Insights Into Augmented Repairs Of The Lateral Ankle Ligaments
CentralAnnals of Sports Medicine and ResearchReview ArticleInsights into Augmented Repairsof the Lateral Ankle Ligaments*Corresponding authorShane Hollawell, Department of Orthopedic Surgery,2315 Route 34 S, Manasquan, NJ 08736; Tel: 732-9740404; Fax: 732-449-4271; Email:Submitted: 03 November 2015Accepted: 21 December 2015Published: 23 December 2015Shane Hollawell1* and Catherine Churchill2ISSN: 2379-05711CopyrightDepartment of Orthopedic Surgery, Rutgers University Medical School, USA2Department of Podiatry, Jersey Shore University Medical Center, USA 2015 Hollawell et al.OPEN ACCESSAbstractChronic ankle instability can be a disabling condition requiring surgical correction.The Brostrom procedure is the most common repair technique used for primary repairof the lateral ankle ligaments. Infrequently, this procedure fails and requires revisionalsurgery. Revisional cases necessitate augmentation to strengthen the repair. Highdemand athletes, patients with high Body Mass Indexes, and patients with conditionsassociated with ligamentous laxity may also require augmentation during the primarysurgical procedure. Augmented repair techniques include use of xenografts, allograftrepair techniques, and proprietary kits that use suture anchors, non-absorbable tape,and non-absorbable sutures to repair the ankle construct. Augmentation offers superiorrepair strength beyond the typical construct of a Brostrom repair and is indicated foruse in revisional procedures and in patients with physically demanding lifestyles.ABBREVIATIONSATFL: Anterior Talofibular Ligament; CFL: CalcaneofibularLigamentINTRODUCTIONLateral ankle sprains are among the most common sportsrelated injuries. An estimated 23,000 ankle sprains occur daily[1]. Fortunately, most ankle sprains heal with conservativemeasures including a period of rest, ice, elevation, compression,non-steroidal inflammatory medications, and physical therapy.Orthoses may also be beneficial after ankle sprains, particularlyin the presence of a varus abnormality, in providing neutrallower extremity alignment and in reducing strain on the ankleligaments [2]. Some studies indicate up to 30% of ankle sprains,however, may become chronic with disabling pain and ankleinstability [3].Chronic ankle instability can manifest as a functional ormechanical instability. Functional instability refers to thefeeling of the ankle “giving out” without a true tear of the lateralankle ligaments [4]. Patients with functional ankle instabilitywill complain of difficulty ambulating on uneven surfaces andcommonly describe their ankle as feeling “loose.” These patientswill, however, have normal range of motion of the ankle, andpotentially lack objective evidence of tibiotalar instability. Stressradiographs will be negative for tibiotalar instability. In contrast,in a mechanically unstable ankle, there is a true rupture of thelateral ankle ligaments [5]. Unlike a functionally unstable ankle,a mechanically unstable ankle will be associated with a positiveanterior drawer test and increased range of motion due to a tearor structural abnormality of the ankle ligaments [4,5].Keywords Lateral ankle instability Brostrom procedure Augmented lateral ankle repair Revisional surgeryPrior ankle injury increases the chance of ankle sprainrecurrence, which has been shown to lead to loss of proprioceptionand further weakening the lateral ankle ligaments [6]. Manystudies have demonstrated that ankle injuries can lead to alteredpostural control, defined as the ability of an individual to maintainhis or her center of mass over a single supporting foot [6-8].Rehabilitation protocols focusing on balance and proprioceptionlead to an increase in postural stability [9].After exhausting conservative management, surgical repairof the lateral ankle ligaments may be warranted, especiallyin patients with recurrent sprains and patients who have hadsignificant periods of interrupted activity, or when pain andweakness persist. A large number of surgical procedures havebeen described, and most patients requiring surgery respondwell to primary anatomic repair of the damaged lateral ankleligaments. Some cases require further augmentation andstrengthening of the primary surgical repair and will be the focusof this article.Evaluating chronic ankle instabilityWhen evaluating a patient with chronic ankle instability,a systematic work up should be employed. This includesa careful history and physical examination to preventoverlooking critical related pathologies. A common cause offailure of primary surgical ankle repair is the failure to addressassociated pathologies. Physical examination should evaluate forconcomitant subtalar joint instability and for pathology of theperoneal tendons. Subtalar joint instability can be challengingto diagnose; preoperative diagnostic blocks may prove useful.One should evaluate for possible intra-articular pathology suchas osteochondral defect of the talus or tibia. Chronic injury toCite this article: Hollawell S, Churchill C (2015) Insights into Augmented Repairs of the Lateral Ankle Ligaments. Ann Sports Med Res 2(9): 1054.
