CFPC CoI Templates: Slide 1 Used In Faculty Presentation . - WildApricot
CFPC CoI Templates: Slide 1 – used in Faculty presentation only. Faculty/Presenter Disclosure Faculty: Ronald Schondorf Relationships with financial sponsors: Grants/Research Support: Nada Speakers Bureau/Honoraria: Nada Consulting Fees: Nada Patents: Nada
CFPC CoI Templates: Slide 2 Disclosure of Financial Support This program has received financial support from my pocket in the form of time spent preparing. This program has received in-kind support from no one in the form of ? Potential for conflict(s) of interest: Dr Ronald Schondorf has received nothing from anyone
Orthostatic Hypotension Dr. Ronald Schondorf Department of Neurology Jewish General Hospital McGill University
Objectives CanMeds Objectives Learn stuff about OH Real Life Objectives Have fun doing it
Scansorial Snakes Have higher BP (40-70 mmHg) than aquatic snakes (20-30 mmHg) Have more developed autonomic nervous system circuitry Have heart positions that are closer to the head than non-climbing species Have shorter body length, small body girth, tight skin and low compliance of the subcutaneous tissue space.
Solutions to Overcome Hydrostatic Gradient Pump harder at higher pressure (giraffe) Place heart closer to head (tree-climbing snake vs. terrestrial snakes) Auxiliary heart (no evidence as yet) Siphon
TILDA Normative Data to Stand
Tilt Table Testing
Ultimately Hypotension May Be Caused By Impaired adaptive mechanisms Disease related conditions Reflex syncope
Major Aims of Autonomic Clinical Evaluation Determine whether autonomic function is normal or abnormal Localize the site(s) of dysfunction Recognize patterns of autonomic failure Assess the degree of dysautonomia Ascertain whether the abnormality is primary or secondary Prognosticate and treat
Cerebral Symptoms of Postural Hypotension Dizziness Visual disturbance scotoma greying out colour defects Loss of consciousness Impaired cognition Focal neurologic signs
Other Symptoms of Postural Hypotension Muscle hypoperfusion coathanger ache lower backache Cardiac hypoperfusion angina pectoris Orthostatic dyspnea Spinal cord hypoperfusion Renal hypoperfusion “Non-specific” weakness falls
Factors Influencing Orthostatic Hypotension Speed of positional change Standing (waiting in line) Prolonged recumbency Exercise (mild) Meals Heat Time of day Drugs
Response to Stand
Cerebrovascular Response to Stand in Young and Elderly Lipsitz et al. Stroke 2000
Factors Influencing Orthostatic Hypotension Speed of positional change Standing (waiting in line) Prolonged recumbency Exercise (mild) Meals Heat Time of day Drugs
Physiologic Effects Of Prolonged Bedrest Reduced cardiac parasympathetic activity Reduced sympathetic vasomotor activity Increased venous compliance Reduced plasma and blood volume Reduced stroke volume Reduced baroreflex function
Factors Influencing Orthostatic Hypotension Speed of positional change Standing (waiting in line) Prolonged recumbency Exercise (mild) Meals Heat Time of day Drugs
The Most Important Question to Ask For Exercise Related Syncope Did you lose consciousness during exercise or after you stopped? After makes structural heart disease much less likely
Exercise Induced Hypotension In Autonomic Failure Blunting of vasoconstriction in non-exercising beds or splanchnic bed Overperfusion of exercising muscle Reduced cardiac output response to exercise
Exercise Patterns During Autonomic Failure
Factors Influencing Orthostatic Hypotension Speed of positional change Standing (waiting in line) Prolonged recumbency Exercise (mild) Meals Heat Time of day Drugs
Postprandial Hypotension
Factors Influencing Orthostatic Hypotension Speed of positional change Standing (waiting in line) Prolonged recumbency Exercise (mild) Meals Heat Time of day Drugs
Medication-Induced Hypotension Anti-hypertensives Anti-anginals Anti-depressants Diuretics Terazosin Dopaminergic agonists
