Prevalence And Nature Of Potential Drug-drug Interactions .
Eneh et al. BMC Infectious Diseases(2020) SEARCH ARTICLEOpen AccessPrevalence and nature of potential drugdrug interactions among hospitalized HIVpatients presenting with suspectedmeningitis in UgandaProsperity C. Eneh1, Katherine Huppler Hullsiek2, Daniel Kiiza3, Joshua Rhein3, David B. Meya3,4,5,David R. Boulware4 and Melanie R. Nicol1*AbstractBackground: Management of co-infections including cryptococcal meningitis, tuberculosis and other opportunisticinfections in persons living with HIV can lead to complex polypharmacotherapy and increased susceptibility todrug-drug interactions (DDIs). Here we characterize the frequency and types of potential DDIs (pDDIs) inhospitalized HIV patients presenting with suspected cryptococcal or tuberculous meningitis.Methods: In a retrospective review of three cryptococcal meningitis trials between 2010 and 2017 in Kampala,Uganda, medications received over hospitalization were documented and pDDI events were assessed. IBMMicromedex DRUGDEX online drug reference system was used to identify and describe potential interactions aseither contraindicated, major, moderate or minor. For antiretroviral DDIs, the Liverpool Drug Interactions Checkerfrom the University of Liverpool was also used to further describe interactions observed.Results: In 1074 patients with suspected meningitis, pDDIs were present in 959 (overall prevalence 89.3%) duringthe analyzed 30 day window. In total, 278 unique interacting drug pairs were identified resulting in 4582 pDDIevents. Of all patients included in this study there was a mean frequency of 4.27 pDDIs per patient. Of the 4582pDDI events, 11.3% contraindicated, 66.4% major, 17.4% moderate and 5% minor pDDIs were observed. Among allpDDIs identified, the most prevalent drugs implicated were fluconazole (58.4%), co-trimoxazole (25.7%), efavirenz(15.6%) and rifampin (10.2%). Twenty-one percent of the contraindicated pDDIs and 27% of the major onesinvolved an antiretroviral drug. Increased likelihood of QT interval prolongation was the most frequent potentialclinical outcome. Dissonance in drug interaction checkers was noted requiring clinicians to consult more than onedatabase in making clinical decisions about drug combinations.(Continued on next page)* Correspondence: mrnicol@umn.edu1Experimental and Clinical Pharmacology, University of Minnesota,Minneapolis, MN, USAFull list of author information is available at the end of the article The Author(s). 2020 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License,which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you giveappropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate ifchanges were made. The images or other third party material in this article are included in the article's Creative Commonslicence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commonslicence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtainpermission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.The Creative Commons Public Domain Dedication waiver ) applies to thedata made available in this article, unless otherwise stated in a credit line to the data.
Eneh et al. BMC Infectious Diseases(2020) 20:572Page 2 of 11(Continued from previous page)Conclusions: The overall prevalence of pDDIs in this population is high. An understanding of drug combinationslikely to result in undesired clinical outcomes, such as QT interval prolongation, is paramount. This is especiallyimportant in resource limited settings where availability of therapeutic drug monitoring and laboratory follow-upare inconsistent. Adequate quantification of the increased likelihood of adverse clinical outcomes from multipledrug-drug interactions of the same kind in a single patient is needed to aid clinical decisions in this setting.Keywords: Drug-drug interactions, HIV, Suspected meningitis, Acute care, Cohort studies, DDIsKey findingsThe result of this analysis shows that potential drugdrug interactions, ranging from minor to contradictedinteractions, in this subset of the population are significant and sometimes unavoidable. Although frequencyand type of drug-drug interactions have been previouslycharacterized in various populations, this is to our knowledge the first description of potential drug-drug interactions among hospitalized patients living with HIV andpresenting with co-morbidities like meningitis and tuberculosis. The findings will be of particular interest toclinicians in similar settings as this information can inform their monitoring and care of these patients especially given the vulnerabilities they face due to theircomorbidities.BackgroundThe beneficial effects of medications for acute andchronic management of HIV and comorbidities can belifesaving, but can also implicitly increase the risk ofdrug related problems [1]. The complexity of the treatment regimen for HIV patients presenting with suspected meningitis further increases their risk ofpolypharmacy. Polypharmacy is common among hospitalized adult patients and studies conducted in variousdeveloped countries report rates of potential drug-druginteractions ranging from approximately 1 to 66% [2].Drug-drug interactions (DDIs) contribute significantly toadverse