Hollawell et al. (2015)Email:Centralthe ankle syndesmosis may also be present. It is essential torecognize a cavus or rear foot varus foot type [10]. A ColemanBlock test will reveal if a lateralizing calcaneal wedge osteotomyis necessary to reduce lateral ankle ligament stress. Additionally,the surgeon must evaluate for a forefoot driven cavus deformitythat may require a dorsiflexory first metatarsal osteotomy [10].In adolescent patients, consider the presence of a tarsal coalitionas a contributing factor to the instability or pain [11]. Familialdisorders associated with hypermobility such as Ehlers-Danlossyndrome and Marfan’s syndrome should be ruled out [12]. Onemust assess the patient’s physical and occupational demands.Athletes, patients with ligamentous laxity, and patients withelevated Body Mass Indexes may require procedures that offeradditional strength to traditional repair techniques.MRI and stress radiographs such as the anterior drawer andthe stress inversion tests will help reveal the condition of thenative ligaments [13]. These imaging studies are particularlyimportant in cases of revisional surgery to provide the surgeonwith information on the quality of the endogenous ligaments andtissue.More than 70 surgical procedures have been described toaddress lateral ankle instability [14]. Surgical options includedirect repair of the lateral ankle ligaments, the use of tendonallografts and autografts, and arthroscopic ligament repair.Surgical repairs can be classified as anatomic or non-anatomicrepairs. Anatomic repairs, such as the one described by Brostrom,use endogenous ligamentous structures to restore the lateralankle ligaments [15]. Non-anatomic repairs use additional tissueto stabilize the lateral ankle ligaments when inadequate nativetissue precludes direct repair.The surgical techniques can be further classified asaugmented or non-augmented repairs. Non-augmented repairsare surgical techniques that use only native tissue for restorationof the lateral ankle ligaments. In contrast, augmented repairsrefer to surgical techniques involving use of tendon allograftsor autografts to strengthen the repair. Multiple techniques havebeen described including peroneus longus, peroneus brevis, andharvested hamstring to reconstruct the lateral ankle complex[16]. In addition to tendon grafting techniques, other forms ofaugmented repair include proprietary kits that contain sutureanchors and suture tape that can be used in conjunction withanatomic repair techniques, such as the Brostrom procedure,to strengthen to the surgical repair. Theoretically, augmentedprocedures offer additional strength and stability to the constructand may be beneficial in patients with physically demandinglifestyles, patients with conditions associated with ligamentouslaxity, and patients with failed primary non-augmented repairs[16].Anatomic RepairsCurrently, the “work-horse” lateral ankle stabilizationprocedure is the Brostrom-Gould procedure. The Brostromprocedure was first described in 1966 and involved repairof ruptures of the anterior talofibular ligament (ATFL) andcalcaneofibular ligament (CFL) [15]. In 1980, Gould modified theprocedure, describing a primary ligament repair strengthenedwith the use of the inferior extensor retinaculum after imbricationAnn Sports Med Res 2(9): 1054 (2015)of the ATFL and CFL [17]. The Brostom-Gould procedure isa popular procedure for anatomic repair of the lateral ankleligaments because it is technically easy to perform and closelyrestores the kinematics of the ankle. Bell et al. found that 91%of patients who underwent the Brostrom-Gould proceduredescribed their ankle function as good or excellent at a mean timeof 26 years [18]. Karlsson et al. reported on 180 Brostrom-Gouldprocedures and reported 89% with good to excellent outcomes[19].The Brostrom-Gould procedure involves a curvilinear orstraight linear incision anterior and inferior to the distal aspectof the