Symptom Recall in the Elderly 30% of cognitively normal elderly cannot recall a witnessed fall 3 months later Syncope is denied in 50% of elderly with documented carotid sinus hypersensitivity Dizziness and lightheadedness may not be present in the elderly with orthostasis Shaw FE, Kenny RA, Postgrad Med J 1997
Sudomotor Symptoms Heat intolerance Sweating after exertion or following hot bath Exaggerated hyperhydrosis at normal ambient temperature Pattern of hyperhydrosis Pattern of hypohydrosis (check the socks)
Gastrointestinal Gastroparesis (early satiety, bloating, fullness or frequent nausea) Weight loss Constipation Alternating diarrhea and constipation
Urogenital Urinary frequency and urgency Sphincter dyssynergia erratic volitional voiding Neurogenic bladder Erectile dysfunction, ejaculatory failure, retrograde ejaculation
Normal RSA Heart Rate bpm 90 70 50 Blood Pressure mmHg 120 60 0 CO2 mmHg 50 25 0 0 1 2 3 Time (min) 4 5
Normal Valsalva Response BP 150 mmHg Your text 90 30 10.5 11 Time (min) 11.5
Normal Valsalva Response Heart Rate bpm 120 80 40 Blood Pressure mmHg 100 75 50 10 11 Time (min) 12
Sandroni et al J Appl Physiol 1991
Cases
Autonomic Failure
AF Case Presentation 1 53 y.o man ulcerative colitis resistant to steroids requiring colectomy and subsequent re-anastomosis Complicated post op course sepsis, pneumonia, pleural effusions, renal failure Subacute onset of OH, abnormal sweating and erectile dysfunction Worsening AF over next year
53 y.o man autonomic failure Heart Rate bpm 100 55 10 Blood Pressure mmHg 140 70 0 0 1 2 Time (min) 3 4 5
53 y.o man autonomic failure Heart Rate bpm 140 90 40 Your text Blood Pressure mmHg 140 70 0 6 9 Time (min) 12
53 y.o man autonomic failure Heart Rate bpm 100 55 10 Blood Pressure mmHg 200 100 0 0 10 20 Time (min) 30 40
QSART Autonomic Failure Sweat Output Sweat Rate (nanoliters/min) 1000 800 Forearm Proximal Distal Foot Your text 600 400 200 0 8 10 12 Time (min) 14 16 18
AF Case Presentation 2 53 year old right handed man with a 7 year history of progressive dizziness and near syncope. Postural lightheadedness and coathanger headache Whiting out of vision after meals Diminished palmar and plantar sweating Erectile dysfunction for years
AF Case Presentation 2 (2) No symptoms of neuropathy Biochem, CBC, TSH, cortisol, prolactin, SPEP all normal Normal MRI of the brain Normal EEG
AF Case Presentation 2 (3) BP 120/80 mmHg supine, 100/70 mmHg seated, 80/40 mmHg upright within 1 minute of stand Cardioacceleration during hypotension No symptoms with hypotension Dry palms and soles with no compensatory hyperhydrosis
Heart Rate bpm 120 60 0 Blood Pressure 200 mmHg 80 deg 30 deg 45 deg 100 0 Cerebral Blood Velocity cm/sec 100 50 0 0 14 28 42 Time (min) 56 70
Post Prandial Hypotension Heart Rate bpm 120 60 0 Blood Pressure mmHg 200 100 0 0 10 20 40 50 60 Time (min) 70 80 90
Bicycle Exercise Between min 5 and 14 Heart Rate bpm 120 60 0 Blood Pressure mmHg 200 100 00 5 10 Time (min) 15 20 25
MAST Pants Between 11 and 17 Min Heart Rate bpm 120 60 0 Blood Pressure mmHg 200 100 00 5 10 Time (min) 15 20 25
71 y.o. man avid cyclist Episodic lightheadedness with quick stand Exacerbated by meals wine both Flomax
Delayed OH
77 y.o. man PD 2 year history, asymmetric onset R L, festinating gait Sinemet 100/25 5 times daily, Deprenyl Passed out St Patrick’s Day parade 2009 Other episodes of postural lightheadedness
HUT 77 y.o. man PD
RSA and Valsalva 77 y.o. man PD
Severe Diabetic Autonomic Neuropathy 84 year old man with diabetes mellitus lives in a residence. He has had several falls but tends to minimize this. He does not take anti-hypertensive medication but has been found to have orthostatic hypotension. The patient cannot provide any additional history. Physical exam reveals normal power, areflexia, indifferent plantar responses, No Parkinsonian features. Vibration is not perceived at the toes or ankles. Gait is on a widened base. The pull test is negative.
