Prostalac Hip System
Prostalac Hip SystemSurgical Technique
Prostalac Hip SystemThe Prostalac Hip System is engineered to provide a functional short-term total hipreplacement for those patients who need a two-stage procedure to treat a confirmedinfection of their total hip replacement and where vancomycin and tobramycin are themost appropriate antibiotics for treatment of the infection.The DePuy Prostalac Hip System is comprised of a cobalt chrome alloy core femoralcomponent, a cobalt chrome alloy modular femoral head, a one-piece ultra-high molecularweight (UHMWPe) polyethylene acetabular component, a PMMA stem centering deviceand antibiotic-loaded bone cement. It is designed to provide a means for limited mobilityof the patient following excision arthroplasty surgery and to function as a carrier device forantibiotic drugs for their local delivery within the periprosthetic space following excisionsurgery. The DePuy Prostalac Hip System is designed to remain in situ for approximatelythree months after which a second surgery is performed for implantation of a permanenttotal hip replacement prosthesis.The DePuy Prostalac Hip System combined with the DePuy Hip Revision Solutions portfolioallows you to be ready when hip infection revision surgery is required.2
One-piece poly acetabular component is available in size32mm inner diameter and 42mm outer diameter.Snap fit design captures the modularhead to optimize functionality32mm femoral head is availablein five offset optionsMade from durablecobalt-chromium materialIdeal for SmartSet MV bone cementLong stems are availablein standard offset with leftand right configurationsSimple and proven instrumentationAvailable in four stem lengths3
Surgical TechniqueStep 1—Patient PositioningPlace the patient in the lateral decubitusposition with the affected hip up. Obtainsufficient patient stability prior to draping andsurgical preparation. It is imperative that thepelvis remain stable but the affected leg maybe mobile. The patient must be in the truelateral position with orientation of the pelvisperpendicular to the table.Step 2—Initial incisionA lateral incision is made, curved from thefemoral shaft and middle of the greatertrochanter with slight posterior curve abovethe greater trochanter. The distal extent willdepend on the distal extent of foreign materialwithin the femur and surgical approach.Step 3—Exposing TissueDivide the subcutaneous tissue down tothe fascia, split the fascia in line with itsfibers curving posteriorly above the greatertrochanter into the gluteus maximus. Positiona Charnley retractor to hold the deep fasciaopen exposing the underlying tissues. Dividethe trochanteric bursa. At this point, basedon preoperative findings, surgeon preferenceand previous experience, an anterior lateral,posterior lateral, transtrochanteric or extendedtrochanteric osteotomy approach may bechosen. Whatever the choice, every effort mustbe made to leave soft tissue attached to thebone so that it will not be devascularized. Thisis particularly so in the case of an extendedtrochanteric approach, in which case careshould be taken to leave the abductors andvasti attached to the trochanteric and lateralcortex of the femur.4
At this point a wide subtotal capsulectomyis carried out to permit easy dislocation ofthe hip along with adequate exposure of theacetabular rim and proximal cortex of thefemur. A minimum of three synovial soft tissuebiopsies should be sent for bacteriologic study.A frozen section, white blood cell count andSTAT gram stain may be considered at thispoint as well.Step 4—Component RemovalBefore any of the Prostalac componentsare prepared or used, remove all existingimplanted components, cement and any otherforeign material (e.g., trochanteric fixationhardware, etc.) and thoroughly debride theinfected hip. This step is essential if a highsuccess rate is to be expected (Figure 1).Figure 1If there is doubt as to the adequacy of cementremoval, an intraoperative radiograph can behelpful at this point.Step 5—Acetabular PreparationReaming of the acetabulum is notrecommended in most cases. It may potentiallyremove valuable bone and irregularities thatare useful for interference fixation of thecement mantle used later in the case.Using manual tools, remove all foreign materialand soft tissue down to bleeding bone andtake care to identify and remove any hiddenpieces of bone cement (Figure 2).Figure 25