fibula. The peroneal tendon sheath is identified and canbe examined for possible injury to the peroneal tendons. TheATFL is identified and examined for attenuation or frank tearing.The ATFL is reflected from its attachment to the fibula. Suturematerial is utilized to repair the ATFL. The CFL is examined andrepaired as necessary in a similar fashion. The inferior extensorretinaculum is mobilized over the ATFL and sutured to theperiosteum of the fibula. Sutures are tied with the foot slightlydorsiflexed and everted. While the Gould modification is used tostrengthen a traditional Brostrom repair, it is not considered aform of augmented repair, as only endogenous nearby tissue isutilized to strengthen the surgical repair.Non-Anatomic Repair ProceduresTypically, non-anatomic repairs involve the sacrifice or splittransfer of the peroneal tendons [20]. A multitude of non-anatomic repair techniques have been described including ChrismanSnook [21], Watson-Jones [22], and Evans [23]. These cases mostcommonly involve splitting the peroneal tendons and routingthem through a drill hole in the fibula. In some cases, the tendonis embedded into the talus and/or calcaneus. These proceduresare indicated for cases of ligamentous laxity and extreme obesity,and are currently reserved for cases of revisional repair. Theserepairs can be technically challenging and may alter subtalar andankle joint motion. Normal anatomy is not replicated, potentiallyleading to stiffness and degeneration by non-anatomical forcesacross the ankle joint [24]. Additionally, these type of repairs areassociated with reduced eversion strength secondary to alteredperoneal tendon function [25]. These type of procedures typically require longer incisions, creating greater incisional concernsand potential for nerve injury.Allograft TechniquesIn recent years, non-anatomic procedures have becomeless routine and have largely been overtaken by newerreconstructive procedures due to the advancements in allograftand augmentation techniques. Allograft techniques are becomingmore popular as they allow augmentation and restoration of thenormal anatomic insertion of ligamentous structures. Unlikenon-anatomic procedures, they do not alter ankle anatomy anddo not sacrifice normal tissues. Allograft techniques have beenshown to lead to good functional outcomes, although with theirown limitations and concerns [25].Various allograft techniques have been reported in theliterature, varying by the graft insertion site, choice of allograft,and anchoring technique [25]. Techniques have been described2/5
Hollawell et al. (2015)Email:Centralutilizing the peroneal tendons, plantaris, gracilis, fascia lata andsemitendinosus tendons [14]. Ellis et al. described a methodinvolving the creation of two bone tunnels in the fibula andutilizing an anterior tibial tendon allograft [25]. All patientsshowed good to excellent activity levels postoperatively [25].Grambart described a procedure involving a peroneus longusallograft secured proximally in the fibula with a bio-tenodesisscrew [26]. Distally, the graft is split longitudinally with theanterior arm of the graft insertedinto the talus and the posteriorarm into the calcaneus [26]. Additional reconstructive techniquesinclude the use of a hamstring allograft or autograft secured intothe talus, fibula, and calcaneus by bio-tenodesis screws [27].Risks associated with allografts include host rejection,avascular tissue implantation, chance of disease transmission, andhigher cost [25]. Need for precise proper physiologic tensioningand “bunching” of the allograft can make these cases technicallydemanding. However, allograft repairs can be appropriatesurgical options in cases of failed prior repair attempts, when thedegree of ligamentous degeneration precludes direct repair, andin cases of hyperlaxity.Arthroscopic Procedures (Arthrobrostrom)Arthroscopy for direct ligament repair has also becomeincreasingly popular