A Digital NHS? - King's Fund
BRIEFINGA digital NHS?An introduction to thedigital agenda and plans forimplementationAuthorsMatthew HoneymanPhoebe DunnHelen McKennaSeptember 2016
A digital NHS?Key messages Digital technology has the potential to transform the way patients engage withservices, improve the efficiency and co-ordination of care, and support peopleto manage their health and wellbeing. Previous efforts to digitise health care have resulted in considerable progressbeing made in primary care, while secondary care lags significantly behind. The government and national NHS leaders have set out a high-level visionand goals for digitising the NHS. However, there is a risk that expectationshave been set too high and there has been a lack of clarity about the fundingavailable to support this work. In view of this, we welcome the more realistic deadlines called for in theWachter review. We also welcome the Wachter review’s conclusion that currentfunding would be insufficient to achieve the goals set for 2020. This agenda has been subject to a confusing array of announcements, initiativesand plans. Shifting priorities and slipping timescales pose a risk to credibilityand commitment on the ground. Ministers and national leaders must now set out a definitive plan which clarifiespriorities and sets credible timescales, generates commitment and momentum,and is achievable given the huge financial and operational pressures facingthe NHS. This requires urgent clarification about when funding alreadyannounced will be available and how this can be accessed. Holding backinvestment until the end of the parliament, as appears to be planned, willimpact on the ability of local areas to make significant progress. Progress in this area requires much more focus on engaging and upskilling thepeople (at all levels in the NHS) who are expected to use it. The importance ofengaging clinicians, in particular, and conveying the benefits associated withdigitisation should not be underestimated. Data sharing is essential for conducting research and improving patientcare. The recent Caldicott and Care Quality Commission reviews present anopportunity to address legitimate public concerns about data sharing in theNHS. However, it is also critical that information governance is not a barrierto progress.Key messages 1
A digital NHS?IntroductionThe report by Professor Robert Wachter and the National Advisory Group onHealth Information Technology (2016) is the most recent in a series of reviews andinitiatives seeking to support the NHS’s efforts to digitise. Together with ambitionsset out in the NHS five year forward view (NHS England et al 2014) and supportingstrategies, this represents a sustained push from the centre to deliver a step changein how the NHS uses digital technology.This briefing seeks to make sense of the national policy agenda in this area,providing a context for leaders developing local plans and a broad assessment ofprogress thus far. It includes an analysis of the remaining barriers to progress aswell as the opportunities for overcoming them. It draws on key policy documents,a literature review and quantitative data published by the relevant national bodies.Introduction 2
A digital NHS?Where have we come from?Digitisation in health care is not new, with computers first being used foradministrative, financial and research purposes in the 1960s, and Departmentof Health reviews dating back to the 1970s (Alderson 1976). The first nationalinformation technology (IT) strategy for the NHS came in 1992 (NHS ManagementExecutive 1992). Subsequent strategies in 1998 and 2002 led to the creation of theNational Programme for IT (NPfIT), later called Connecting for Health, whichaimed to create a single electronic care record for patients, connect primary andsecondary care IT systems, and provide a single IT platform for health professionals.This multi-billion-pound programme of investment dominated the digital agendaunder the Labour government. Running from 2002 to 2011, it failed to achieveits main objectives – including establishing an integrated electronic health recordsystem across secondary care – although it did establish some important nationaldigital infrastructure and services (National Audit Office 2013). Overly centraliseddecision-making, combined with a lack of local engagement, meant that users’ needswere poorly understood and providers were directed to implement at pace systemsthey had little say over (National Advisory Group on Health Information Technology inEngland 2016). In contrast, digitisation in general practice has been much morewidespread, with almost all GPs using electronic health records and computers intheir interactions with patients; something described in the Wachter review (2016).By the time Jeremy Hunt took up his post as Secretary of State for Health in 2012,NPfIT was all but wound down, though some contracts will continue into the 2020s.In 2013, he challenged the NHS to ‘go paperless’ by 2018 (Hunt 2013). This ambitionwas expanded on in the NHS five year forward view (NHS England et al 2014) andsubsequently extended to 2020. The National Information Board was set up to leadthis strand of work and to support the health and care system to deliver the digitaltransformation set out in the Forward View.Where have we come from? 3