Severe Diabetic Autonomic Neuropathy (2) RSA
Severe Diabetic Autonomic Neuropathy (2) Valsalva
Severe Diabetic Autonomic Neuropathy (2) Head-Up Tilt
Severe Diabetic Autonomic Neuropathy (2) QSART
Another Case of Diabetic Autonomic Neuropathy? 71 year old man who experienced an episode of syncope after running on the treadmill. He was admitted to hospital for a full cardiac workup that was negative. The patient had a similar episode of syncope 4 years ago. Now he finds that he has whiteout of his vision if he walks vigorously. On other occasions he may experience an ache of his neck and shoulders. Three years ago he began to have atrial fibrillation and started dabigatran. He has diabetes mellitus controlled with metformin. Hemoglobin A1C is 6%. Other medications include Lipitor and Viagra for erectile dysfunction. He has occasional constipation. The patient frequently yells or sings in his sleep. On one occasion while he was in a hotel security was called because he was yelling in his sleep in the middle of the night. He has punched the wall, knocked over lamps and even inadvertently struck his wife while sleeping. He has no symptoms of diabetic neuropathy, bladder or laryngeal dysfunction.
Another Case of Diabetic Autonomic Neuropathy? Physical examination reveals orthostatic hypotension. Normal motor examination. No cogwheeling. Normal fine finger movements. Reflexes are normal. Plantars are flexor. Vibration is normal at the toes. Gait and station are normal.
Another Case of Diabetic Autonomic Neuropathy? RSA and Valsalva
Another Case of Diabetic Autonomic Neuropathy? Head-Up Tilt
Another Case of Diabetic Autonomic Neuropathy? QSART
Case of Syncope in Elderly Man 78 year old man with paroxysmal atrial fibrillation and a left parietal stroke was referred in 2002 for evaluation of approximately 5 episodes of transient loss of consciousness that occurred without warning while seated or recumbent. In 1992, prolonged bradycardia was noted during carotid sinus massage. A VVI pacemaker was inserted at that time and subsequently exchanged in 2000 for an A-V pacemaker. During his most recent visits to the emergency room, hypotension was noted during episodes of tachycardia that responded to adenosine.
Medications (1) Metoprolol Omeprazole ASA Simvastatin Warfarin
First Tilt
Case of Syncope in Elderly Man (2) In 2006, he was admitted to the Montreal Heart Institute for recurrent syncope. Tricuspid and mitral insufficiency were noted. Syncope was provoked during Dipyridamole injection. The pacemaker battery and atrial pacing wire were replaced.
Medications (2) Irbesartan Metoprolol Amiodarone Amlodipine Bisoprolol Furosemide Simvastatin Warfarin
Case of Syncope in Elderly Man (3) During review of systems he mentioned feeling light-headed after meals. Physical examination revealed a supine BP of 110/70 mmHg which decreased to 90/70 mmHg upon standing. There was moderate cognitive impairment but the neurological examination was otherwise unremarkable for age.
Second Tilt
Important Take Home Points Diagnoses are often presumptive (CSH) Etiology of syncope may change with time Always pay close attention to medications Look for additional stressors of orthostatic hypotension Hypotension is not always appreciated after short duration stand
Additional Points to Ponder Evaluation of autonomic nervous system function in the elderly is limited if effectors are impaired Did the hypotension contribute to the patient’s cognitive impairment?