in recent years. Ankle arthroscopyis performed on many patients who undergo lateral anklestabilization, in large part due to the mechanism of injury.With lateral ankle injuries, there is a high number of patientswith symptomatic impingements, capsulitis, synovitis, andosteochondral defects of the tibiotalar joint. Arthroscopy allowsfor joint debridement, subchondral drilling of osteochondraldefects, excision of loose bodies, and synovectomy. Afterarthroscopic debridement of the ankle joint, it is typical toperform an open Brostrom-Gould technique using bone anchorsto augment the repair.A proprietary company has developed an all-insidearthroscopic system utilizing a Micro Suture Lasso to performthe Brostrom-Gould procedure. In this technique, known as theArthrobrostrom, suture anchors are placed arthroscopicallythrough the anterolateral arthroscopic portal. Early results,such as those by Cottom and Rigby, have shown a promisingreduction in painful patient symptoms and an earlier return toweight-bearing [28]. At this time, no evidence-based results forarthroscopic lateral ankle repair have been reported for revisionalcases. Rather, arthroscopy of the ankle joint is recommended asan adjunctive procedure with open repair of the lateral ankleligaments in revisional cases.Augmented RepairsManufacturers have developed new technologies to furtheraugment lateral ankle ligament repair. These techniques may beuseful alternatives to surgical techniques using tendon allograftsand autografts. Several proprietary kits are available to provideadditional stability to lateral ankle ligament repair. Thesesystems use Fiber Tape or a similar suture material attached tobone via knotless anchors or swivel locks. Commonly, one anchoris placed in the fibula and one in the talus. Anchors are essentialif there is paucity of the ligamentous structures on the fibularortalar side of the construct. Between manufacturers there areAnn Sports Med Res 2(9): 1054 (2015)minor variations in the insertion sites of the anchors and thenon-absorbable material used, but all share a similar philosophyin that their devices serve to augment anatomic repairs. Therepair can be exceptionally strong; there is a potential risk ofovertightening the ligaments, leading to an overly-rigid repair.Controlled studies are necessary to determine the benefit andlong term results of these systems.Waldrop et al., conducted a study using 24 cadaver specimensdivided into four groups [29]. One group consisted of a controlgroup with intact ATFLs, and in a second group, a traditionalBrostrom was performed. In another group, a Brostromaugmented with a suture anchor in the talus was performed, andin the final group a Brostrom with a suture anchor into the fibulawas performed. Load-to-failure testing was done for each group.No statistically significant difference was found between thethree repair groups in the amount of force required to producefailure of the surgical repair, and all three repair types were muchweaker than the uninjured ATFL group. Suture anchors did notappear to offer superior strength over the traditional Brostromprocedure. This study, however, only evaluated strengthimmediately after the operation. The repair may strengthen overtime as the ligament repair heals. Further studies are necessaryto determine repair strength over time.In contrast to Waldrop’s study, Viens et al. conducted a studyon 18 cadaver limbs [30]. The three study groups consisted ofone group with intact ATFL, one group with suture tape repairof the ATFL, and one group with suture tape augmentation inconjunction to a traditional Brostrom procedure. Unlike Waldrop,Viens found that in the suture tape group, the mean ultimateload-to-failure of suture tape augmentation (315.5 66.8 N) wassignificantly higher than that of the intact ATFL (154.0 63.7 N).Additionally, the mean ultimate load of the Brostrom repair withsuture tape augmentation was not significantly