Surgical TechniqueStep 6—Cement MixingAcetabular COMPONENTThe antibiotic bone cement is prepared usingSmart Set MV Bone Cement, tobramycinsulfate and vancomycin hydrochloride, all inpowder form.Proper mixing of the antibiotics and bonecement is critical to the success of this device.The safety and potential benefit of the Prostalachip has only been demonstrated when usedwith tobramycin sulfate and vancomycinhydrochloride at the indicated doses.Figure 3Thoroughly mix one or two 40g bags of SmartSet MV bone cement and the recommendeddosage of tobramycin sulfate and vancomycinhydrochloride powders (see chart) with equaldistribution of each in an open bowl (Figure 3).Mixing is facilitated by adding the powderedcement and powdered antibiotics to a plasticcontainer and shaking it vigorously.Then add liquid monomer and carefully mix allingredients by hand with a spatula, pressingthe bone cement around the sides of thebowl until all ingredients are blended together(Figure 4). The antibiotic-loaded bone cementconsistency will be slightly different than bonecement without antibiotics. This is normal andwill not affect the setting and performance ofthe bone cement.Figure 4Recommended DosesAntibioticBone CementTobramycin sulfate3.6g powder andvancomycin hydrochloride1.0g powderPer Smart Set MV40g packetSmart Set MV Bone Cement RequirementsImplantBone Cement120 mm Std/High,150, 200, 240 mm1- 40g packageof bone cementAcetabular Cup61-2 packages(depending onindividual patient anatomy)The antibiotic-loaded bone cement will beready for use when the cement turns into afirm, doughy state, usually about 4-5 minutesafter adding the monomer. The cement is readywhen it no longer sticks to the surgical gloves.
Step 7—Acetabular Cup InsertionPlace the antibiotic-loaded bone cement intothe acetabulum in the doughy state and shapearound the acetabulum. Do not pressurize thecement, as deep intrusion is undesirable. Thisbone cement procedure is intended to achievestable, but not rigid fixation by interdigitationand interference fit with the irregularitiesof the surrounding bone. It also allows easyremoval during the second stage, withoutbone attached (Figure 5).Figure 5Insert the Prostalac cup into the cementmantle at an appropriate location and at anorientation of 45 degrees of abduction and20 degrees of anteversion. Use a cup impactorwith a 28 mm head impactor to position thecup and apply pressure until the cement hashardened (Figure 6).Step 8—Femoral PreparationUtilize the Endurance broaches to preparethe femoral envelope for optimal fit of theProstalac hip (Figure 7).Figure 6To confirm stem size selection, stem trialsshould be used to determine if a short or longstem is to be used. The long stems have ananterior bow to match the bow in the femur.120 mm Standard/High Offset Short StemAttach the size 1 broach to the Endurancehandle and broach down the medullary canal.Continue broaching using progressively largerbroaches until reaching the broach size thatcorresponds to the templated implant size.150, 200, 240 mm Long Left/Right StemsIf the long stems are to be used, then broachup to the size 3 broach. The long stem mold isbased on the size 3 broach.Figure 77
Surgical TechniqueStep 9—Trial ReductionTrial Neck SelectionStem SizeBroach SizeTrial Neck120 mm Std120 mm High150, 200, 240 mm Std1 to 51 to 53Size 1 StandardSize 1 HighSize 3 RevisionTrial neck segments and trial modular headsare available to use with the broach, to assessjoint stability and range of motion. Perform atrial reduction with a 5 Prostalac head trialto allow for two up or one down adjustmentin neck length without using a skirted femoralhead. During trial reduction, thoroughlyexamine range of motion and stability. Refer tothe chart at the back of this surgical techniquefor detailed base offset, neck length and leglength adjustment information.Note: The Prostalac trial head is slightlysmaller in diameter than the final head toallow easy reduction and dislocation since theacetabular component is a snap-fit design.Step 10—Femoral Mold PreparationA. Mold selection (Figure 8)120 mm Standard/High Offset Short StemsChoose the short mold that matches the lastbroach size used.Figure 8150, 200, 240 mm Long StemsChoose the left or right size 3 long mold tomatch the infected side of the hip.B. Mold Preparation (Figure 9)Before using the Prostalac molds, apply a thinlayer of sterile mineral oil inside the mold toallow easy removal of the implant after thecement has hardened around the implant.C. Mold AssemblyDo not assemble the molds at this time. Themold will be assembled in Step 12.Figure 98