A digital NHS?What are the potential benefitsof digitisation?It is often remarked that technological change has been much slower in healthcare than in other sectors such as banking and retailing, where technology haswrought significant changes in the relationship between service providers and theircustomers. This may be a reasonable analogy for online transactions (for example,ordering a prescription or making an appointment is similar to arranging a banktransfer or buying a train ticket). Being able to do these things online would bemore convenient for many people, although on its own would hardly amount to atransformation in patients’ experience of health care.However, technology has the potential to bring about a more fundamentalchange in the relationship between patients and health professionals. Greateradoption of technology and using it more effectively present opportunities to driveimprovements in quality, efficiency and population health (Imison et al 2016) andrevolutionise patient and user experience (Ham et al 2012) in a number of ways. It could help put people in control to take a more active role in their own healthand care (Klasnja and Pratt 2012) by providing access to relevant, high-qualityinformation and facilitating peer support online (Gretton and Honeyman 2016). It can support improvements in the safety and quality of care – for example,by reducing the risk of mis-identification and other avoidable errors(NHS Connecting for Health and NHS National Patient Safety Agency 2009). For clinicians, it may mean less time and effort in accessing information aboutpatients; remote monitoring can help clinicians better understand the progresspatients are making and ultimately help to deliver better health outcomes. It can facilitate advances in medical practice – for example, through the useof advanced analytic techniques, such as machine learning, to support clinicaldecisions and supporting personalised treatments based on analyses of people’sgenomes (Gretton and Honeyman 2016).What are the potential benefits of digitisation? 4
A digital NHS? Data captured by digital technologies could improve service planning, help aligncapacity more closely with demand (Imison et al 2016) and enable new serviceconfigurations – for example, GP federations where practices co-ordinate andfacilitate patient access through online hubs (Castle-Clarke et al 2016). IT, data systems and information sharing are critical to delivering integratedcare and can help to co-ordinate care delivered by professionals across differentorganisations and even across patients’ wider support networks. It can help deliver efficiency improvements. McKinsey estimated that modernhealth systems can save between 7 per cent and 11.5 per cent of their healthexpenditure (London and Dash 2016), while a study commissioned by NHSEngland estimated annual savings of 10 billion or more would come aftercommensurate investment in this agenda (Dunhill 2015). However, thecalculations behind this have not been published, leading many to questionwhether it is a realistic estimate.What are the potential benefits of digitisation? 5
A digital NHS?What is the national vision andhow much progress has beenmade towards it?The Forward View built on Jeremy Hunt’s challenge to the NHS to ‘go paperless’,outlining ambitions to ‘exploit the information revolution’ to help close the threegaps identified (care and quality, funding and efficiency, health and wellbeing). Itpromised to take a different, more even approach to policy, in contrast to the recentoscillation between two poles. ‘Letting a thousand flowers bloom’, as the ForwardView described much of the NHS’s approach to digital technology in recent years,has resulted in fragmentation and systems that do not work together, while overcentralisation has led to systems that do not meet local need. In future, nationalbodies are to focus on providing the ‘electronic glue’ and national standards forinteroperability to enable different parts of the system to work together, whileallowing local partners to make decisions on what they need in their area.The National Information Board report, Personalised health and care 2020(PHC2020), set out core priorities and a framework for action for delivering theForward View’s vision (National Information Board 2014). Local implementationwas to the fore, to be driven by ‘local digital roadmaps’. Led by clinicalcommissioning groups (CCGs), these roadmaps set out a five-year vision for howlocal areas – having come together to form 89 ‘footprints’ across England – aimto improve digital technology, strategy and organisational leadership (referred tocollectively as ‘digital maturity’) and deliver the paperless vision by 2020. Localdigital roadmaps were submitted in June 2016 and will now be aligned withthe 44 sustainability and transformation plans (STPs) currently being finalised(see The King’s Fund 2016b).In early 2016, Jeremy Hunt announced that more than 4 billion had been set asidefor digital and technology projects in the NHS over the course of this parliament,including 1.8 billion to meet the ‘paperless at the point of care’ ambition.What is the national vision and how much progress has been made towards it? 6