different fromthat of the intact ATFL control group. They concluded that suturetape alone, or in conjunction with a Brostrom repair, offerssuperior strength to the Brostrom repair alone. They theorizedthat suture tape augmentation may be beneficial in cases ofrevisional surgery, in cases of ligamentous laxity, and in obesepatients.Other modifications to augment deficient ligaments includedermal graft products and xenografts. Parks described thesatisfactory results and absence of recurrent instability in thirtyfive lateral ankle stabilization procedures that were performedusing acellular human dermal graft to augment repair [31].Xenografts can additionally be used to strengthen repairsand may be derived from bovine, equine, and porcine sources.Xenografts avoid pitfalls such as the need for a longer incision orissues with the harvesting of an autograft altering the dynamicstability of the foot [16]. Xenografts may offer strength similarto autografts and may be a promising alternative in lateral anklestabilization procedures [32].Augmented repair techniques may be particularly usefulin cases of revisional surgery. Revisional cases after a failedprevious direct repair are particularly challenging. It is criticalto determine the etiology of the initial repair’s failure. An indexof suspicion should be raised for a condition of ligamentouslaxity, a component of hind foot varus, subtalar joint instability,3/5
Hollawell et al. (2015)Email:Centralor recurrent high-grade ankle sprains. Revisional cases canachieve optimal outcomes with specialized augmentation of ananatomical repair. Tissue quality may be poor and the lateral ankleligamentous tissue may deteriorate over time. Simply repeatinga Brostrom-Gould repair without using a supplementary form ofaugmentation can lead to less than optimal outcomes.The precise clinical role of tendon allografts, xenografts,suture anchors, and suture tape in lateral ankle stabilizationsurgery is yet to be determined. Additional strength to theBrostrom repair may be necessary in elite athletes, patientswith high Body Mass Indexes, and in patients with ligamentouslaxity. Further research is necessary before definitive surgicalrecommendations can be made on when to use which type ofaugmentation and which augmentation technique provides thegreatest repair strength.CONCLUSIONMost lateral ankle sprains resolve uneventfully withconservative treatment. In spite of this, some cases requiresurgical repair. The large majority of patients have successfuloutcomes with a primary anatomic repair such as the BrostromGould procedure. Cases of revisional lateral ankle repairare particularly challenging. Success requires a thoroughunderstanding of common surgical pitfalls. It is also essentialto determine why the primary repair failed. The surgeon mustattend to concomitant deformities such as rear foot varus orsubtalar joint stability, and be cognizant of neuromuscular andcollagen disorders. After a failed primary Brostrom-Gould, oneshould choose a procedure that offers further augmentation tothe surgical repair. Athletes, patients with physically demandingoccupations, and patients with high Body Mass Indexes are alsoexcellent candidates for augmented primary repairs with eitherproprietary products using suture anchors and non-absorbablesutures, tendon allografts, or biologic xenografts.Long-term clinical results are not yet available on whichaugmentation method provides the best outcomes, and there areno studies comparing allograft reconstructions with proprietarytechnologies such as suture tape and suture anchors. Despite this,there is a role for augmentation of a primary lateral collateralligament repair in cases of hyperlaxity, patients with physicallydemanding life-styles, and in secondary-type procedures.REFERENCES1. Colville, MR. Reconstruction of the lateral ankle ligaments. J. Bone andJoint Surgery. 