Step 11—Cement MixingFemoral COMPONENTUsing a cement mix bowl, thoroughly mixone 40g bag of Smart Set MV bone cementand 3.6g of tobramycin sulfate and 1.0gof vancomycin hydrochloride powders withequal distribution of each (Figure 10). Mixingis facilitated by adding the powdered cementand powdered antibiotics to a plastic containerand shaking it vigorously.Then add liquid monomer and carefully mix allingredients by hand with a spatula, pressingthe bone cement around the sides of thebowl until all ingredients are blended together(Figure 11). The antibiotic-loaded bone cementconsistency will be slightly different than bonecement without antibiotics. This is normal andwill not affect the setting and performance ofthe bone cement.Figure 10The antibiotic-loaded bone cement will beready for use when the cement turns into afirm, doughy state, usually about 4-5 minutesafter adding the monomer. The cement is readywhen it no longer sticks to the surgical gloves.Figure 119
Surgical TechniqueStep 12—Femoral MoldCement ProcessCement insertion into short/long mold:When the antibiotic-loaded bone cementbecomes doughy, roll the cement into theshape of a tube (Figure 12).Lay the doughy antibiotic-loaded cement intoone side of the open mold, so that the mold isfilled from the bottom to the top (Figure 13).Figure 12The long mold is used for the 150, 200and 240 mm stem. Before insertion of theantibiotic bone cement into the long mold,place an appropriately sized cement spacerinsert in the bottom of the mold in order to fitthe appropriate stem. 150 mm stem—Long insert 200 mm stem—Short insert 240 mm stem—No insertFigure 13Assemble the other side of the mold to themold that contains the bone cement and lockit down with the mold nuts. Place the closedmold into a vertical position and lock into theinstrument base. Continue to push down thecenter of the mold and hand-pressurize anyremaining cement.Stem insertion into short/long mold:Immediately insert the appropriate short orlong stem implant into the opening at the topof the mold and push down until the neckregion of the stem reaches the top of the mold(Figure 14).Figure 1410
Excess cement may be used to place a thincovering around the neck of the implant,thereby minimizing the area of exposedforeign material. Take care that excess cementis not built up too much around the neck ortoo close to the taper, as it may interfere withproper seating of the femoral head.Hold the stem in place so that it remainscentered in the mold.Allow the cement to thoroughly harden,disassemble the mold and remove theProstalac implant (Figure 15).After removing the implant from the mold,remove any excess cement that may haveformed around the medial and lateral sides ofthe stem with a Rongeur.Note: Prior to insertion of the implant, aPMMA stem-centering device may be used tofacilitate the formation of a uniform thicknesscement mantle by keeping the core implantcentered with the mold instrument during thecement curing process.Alternatively, the two halves of the moldcan be packed with cement and the stemembedded in the cement and the moldassembled around the implant. This can beparticularly helpful with the 240 mm stem, asit requires considerable force to insert it intothe cement-filled mold. Pliers can then beused to facilitate compression and closure ofthe mold.Figure 1511
Surgical TechniqueStep 13—FEMORAL INSERTIONAND HEAD ATTACHMENTIntroduce the Prostalac antibiotic-loadedprosthesis into the canal by hand. Place afemoral trial head on the stem and gently tapwith a head impactor to seat the stem in thefemoral canal.Clean and dry the Articul/eze taper. Manuallyintroduce the appropriate 32 mm head byfirmly pushing and twisting the femoral headonto the taper. Engage the head with two tothree light mallet taps with the head impactor(Figure 16).Figure 1612The long-stemmed mold can be usedto reconstruct severe proximal femoraldeficiencies. In this case the stem is implantedinto the remnant of the femur and a bolus ofcement is packed around the prosthesis boneinterface proximally. Limb length is determinedby first inserting the stem in the canal and thefemoral head in the acetabular cup, restoringlimb lengths by longitudinal traction on thelimb and marking the stem at the appropriatelevel. The hip is then dislocated and theimplant is fixed with an extra mix of cementpacked around the bone prosthesis interface,such that a collar of cement provides forlongitudinal stability.