A digital NHS?Most recently, the Wachter review made a series of recommendations to theDepartment of Health and NHS England on their efforts to digitise secondary care.These included: the appointment of a national Chief Clinical Information Officer (CCIO) tooversee NHS clinical digitisation efforts CCIOs in every trust to lead the development of clinical information systems,supported by a new cadre of trained, professional clinician-informaticians additional funding and a phased approach to implementation with a revisedtarget for all trusts to reach ‘digital maturity’ by 2023 ensuring that interoperability is a core goal and feature of a digitised NHS a national engagement strategy, robust independent evaluation andestablishment of digital learning networks to support implementation.The Department of Health has not formally responded to the report so it is not yetclear how much of it will be adopted as policy. However, the Secretary of State andNHS England have responded positively and some recommendations are alreadybeing implemented, so it is clear that the report will have a significant impact on theapproach taken to digitisation across the NHS.This next section of this briefing looks in more detail at the key commitments madeprior to Wachter, and what we know about progress so far, grouped under threebroad themes: interoperable electronic health records patient-focused digital technology ‘secondary uses’ of data, transparency and consent.What is the national vision and how much progress has been made towards it? 7
A digital NHS?Interoperable electronic health recordsThe main commitments of the Forward View and PHC2020 in this area are as follows: by 2018, clinicians in primary care, urgent and emergency care, and other settings willhave gone ‘paperless’ – ie, will be using digital patient records only. a set of national standards and interoperability requirements will be agreed in 2015and rolled out across the system by 2020 by 2020, digital care records will be interoperable and in real time.The Wachter review suggests a phased approach to digitisation in acute hospitals andproposes a new target for all trusts to achieve ‘digital maturity’ by 2023.Electronic health records are digital records of a patient’s health and care (see box).Provided that certain conditions (mainly related to interoperability) are met, usingdigital health records should allow the whole record (or relevant information fromit) to be shared quickly, securely and in a standard way between health professionalsto support patient care, forming an ‘integrated’ electronic health record. Thecomplex mix of systems and practices in the NHS at present means that this isnot happening as often as it could. It is this vision that local commissioners andproviders are being asked to achieve. This goal is also a fundamental building blockfor much of the rest of the strategy to harness digital technology, as the healthrecord can be a rich source of useful information for many different purposes.What is the national vision and how much progress has been made towards it? 8
A digital NHS?Health records explainedA health record is a set of information about a person’s contact with a health care provider.Health records currently come in a range of formats (paper and electronic) and arestored using a range of systems. They include various pieces of information (eg, currenttreatments, test results, clinical notes, care plans, correspondence between professionals).Traditionally, in England, the most comprehensive records are those created and held bygeneral practitioners (GPs). When clinicians in other parts of the system need a patient’srecord (or part of it), they can request it. This information has typically been shared byletter, email, fax or phone. Hospital doctors treating patients who are admitted urgentlywill often not have access to an up-to-date record, relying on the hospital’s latest record forthe patient (if one exists) until the record arrives from primary care. Paramedics often donot have access to any NHS information about patients when attending emergencies.The Summary Care Record, a national service provided by NHS Digital, gives basicinformation (allergies and ongoing medication) to those with systems that can access it.When clinicians interact with patients in settings outside primary care, they will createtheir own set of records covering that interaction – often on multiple systems, dependingon the specialty. A summary of this information is fed back to GPs, typically in the form ofa letter from the person responsible for care. GPs then update their records accordingly.Other sources:For more information see: NHS Choices, ‘Your health and care records’Parliamentary Office of Science and Technology note, ‘Electronic health records’In primary care, the vast majority of practices have some form of electronic healthrecord system (The Commonwealth Fund 2015). This widespread adoption hasbeen driven by the fact that, since 2007, most primary care IT systems in England(75 per cent) have been centrally funded, with commissioners choosing an approvedsystem on behalf of their local GP practices via the GP Systems of Choice (GPSoC)framework. This approach has led to market consolidation (Hampson et al 2015),with EMIS Health and TPP systems covering about 90 per cent of patients inEngland (Health and Social Care Information Centre 2016b).What is the national vision and how much progress has been made towards it? 9
A digital NHS?Beyond primary care, digital systems are more diverse and fragmented. In late2015, all 239 NHS trusts and foundation trusts self-assessed their existing digitalcapabilities (see Figure 1). This process revealed that: information in acute trusts is less digitised and less structured and they are lessable to share information digitally a similar but slightly improved picture exists among community trusts mental health trusts seem further ahead, with most reporting near-fulldigitisation of clinical information and a greater capacity to share information.Figure 1 The digital availability of notes across trustsWhat proportions of clinical notes are available digitally in your organisation?8070Percentage of trusts6050403020100No response0%1% – 20%21% – 40%41% – 60%61% – 80%81% – 100%Don’t KnowPercentage of notes availableAcuteAmbulanceCommunityMental healthSource: NHS England 2016cNote: Figure shows results from one survey question that is broadly representative of the results frommany of the survey questionsThe same assessment exercise is now available (but not mandatory) for social careproviders. No results have been published as yet.As already noted, local digital roadmaps are the main mechanism for supportingand driving the adoption of digital records and information sharing (NationalInformation Board 2016). These roadmaps describe how local areas will put inWhat is the national vision and how much progress has been made towards it? 10