drug events such as drug toxicity and ineffectivetherapy, and can also lead to increased hospital admissions [3, 4].Potential drug-drug interactions (pDDIs) involve concomitant administration of two drugs identified as having presumed or known clinically significantconsequences. Some potentially interacting drug pairsare still likely to be prescribed in combination with relatively high frequency due to limitations on alternativemedication therapy for specified treatment regimens [5,6]. The incidence of actual DDIs (aDDIs) is consistentlylower than that of pDDIs [7, 8]. The clinical outcome ofa pDDI is often not well defined because available datato track each potential interaction to its actual clinicalmanifestation is often inconsistent. However, epidemiological data suggest that the absolute number of patientswho do experience some kind of drug interaction-basedadverse event is high, especially in the presence ofknown risk factors like older age or polypharmacy [9].Hence, recognition of pDDIs is valuable as it createsknowledge that aids clinicians to prevent aDDIs.Resource-limited settings in sub-Saharan Africa oftenlack adequate therapeutic drug monitoring and other laboratory follow up to monitor outcomes from potentially interacting drugs. Identification of common pDDIsin this population, in addition to risk factors that canpredict the likelihood of an adverse effect is crucial forpatient safety. For patients on antiretrovirals (ARVs),pDDIs have been reported in the outpatient settings inlow and middle income countries [10, 11]. However,there is currently no data available for pDDIs in hospitalized HIV-infected patients presenting with life threatening co-infections such as meningitis. The aim of thisstudy was to characterize the frequency and types ofpDDIs involving HIV patients presenting with suspectedmeningitis in a hospital setting in Uganda.MethodsStudy setting and populationThis study was a retrospective review of three HIVassociated cryptococcal meningitis trials that enrolledpatients between 2010 and 2017 in Kampala, Uganda.The first trial enrolled antiretroviral (ARV)-naïve patients living with HIV with no previous history ofcryptococcal meningitis (NCT01075152, COAT) andrandomized participants to initiate antiretroviral therapy(ART) either early (1-week) or late (4–6 weeks) afterdiagnosis of cryptococcal meningitis [12]. The secondtrial consisting of an open-label pilot and the third arandomized phase 3 trial, enrolled both ART-naïve andART-experienced patients living with HIV and followedboth those presenting with first episode of cryptococcalmeningitis and those with previous history of cryptococcosis (NCT01802385, ASTRO) [13, 14]. In these threetrials, ART was generally initiated or switched 1–6 weeksafter diagnosis of cryptococcal meningitis. All participants had documented HIV-1 infection. Subjects withno available medication therapy record during their hospital stay were excluded. The original trials that providedthe data used for this analysis received written, informed
Eneh et al. BMC Infectious Diseases(2020) 20:572patient consent and were approved by the Mulago Research Ethics committee, the Uganda National Councilof Science and Technology and the National DrugAuthority.Data collectionDrug utilization review for de-identified patients wereextracted for the patient’s hospital stay (maximum of 30days drug record). Patients who were screened but notenrolled for either of the above mentioned original studies, but who had documented drug therapy during theirhospital stay were also included in this analysis. A pDDIwas recorded if the patient received the interacting drugpair on the same calendar day and were included regardless of drug dose or administration time. Fixed dosecombination (FDC) drugs such as tenofovir/lamivudine(TDF/3TC) are considered two individual drugs for thepurposes of identifying pDDIs. Extracted data was collated on Java with programming language on IntelliJIDE .Classification of drug interaction and strength of scientificevidenceIBM Micromedex DRUGDEX system was used to define the types of pDDIs [15]. The software has been previously validated [16]. Drug interactions were classifiedinto 4 main categories based on the likelihood and severity if the interaction were to occur; (i) contraindicated– the two drugs should not be used concurrently; (ii)major – the interaction may be life-threatening and/orrequire medical intervention to minimize or prevent serious adverse effects; (iii) moderate – the interaction mayresult in exacerbation of the patient’s condition and/orrequire an alteration therapy; and (iv) minor – the interactions have limited clinical effects that may include anincrease in the frequency or severity of the adverse effects, but generally would not require a major alterationin therapy.Specifically for interactions involving an antiretroviraldrug, clinical significance was further assessed and compared to recommendations from Micromedex using theonline University of Liverpool HIV drug interactionchecker [17]. This database has been curated for HIVdrugs and provides guidelines for management of clinically significant HIV drug interactions. This database iscontinuously updated as new information becomes available