General Principles of Treatment Treat symptoms not low blood pressure Watch for supine hypertension Pay attention to volume status Pay attention to disease specific factors Pay attention to side effects of medications
Physical Countermaneuvers Leg cross Toe lift One leg up Bend from the waist Down on one knee Squat Fishing chair
Physical Counter Maneuvers
Treatment of Orthostatic Hypotension Lifestyle management Physical counter-maneuvers Water ingestion Fludrocortisone Midodrine Pyridostigmine Octreotide Erythropoietin L-threo-DOPS
Effects of Chronic Fludrocortisone Administration Reduced angiotensin secretion Increased secretion of atrial natriuretic factor Pressure natriuresis Reduced sympathetic activity Potentiation of the pressor response to norepinephrine Variable increase in plasma volume
Effects of Midodrine Administration Increased blood pressure Increased total peripheral resistance Increased venomotor tone Decreased heart rate Decreased sympathetic activity Decreased plasma volume
Supine Hypertension Associated with increased Cr o reduced GFR o LVH o Intracranial hypertension o
Autonomic Neurosci 2008
Supine Hypertension in Autonomic Failure Is Reduced By Viagra Gamboa et al. Hypertension 2008
Merci Questions?
Dr. Ronald Schondorf Department of Neurology Jewish General Hospital McGill University. Objectives CanMeds Objectives Learn stuff about OH Real Life Objectives Have fun doing it. Scansorial Snakes Have higher BP (40-70 mmHg) than aquatic snakes (20-30 mmHg)
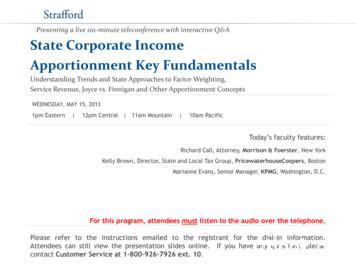
Payroll Factor [Marianne Evans] Specific Industry Apportionment [Kelly Brown] Combined/Consolidated Return Issues [Richard Call] Latest Important Developments Slide 51 [Kelly Brown] Slide 8 - Slide 10 Slide 40 - Slide 44 Slide 45 - Slide 50 Slide 11-Slide 14 Slide 15 - Slide 26 Slide 27 - Slide 33 Slide 34 - Slide 39
San Francisco, California Los Angeles, California Orlando, Florida. Slide 3 What do we do? Slide 4. Slide 5. Slide 6. Slide 7. Slide 8. Slide 9. Slide 10. Slide 11. Slide 12. . IFMA: 2013. What is The Goal. Who or What is Steering the Ship? HIPAA HCAHPS LEED ASHE/FGI Slide 34. Slide 35
Methods: We calculated the cost of illness (COI) every 3 years from 1996 to 2020 using governmental statistics. COI was calculated by summing the direct costs, morbidity costs, and mortality costs. Results: From 1996 to 2011 COI was trending upward. COI in 2011 (697 billion yen) was 1.7-times greater than that in 1996 (407 billion yen).
Southwest Research Institute PI-Institution Don Hassler, PI Project management Electronics Geology, atmosph. transport Astrobiology University of Kiel Lead-CoI Institution Bob Wimmer, Lead-CoI Sensorhead, FEE data analysis Modeling DLR Cologne Calibration, Dosimetry Günther Reitz, Lead-CoI Astronaut Safety Johnson Space Flight Center Astronaut .
Jul 26, 2018 · party Certifier’s name must be on IP. D. Organic Claims. “100% Organic”: all ingredients are Certified Organic ingredients (COI) “Organic”: 95% COI “Made With Organic”: 70-95% COI “Made with organic _
PMO, this COI Model Charter, as it requires, to meet its particular, community's mission needs. The COI Model Charter is a baseline of terms for the governance and management of a COI. Any required changes to the primary terms of this charter, other than the addendum that
LibreOffice uses three terms for one concept: slide master, master slide, and master page. All refer to a slide which is used to create other slides. This book uses the term . See "Working with templates" on page 17 for more information about templates. Figure 1: Sidebar Master Pages section
Tulang-tulang pembentuk rangka tubuh . 12 3. Tulang-tulang di regio manus tampak . Anatomi hewan ini yang dipelajari adalah anatomi tubuh hewan piara. Pelaksanaan perkuliahan dan praktikum anatomi hewan dilakukan setiap minggu sesuai jadwal dengan beban 3 sks (1-2) pada mahasiswa semester 1. Pelaksanaan meliputi tutorial, pretest, praktikum di laboratorium, pembuatan laporan, dan ujian .