Step 14—Cup AttachmentCheck to assure that the bone cement hascured around the all-poly acetabular cup.Insert the femoral head into the cup and snapinto place (Figure 17).Prior to reduction, the inner surface of theacetabular cup must be clean and dry. Bloodand other fluids will act as a hydraulic block tothe snap-fit configuration. Position the femoralhead on the mouth of the acetabular cup andapply gentle abduction pressure to engage thesnap-fit configuration. Once engaged, it is verydifficult to disengage this articulation.Second-stage ReimplantationAt the time of the second stage reimplantation,the hip can be managed as if it were afailed total hip arthroplasty secondary toaseptic loosening. The surgical exposureand reconstructive implant selection is persurgeon preference. Antibiotic-impregnatedcement is not a necessary component of thesecond-stage reimplantation and cementlessimplants can be utilized. As the Prostalac stemis often incarcerated in the femur followingan extended trochanteric osteotomy, a repeatosteotomy is suggested to facilitate componentremoval. If not, care should be taken to removethe cement from the shoulder of the prosthesis.Figure 17Dislocation of the Snap-fit Acetabular CupThe snap-fit configuration is robust andmust be destroyed to allow for ease ofdislocation. This is accomplished by removinga thin strip of polyethylene from the lip ofthe acetabular cup. Approximately one-thirdthe circumference of the acetabular cup rimshould be removed, allowing for dislocation ofthe hip. The polyethylene is easily separatedfrom the mantle of cement in the acetabulum,and the acetabular cement is then split intopie-shaped pieces to facilitate extraction.13
Prostalac Hips - Piece-by-pieceACDSize(mm)StemBase OffsetLength(mm)(mm)BLegAdjustmentLength (mm)NeckAngle(degrees)120 Std1203526135120 High1204126135150 Std Left1504430135150 Std Right1504430135200 Std Left2004430135200 Std Right2004430135240 Std Left2404430135240 Std Right2404430135Note: All measurements are based on a 32 mm 5.0 Articul/eze head.Stem Offset32 mm Head SizeSize (mm) 1 5 9 13 17120 Std3235384143120 High3841444749150 Std Left4144475052150 Std Right4144475052200 Std Left4144475052200 Std Right4144475052240 Std Left4144475052240 Std Right4144475052Cementralizer InformationCat. No.Stem SizeMinimum RecommendedCementralizer (mm)1376-38-000120 mm-Size 1 Mold10.51376-38-000120 mm-Size 2 Mold10.51376-20-000120 mm-Size 3 Mold11.01376-21-000120 mm-Size 4 Mold12.01376-22-000120 mm-Size 5 Mold13.01376-20-000150, 200, 240 mm-Size 3 Mold11.014
Ordering InformationProstalac InstrumentationCat. No.DescriptionNeck SegmentsCat. No.Stem/Size2541-13-000Femoral Trial, Size 3, Left, 150 mm2521-01-501120 mm Std/Size 1 Std2541-23-000Femoral Trial, Size 3, Left, 200 mm2521-11-501120 mm High/Size 1 High2541-33-000Femoral Trial, Size 3, Left, 240 mm2521-23-501150/200/240 mm/Size 3 Revision2541-18-000Femoral Trial, Size 3, Right, 150 mm2541-28-000Femoral Trial, Size 3, Right, 200 mm2541-38-000Femoral Trial, Size 3, Right, 240 mm2541-41-000Mold Base2541-42-000Mold Jaw2541-43-000Mold Quick Release Nut2541-44-000Mold Handle2541-51-000Mold, Size 12541-52-000Mold, Size 22541-53-000Mold, Size 32541-54-000Mold, Size 42541-55-000Mold, Size 5Endurance InstrumentsCat. No.Description2521-01-510Broach Size 12521-02-510Broach Size 22521-03-510Broach Size 32521-04-510Broach Size 42521-05-510Broach Size 52521-00-506Broach Handle2521-00-508Broach Extractor2541-83-000Long Stem Mold, Size 3, Left, 240 mm2541-88-000Long Stem Mold, Size 3, Right, 240 mmImplantsCat. No.Size2541-83-165Long Stem Mold, 165 mm Insert1541-01-000120 mm Std2541-83-215Long Stem Mold, 215 mm insert1541-06-000120 mm High2541-91-320Trial Ball, 1 Neck, 32 mm OD1541-13-000150 mm Std-Left2541-92-320Trial Ball, 5 Neck, 32 mm OD1541-18-000150 mm Std-Right2541-93-320Trial Ball, 9 Neck, 32 mm OD1541-23-000200 mm Std-Left2541-94-320Trial Ball, 13 Neck, 32 mm OD1541-28-000200 mm Std-Right2541-95-320Trial Ball, 17 Neck, 32 mm OD1541-33-000240 mm Std-Left2541-96-000Extractor Instrument1541-38-000240 mm Std-Right2541-99-000X-ray Templates32 mm Femoral HeadsCat. No.Description1365-21-000 11365-22-000 51365-23-000 91365-24-000 131365-25-000 17Smart Set MV Bone CementCat. No.Description5450-50-00040gAll-Poly CupCat. No.Size1541-42-32042 OD x 32 IDAntibiotics/Sterile Mineral Oil (Supplied by hospital)DescriptionTobramycin Sulfate3.6g powder per40g Smart Set MV CementVancomycin Hydrochloride1.0g powder per40g Smart Set MV CementSterile Mineral Oil15
