There is a pendant that sits on the upperchestTranstracheal Oxygen Advantages:9 Increased mobility and exercise9 Lower oxygenyg flow requirementsq Disadvantages9 Invasive9 Dislodgement9 Infection14
Transtracheal OxygenLiquid Oxygen LOX –liquid oxygen Reservoir – Home unit9 Weighs 100-160 pounds when filled Portable unit9 Examples: Helios, Escort, Spirit, SprintLOX reservoirs andportablesAdvantages of Liquid Oxygen Reservoir holds 8-10 day supply of oxygenwith continuous flow rate at 2L/m Does not require electricity resulting in anaverage monthly savings of 70. Delivery of high flow – up to 15L/m Portable unit weighs 3.5 lbs with a durationtime of 8 hours at 2L/m15
Inflight OxygenHelios HAHST : High Altitude HypoxiaStimulation Test ABG drawn on 15% oxygen PO2 50 mmHg indicative of need forsupplemental O2 in flightDisadvantages ofLiquid Oxygen Requires hand and arm strength Requires hand eye coordination to fillportable tanks Connections can freeze. The actualtemperature is negative 297 F. Reservoir has to be refilled by DME source16
SmartDose SmartDose Automatically adjusting O2 flow rate incontinuous or pulse dosing. Available for use in conjunction with:9 Compressed O29 Liquid O2Product ComparisonStandard conserverSmartDoseSmartDose Increased WOBDecreased WOBLower dose size & flowrate with activityIncreased dose size &flow rate with activityTiTriggeredd manuallyllAutoAAutot -adjustsdj t beforeb fpttdevelops symptomsLimits activity resulting indecondititioningPromotes activityForces pt to focus on thedevice & diseaseAllows pt to focus on livingNo additional cost17
(due to increased cardiac output from exercise) results in hypoxemia Ventilation/Perfusion The adequacy of gas exchange in the lungs is determined by the balance between pulmonary ventilation and capillary bloodpulmonary ventilation and capillary blood flow. Expressed as the ventilation-perfusion (V/Q) ratio. Clinical Situation of Low V .
What is an Oxygen Concentrator? Oxygen concentrators were introduced in the mid-1970's and have become the most convenient, reliable source of supplemental oxygen available today. Oxygen concentrators are the most cost-effective, efficient, and safest alternative to using high-pressure oxygen cylinders or liquid oxygen.
An oxygen concentrator has been prescribed to provide you with a source for supplemental oxygen. SeQual's Integra E-Z Oxygen Concentrator is an electronically operated oxygen concentrator that separates oxygen from room air. It does not remove oxygen from a room any more than by simply breathing the same room air.
Decreased heart rate Decreased blood pressure Slowed breath rate Decreased need for oxygen Increased blood flow Reduced muscle tension Decreased incidence of headaches and muscle pain Fewer emotional responses such as anger, crying, anxiety, apprehension, and f
78.1 % nitrogen, 21 % oxygen, 0.9% carbon dioxide and noble gases. Any one of these gases, e.g. oxygen, contributes to the total air pressure in exactly these proportions. 1013 hPa x 0.21 213 hPa That is to say, at an air pressure of 1013 hPa, the partial oxygen pressure is 213 hPa. 78.
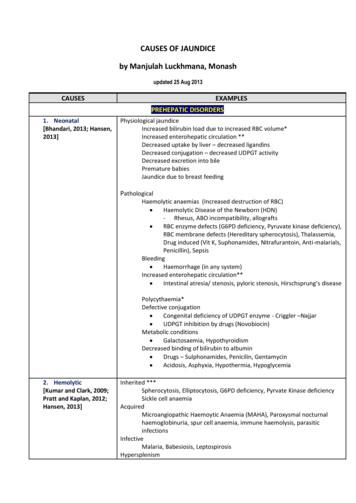
1. Neonatal [Bhandari, 2013; Hansen, 2013] Physiological jaundice Increased bilirubin load due to increased RBC volume* Increased enterohepatic circulation ** Decreased uptake by liver – decreased ligandins Decreased conjugation – decreased UDPGT activity Decreased excretion into bile Premature babies Jaundice due to breast feeding Pathological
the adjusted death rate (Figure 5.1.a) decreased by 29%. The unadjusted death rate for the dialysis population decreased by 27%, while the adjusted death rate decreased by 29%. The unadjusted death rate for the transplant population decreased by 2%, while the adjusted death rate decreased by 40%. Differences between the unadjusted and adjusted
available oxygen in the work area, creating an Oxygen Deficiency Hazard (ODH). There are serious health effects associated with exposure to decreased oxygen concentrations. If oxygen . pressurization of a cryogenic device or associated equipment or systems. Hydrogen is a significant hazard
1 Contents Abbreviations 1. Context and considerations 2. Definitions and intended use 2.1 Oxygen sources devices Oxygen concentrator Oxygen cylinder 2.2 Oxygen delivery devices Nasal oxygen cannula with prongs Mask with reservoir bag Venturi mask 2.3 Devices for oxygen regulat