1994; 76A: 1092.2. Mattacola CG, Dwyer MK. Rehabilitation of the Ankle after AcuteSprain or Chronic Instability. J Athl Train. 2002; 37: 413-429.3. Lee KT, Young UP, Kim JS, Kim JB, Kim KC, Kang SK. Long-term resultsafter modified Brostrom procedure without calcaneo fibular ligamentreconstruction. Foot and Ankle International. 2011; 32: 153-157.the functionally unstable ankle. Aust J Physiother. 1994; 40: 41-47.7. Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instabilityof the ankle and its value in predicting injury. Med Sci Sports Exerc.1984; 16: 64-66.8. McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictorof ankle injuries in high school basketball players. Clin J Sport Med.2000; 10: 239-244.9. Holmes A, Delahunt E. Treatment of common deficits associated withchronic ankle instability. Sports Med. 2009; 39: 207-224.10. Deben SE, Pomeroy GC. Subtle cavus foot: diagnosis and management.J Am Acad Orthop Surg. 2014; 22: 512-520.11. WähnertD, Grüneweller N, Evers J, Sellmeier AC, Raschke MJ, OchmanS. An unusual cause of ankle pain: fracture of a talocalcaneal coalitionas a differential diagnosis in an acute ankle sprain: a case report andliterature review. BMC Musculoskeletal Disorders. 2013, 14: 111.12. Scheper MC, Engelbert RH, Rameckers AA, Verbunt J, Remvig L, JuulKristensen B. Children with Generalized Joint Hypermobility andMusculoskeletal Complaints: State of the Art on Diagnostics, ClinicalCharacteristics, and Treatment. BioMed Research International. 2013;1-13.13. Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibularligament injury with stress radiography, ultrasonography and MRimaging. Skeletal Radiol. 2010; 39: 41-47.14. Di Giovanni CW, Brodsky A. Current concepts: lateral ankle instability.Foot Ankle Int. 2006; 27: 854-866.15. Broström L. Sprained ankles. V. Treatment and prognosis in recentligament ruptures. Acta Chir Scand. 1966; 132: 537-550.16. Hollawell, SM. An improved lateral ankle stabilization procedure.Podiatry Management. Oct 2008: 137-142.17. Gould N, Seligson D, Gassman J. Early and late repair of lateral ligamentof the ankle. Foot Ankle. 1980; 1: 84-89.18. Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results afterBroström procedure for chronic lateral ankle instability. Am J SportsMed. 2006; 34: 975-978.19. Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of thelateral ligaments of the ankle for chronic lateral instability. J BoneJoint Surg Am. 1988; 70: 581-588.20. Karlsson J1, Bergsten T, Lansinger O, Peterson L. Lateral instabilityof the ankle treated by the Evans procedure. A long-term clinical andradiological follow-up. J Bone Joint Surg Br. 1988; 70: 476-480.21. Chrisman OD, Snook GA. Reconstruction of lateral ligament tearsof the ankle, an experimental study and clinical evaluation of sevenpatients treated by a new modification of the elmslie procedure. JBone Joint Surg Am. 1969; 5: 904-912.22. Watson-Jones R. Recurrent forward dislocation of the ankle joint. JBone Joint Surg Br. 1952; 34-B: 519.23. EVANS DL. Recurrent instability of the ankle; a method of surgicaltreatment. Proc R Soc Med. 1953; 46: 343-344.4. Richie DH Jr. Functional instability of the ankle and the role ofneuromuscular control: a comprehensive review. J Foot Ankle Surg.2001; 40: 240-251.24. Sugimoto K, Takakura Y, Akiyama K, Kamei S, Kitada C, Kumai T.Long-term results of Watson-Jones tenodesis of the ankle. Clinical andradiographic findings after ten to eighteen years of follow-up. J BoneJoint Surg Am. 1998; 80: 1587-1596.6. Ryan L. Mechanical stability, muscle strength and proprioception in26. Grambart S. A closer look at allografts for lateral ankle ligament5. Freeman MA, Dean MR, Hanham IW. The etiology and prevention offunctional instability of the foot. J Bone Joint Surg Br. 1965; 47: 678685.Ann Sports Med Res 2(9): 1054 (2015)25. Ellis SJ, Williams BR, Pavlov H, Deland J. Results of anatomic lateralankle ligament reconstruction with tendon allograft. HSS J. 2011; 7:134-140.4/5