Essential Product informationThis Essential Product Information does not includeall of the information necessary for selection and useof a device. Please see full labeling for all necessaryinformation.INDICATIONSThe PROSTALAC Hip temporary prosthesis is indicatedfor use as a short-term total hip replacement (THR) inpatients who need a two-stage procedure to treat aconfirmed infection of their THR and where vancomycinand tobramycin are the most appropriate antibiotics fortreatment of the infection based on the susceptibilitypattern of the infecting microorganism(s).CONTRAINDICATIONSThe following conditions are contraindications for the useof the PROSTALAC Hip temporary prosthesis implantsystem:1. Patient is immunocompromised, nutritionally deficientand/or is otherwise systemically compromised tothe degree that a two-stage excision arthroplasty iscontraindicated;2. Destruction of the proximal femur that precludessupport of the PROSTALAC temporary femoralprosthesis3. Destruction of acetabulum that precludes support ofthe temporary acetabulum component;4. Loss of musculature, neuromuscular compromise orvascular deficiency in the affected limb rendering theprocedure unjustified;5. Poor bone quality, such as osteoporosis, where, inthe physician’s opinion, there could be considerablemigration of the prosthesis and/or a considerablechance of fracturing the femoral shaft;6. Insufficient bone stock to allow for a soundbiomechanical reconstruction for a permanent totalhip replacement prosthesis, i.e., resection arthroplastyor Girdlestone’s procedure is required;7. Infection cannot be confirmed;8. Unable to remove all infected THR devicecomponents;9. Pathogens are resistant to antibiotics to be locallyadministered to treat the infection;1610. Patient sensitivity to antibiotics to be locallyadministered to treat the infection;11. Systemic infection or a secondary remote infection iseither confirmed or suspected; and/or12. Patient does not have a total hip replacementprosthesis, e.g., hip infection is secondary to septicarthritis, trauma, ORIF, osteotomy, arthrodesis, etc.WARNINGS AND PRECAUTIONSThe patient’s wound drainage fluids should not bere-infused during or following the PROSTALAC HipTemporary Prosthesis surgery. Wound drainage followingPROSTALAC Hip Temporary Prosthesis surgery containshigh levels of antibiotics eluted from the device and reinfusion of this fluid has the potential for the introductionof large quantities of antibiotics into the systemiccirculation.Peak and trough serum concentrations of tobramycinsulfate and vancomycin hydrochloride should bemonitored periodically during intravenous administrationof these antibiotics in the presence of the PROSTALAC Hip System to avoid potentially toxic levels. Tobramycinsulfate and/or vancomycin hydrochloride administeredby the intravenous route have the potential for causingototoxicity and nephrotoxicity. The PROSTALAC HipSystem should be used with caution in patients who maybe predisposed to tobramycin sulfate and vancomycinhydrochloride toxicity, since combined PROSTALAC andsystemic administration of these antibiotics may result inhigher than expected serum levels. Patients with the riskfactors of advanced age, preexisting renal dysfunction,dehydration, receipt of large cumulative antibiotic doses,or concurrent or sequential use of other nephrotoxicand/or neurotoxic antibiotics are at increased risk oftoxicity. Please consult the product labels for tobramycinsulfate and vancomycin hydrochloride for a complete listof adverse events, as well as for information regardingsystemic administration.The PROSTALAC Hip Temporary Prosthesis should notbe re-implanted. Even though the implant may appearundamaged, it may be fatigued from previous stressesand may have developed microscopic imperfections,which may lead to implant failure.Consult product labels for the bone cement used inconjunction with the PROSTALAC .