A digital NHS?place 10 ‘universal capabilities’ by 2018, including information sharing acrossgeneral practice, secondary care and social care, and patient access to records andtransactions. Existing projects around integrating information will now becomemajor parts of the roadmap. Local progress will be measured through the CCGImprovement and Assessment Framework and similar frameworks for providers(NHS England 2016b; National Information Board 2016).To support hospitals to progress, 12 of the most digitally advanced acute trusts wererecently selected as new ‘global digital exemplars’, each receiving up to 10 millionfrom NHS England and partnering with international organisations to develop goodpractice and ‘deliver pioneering approaches to digital services’ (NHS England 2016a).A further 20 trusts will become national exemplars, receiving up to 5 million eachas well as support from a new NHS digital academy.Some funding and support is available for primary care too; GPSoC moniesallocated to CCGs have increased this year and other measures are promised in theGeneral Practice Forward View (NHS England 2016d). The Estates and TechnologyTransformation Fund (formerly the Primary Care Transformation Fund), providing 900 million over five years, explicitly invites applications from practices throughtheir CCG for capital funding to improve technology, alongside applications forestates funding.A crucial part of the digital vision is ensuring that records are fully interoperable(see box).Interoperability explainedInteroperability is the ability of different health information systems and softwareapplications – both within and across organisational boundaries – to ‘talk to each other’ andshare information.There are different kinds of interoperability and, for this reason, calls for interoperabilityin health care should be understood as much more than simple exchanges of data. Thesystems involved need to be able to share information in such a way that other systemscan make good use of it, in standard structured forms. This poses technical challenges tosystem developers who have to agree to adopt consistent standards to enable meaningfulinformation sharing to happen.What is the national vision and how much progress has been made towards it? 11
A digital NHS?NHS England’s interoperability strategy reflects its desire to provide the ‘digital glue’to bind local systems together. As well as havin
An introduction to the digital agenda and plans for implementation Authors Matthew Honeyman Phoebe Dunn Helen McKenna September 2016. A digital NHS? Key messages 1 Key messages Digital technology has the potential to transform the way patients engage with services, improve the efficiency and co-ordination of care, and support people to manage their health and wellbeing. Previous .
econo lodge 69 room - 3 story 27,221 g.s.f. scale: 1/16" 1'-0" 0 8' 16' 32' overall plan typical upper floor staira linen stor. d/d d/d d/d d/d d/d d/d d/d d/d d/d d/d d/d king king king king king king king king king king king king king suite storage/ electrical king suite stairb
of NHS Direct, and led the team preparing New Labour's first White Paper, The New NHS: Modern, dependable, which laid the foundations and structure for the current NHS reform programme. He was a member of the top management board of the NHS for 12 years, between 1988 and 2000. His earlier career included 23 years in NHS management,
bunchberry dr nhs wms amb . burgundy ln nhs wms twl . burkwood dr nhs wms amb . burning tree st chs wms twl . burnock dr chs wms mbe . burr ridge rd nhs nms twl . burrwood ave nhs nms ang . burrwood st nhs nms ang . burt dr chs cms lce
NHS Long Term Plan Implementation Framework I 3 Introduction to the NHS Long Term Plan Implementation Framework 1.1 The NHS Long Term Plan, published in January 2019, set out a 10-year practical programme of phased improvements to NHS services and outcomes, including a
allowances are known as NHS Bursaries’1 and apply to courses qualifying students for certain professions (see Professions with training funded by NHS Bursaries). Students wishing to undertake these courses apply for an NHS bursary instead of Student Finance. NHS Bursaries are award
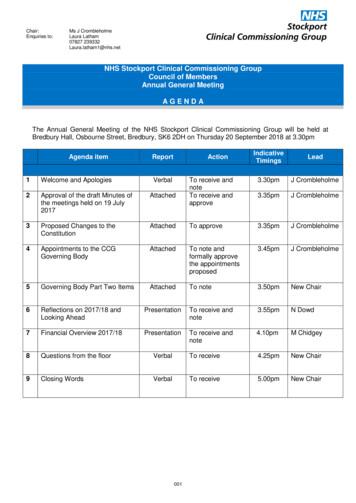
Dr Ranjit Gill . Chief Clinical Officer . NHS Stockport CCG . John Greenough . Lay Member . NHS Stockport CCG . Louise Hayes . Head of Communications and Engagement NHS Stockport CCG . Diane Jones . Director of Service Reform . NHS Stockport CCG . Dr Deborah Kendall .
Patient rights and NHS promises. 13. Part 4 - The things patients should do to help. 27. Part 5 - Rights and promises the NHS makes for NHS staff. 29. Part 6 - The things staff should do to help. 33. Part 7 - Telling the NHS
Currently working to align with work on RightCare'sFrailty Pathway and the Geriatric Medicine workstream of NHS Improvement's Getting It Right First Time (GIRFT) programme . NHS RightCare is a programme of NHS England Piers Glen NHS RightCare Delivery Partner 8 bpollington@nhs.net 07710 152763. Title: PowerPoint Presentation