Hollawell et al. (2015)Email:Centralreconstruction. Podiatry Today. 2010; 23:11.27. Jeys LM, Harris NJ. Ankle stabilization with hamstring autograft: a newtechnique using interference screws. Foot Ankle Int. 2003; 24: 677679.28. Cottom JM, Rigby RB. The “all inside” arthroscopic Broströmprocedure: a prospective study of 40 consecutive patients. J FootAnkle Surg. 2013; 52: 568-574.29. Waldrop NE 3rd, Wijdicks CA, Jansson KS, La Prade RF, Clanton TO.Anatomic suture anchor versus the Broström technique for anteriortalofibular ligament repair: a biomechanical comparison. Am J SportsMed. 2012; 40: 2590-2596.30. Viens NA, Wijdicks CA, Campbell KJ, Laprade RF, Clanton TO. Anteriortalofibular ligament ruptures, part 1: biomechanical comparisonof augmented Broström repair techniques with the intact anteriortalofibular ligament. Am J Sports Med. 2014; 42: 405-411.31. Parks RM, Parks SM. Lateral ankle stabilization using acellular humandermal allograft augmentation. J Am Podiatr Med Assoc. 2015; 105;209-217.32. Laurencin CT, El-Amin SF. Xeno transplantation in orthopaedicsurgery. J Am Acad Orthop Surg. 2008; 16: 4-8.Cite this articleHollawell S, Churchill C (2015) Insights into Augmented Repairs of the Lateral Ankle Ligaments. Ann Sports Med Res 2(9): 1054.Ann Sports Med Res 2(9): 1054 (2015)5/5
Surgical repairs can be classified as anatomic or non-anatomic repairs. Anatomic repairs, such as the one described by Brostrom, use endogenous ligamentous structures to restore the lateral ankle ligaments [15]. Non-anatomic repairs use additional tissue to stabilize the lateral ankle ligamen
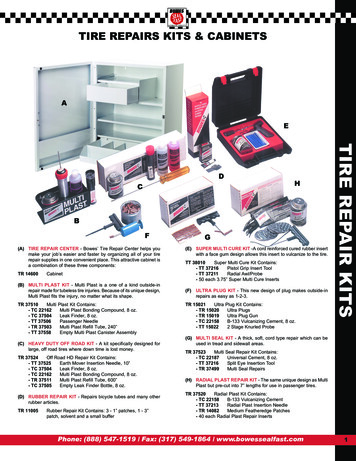
(A) REINFORCED LARGE TIRE BIAS REPAIRS - RT Bias Repairs are extra strong molded permanent repairs for bias ply tires which offer both strength and flexibility. These chemically self vulcanizing repairs are shaped for the best fit making repairs faster and easier and eliminating the need for separ
All other equipment repairs may be charged to Function 8100 (Maintenance of Plant). 0354 Vehicle Repairs/Maintenance 0355 Technology‐Related Repairs and Maintenance (Formerly Computer Repairs) Expenditures for technology‐related repairs and maintenance. 0356 Inspect/Repair Fire Extinguisher
Augmented Reality in Education ISBN: 978-960-473-328-6 . 1 Augmented Reality in Education EDEN - 2011 Open Classroom Conference Augmented Reality in Education Proceedings of the “Science Center To Go” Workshops October 27 - 29, 2011 Ellinogermaniki Agogi, Athens, Greece. 2File Size: 2MB
Augmented Reality for Cars From Wikipedia: Augmented reality (AR) is a live, direct or indirect, view of a physical, real-world environment whose elements are augmented by computer-generated sensory input such as sound, video, graphics or GPS data. HI-CAR: Honda
toward the dominant. The augmented sixth chord is typically preceded by a tonic chord, a subdominant chord, ( )VI, or ( )III; it is almost always followed by V or the cadential chord. Types of Augmented Sixth Chords All augmented sixth chords have three basic components. 1. The bass is a half step above
I think of atomic vectors as “just the data” Atomic vectors are the building blocks for augmented vectors Augmented vectors Augmented vectors are atomic vectors with additional attributes attach
zillman@virtualprivatelibrary.com Augmented Data Discovery Resources 2022 is a comprehensive listing of augmented data discovery resources, sources and sites on the Internet. The below list of sources is taken from my Subject Tracer Information Blog titled Augmented Data Discovery and
Grade 2 ELA Week of April 13-17, 2020 Day Skill Instructions Monday . There was a city park very close to their apartment. The park was really big. Maybe part of it could be turned into a park for dogs. Then Oscar s puppy would have a place to run! 4 Now Oscar needed to turn his idea into a plan. Oscar worked very hard. He wrote letters to newspapers. He wrote to the mayor about his idea for .