The patient must be informed as to the necessity ofadherence to the physician’s instructions regarding theprotected weight bearing throughout the implantationperiod and the need for additional surgery to explantthe PROSTALAC Hip Temporary Prosthesis. ThePROSTALAC Hip temporary prosthesis system has beendesigned to withstand approximately three months ofprotected weight bearing for a person being treatedfor infection of his/her total hip joint replacementprosthesis and is not intended as a permanent hipprosthesis implant. The following conditions, singularlyor concurrently, tend to impose severe loading on theaffected extremity, thereby placing the patient at higherrisk for failure of the PROSTALAC Hip temporaryprosthesis.Device risksLocal or systemic toxicity from the eluted antibioticsdelivered to treat the infection’ incomplete removalof necrotic and/or avascularized bone and othertissues, bone cement, previously implanted prostheticcomponents, fixation and/or reinforcement devices, e/g.,cerclage wires, cement restrictor devices, etc., therebyincreasing the likelihood for a recurrent or persistenthip infection; inability to eradicate the pathogen(s) dueto a resistance to, or ineffectiveness of, the vancomycinhydrochloride and tobramycin sulfate eluted from thePMMA; and/or the inability to regulate the dose ortreatment duration of the locally administered antibiotics;and decreased mechanical strength of the PMMA due tothe quantities of antibiotics contained within the PMMA.1. ObesityHip joint surgery risksRisks known or potentially associated with THRprosthesis surgery are also applicable to surgery with thePROSTALAC device. Adverse effects and complicationsthat may result from this surgery include: Femoral and/or acetabular perforation; fractures of the femur or bonesof the pelvis necessitating internal fixation; breakageof the prosthetic device components; damage to bloodvessels; temporary or permanent nerve damage resultingin weakness, pain, or numbness of the affected extremity;difficulty with insertion of the permanent or hip prostheticdevice components and/or difficulty with removal of thePROSTALAC Hip at the second stage surgery; subluxationand/or disllocoation of the hip joint implant components;arthrofibrosis; limb length discrepancy; phlebitis andthrombophlebitis, hematoma; delayed wound healing;wound problems (dehiscence., necrosis and superficialinfection); and extensive blood loss.2. Heavy labor3. Active sports participation4. Likelihood of falls5. Alcohol or drug addiction6. Unprotected weight bearingKeep prosthesis in the supplied protectors duringsterilization and until implantation. Do not allow contactof prosthesis with hard objects.ADVERSE EVENTSPotential adverse effects of the PROSTALAC Hip weredetermined from a single center, retrospective study of135 PROSTALAC Hip cases. The frequencies of thecomplications reported are available in the Instructionsfor Use.Many of the known or potential adverse effects orcomplications associated with single-stage exchangearthroplasty and two-stage excision arthroplasty forthe treatment of infected THR prostheses are alsoassociated with the PROSTALAC Hip temporaryprosthesis implant system.General surgical risksCardiovascular disorders, including venous thrombosis,pulmonary embolism, transitory hypotension, arrythmiasand myocardial infarction, and/or anesthesia-relatedadverse effects.17
Notes18
19
References:1. Gee, R. et al. “Radiography of the Prostalac (Prosthesis with Antibiotic-Loaded Acrylic Cement)Orthopedic Implant. AJR. 180 2003:1701-1706.2. Younger, ASE, C. Duncan, and B. Masri. “Treatment of Infection Associated with Segmental Bone Lossin the Proximal Part of the Femur in Two Stages with Use of an Antibiotic-Loaded Interval Prosthesis.”JBJS. 80-A 1998: 60-69.Printed in USA. 2010 DePuy Orthopaedics, Inc. All rights reserved.2.5M06100612-60-500 (Rev. 1)
The DePuy Prostalac Hip System is comprised of a cobalt chrome alloy core femoral component, a cobalt chrome alloy modular femoral head, a one-piece ultra-high molecular weight (UHMWPe) polyethylene acetabular component, a PMMA stem centering device and antibiotic-loaded bone cement
hip for this explanation of total hip replacement. There can be other reasons for the re-placement, but, in general, the hip replacement method will be similar. To understand a total hip replacement, you must first understand the structure of the hip joint. The hip joint is a ball-and-socket
Hip Fracture: Patient Education Handbook AdventHealth - Orthopedic Institute Orlando Understanding the Hip & Hip Fractures Anatomy and Function The hip is a ball and socket joint. The pelvic bone contains the cup shaped “socket” (acetabulum) that holds the “ball” (femoral head). Together they form your hip, and allow
each hip action and the primary muscle group it targets. Figure 8 is based on three hip movements: hip sway, hip tuck, and hip roll are the foundation for the Figure 8 training. With the hip roll, you rotate your hips a complete 360 degrees. This fires and stretches the back, sides, a
brace to limit hip flexion. Hip flexion limit to 45 degrees Quad sets, active-assisted and passive hip and knee flexion, ankle pumps Hip flexion ROM limit 60 flexion None None Weight bearing TDWB crutches Post-op hip brace Limit hip flexion to 45 Phase Two 2 to 6 weeks after surgery PWB 50%
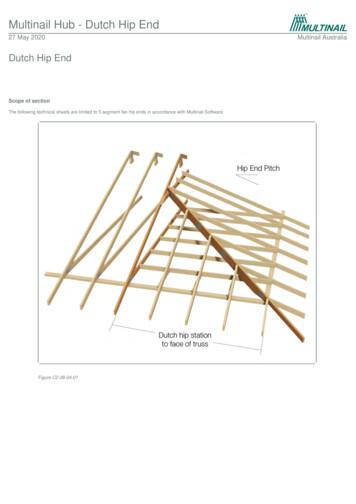
The “Hip Rafters” are positioned from the corner of the span / area and to the centre of the Dutch Hip Girder. Jack Top Chord to Hip Top Chord: Use ‘effective’ flat-head 3/75mm x 3.05Ø nails. Hip Top Chord to be mitre cut. Jack and Hip Top Chord to Waling Plate: Use 30 x 0.8mm looped
What causes a hip fracture? Falls are the most common cause of a hip fracture. As we get older, our strength and balance can reduce and our bones become thinner due to conditions like osteoporosis. What is a hip fracture? The hip is a ball and socket joint where the pelvis and thigh bone (femur) meet. A hip fracture is
A hip-hop dance routine incorporates the look, music, . The most real routines showcase a variety of hip-hop dance styles, signature moves and choreography conveying the character and energy of the street. Hip Hop International (HHI) Hip Hop International founded in 2000 is based in Los Angeles, California. Hip Hop International is
Contractors may use a Government employee's Government Purchase Card as long as the Contracting Office authorizes its use and the contractor notifies the Contracting Officer of all purchases made by the contractor during the billing period. Unauthorized Use of the GPC Page 7 of 29 Knowledge Review Computer supplies from a GSA schedule. Food, drinks, clothing, lodging or travel related expenses .