and clinicians can search this database either by individual drug name or by drug class.Statistical analysisDescriptive statistics were used and presented as meansand percentages unless otherwise specified. We analyzedcontinuous variables with t test or Mann-Whitney Utest, and we analyzed categorical variables with chi-Page 3 of 11square. We defined significance (p .05) in univariateanalysis. We conducted our statistical analysis usingRStudio Version 1.1.456 [18].ResultsMedication administration records were available for1074 patients presenting with suspected meningitis andscreened. The median age of participants was 35 years(IQR, 30, 41 years). Fifty-seven percent (617/1074) weremales. There was an average (range) of 8 (1–27) drugsprescribed per patient during the 30-day window. Table 1compares demographic characteristics of patients whohad at least one pDDI versus those who did not haveany. Significant differences in the two groups were observed in the number of medications administered, baseline CD4, initial diagnosis of tuberculosis andcryptococcal meningitis. Outcome characteristics suchas days of stay in hospital and total number of administered drugs were also significantly different betweengroups. (Table 1) No difference was noted between thetwo groups for age, gender and diagnosis of malaria.Of the total patients included in this sub-analysis, atleast one pDDI were in 959 (overall prevalence 89.3%).In total, 278 unique interacting drug combinations wereidentified resulting in 4582 pDDI events. (SupplementalTable 1) For all patients included in this study, therewas a mean frequency of 4.27 pDDIs per patient with anoverall range of 0–23 pDDIs. The majority (60%) of patients had 1–4 pDDIs, 31.3% had 5–10 pDDIs and 8.7%had 10 pDDIs. For severity classification of the 4582events, 11.3% were contraindicated, 66.4% were major,17.4% were moderate and 5% were minor pDDIs. Table 2summarizes the most frequently occurring pDDIs foreach level of severity along with level of scientific evidence and proposed summary of expected clinical effects. Eighty percent of the top occurringcontraindicated drugs were classified as having the potential to cause QT interval prolongation (Table 2). Nodifferences with respect to incidence of pDDIs was observed between the three study timelines included.Among all pDDIs identified, the most prevalent drugsimplicated are represented in Fig. 1. Fluconazole was themost prevalent drug interacting with other drugs at58.4% of overall pDDI events. Some of the other moreprevalent drugs also interacted with each other. For example, the most common interaction observed in thisstudy is a major interaction between fluconazole and cotrimoxazole (18.3% of the 4582 events) (Table 2). Potential effects of concurrent use of this drug pair per literature is an increased risk of cardiotoxicity including QTprolongation, torsades de pointes and cardiac arrest. Anyinteraction involving two individual medications thatcan prolong the QT interval is classified as a major orcontraindicated interaction on Micromedex.
Eneh et al. BMC Infectious Diseases(2020) 20:572Page 4 of 11Table 1 Comparison of characteristics of patients with and without at least one potential drug-drug interactionOne or more pDDI in study periodn 959No pDDI in study periodn 11517–30316 (32.9)42 (36.5)31–40403 (42.0)48 (41.7)41–50203 (21.2)20 (17.4)51 37 (3.9)5 (4.3)p value*DemographicsAge0.477Gender0.070Male560 (58.4)57 (49.6)Female399 (41.6)58 (50.4)18 (7–55)35 (16–209)No364 (38.0)105 (91.3)Yes595 (62.0)10 (8.7)Baseline diagnostics and investigationsCD4 (cells/mm3)Diagnosis of cryptococcal meningitis0.040 .001Diagnosis of tuberculosis0.049No852 (88.8)109 (94.8)Yes107 (11.2)6 (5.2)No946 (98.6)115 (100)Yes13 (1.4)0Diagnosis of malaria0.209GCS on admission0.00315588 (61.4)54 (47) 15369 (38.6)61 (53)4.58 (2.9–5.4)0 (0–6.6)0.053Number of administered drugs7 (5–9)3 (2–4) .001Days of stay in hospital16 (11–19)8 (4.5–13) .001CSF QCC (log10 CFU/mL)In-patient dataNumber of administered drugs, days in hospital, CD4, CSF QCC median (25th -75th percentile)Category of age, gender, diagnoses and GCSCSF Cerebral Spinal Fluid, QCC Quantitative Cryptococcal Culture, CFU Colony Forming Units – for patients presenting with suspected cryptococcal meningitis andfor whom CSF culture was collected and quantified (N 947 with at least one DDI; N 112 with no DDI)* t test of means for continuous variables and chi-square for categorical variables with significance at p .05Even though the design of the original trial studies excluded ART-experienced patients in COAT and ART initiation was delayed for half of the randomized patients in allthree studies, interactions involving at least one antiretroviral were still prevalent at 30.9% of overall pDDI events(regardless of severity). Antiretrovirals were involved in20.9% of contraindicated pDDIs and 27% of major pDDIs.Table 3 summarizes frequently occurring contraindicatedand major pDDIs involving an antiretroviral drug. Additionally, this table takes into consideration clinical recommendations for approaching each drug combination asidentified by the University of Liverpool HIV drug interaction website. For comparison, interactions involving antiretrovirals as identified by IBM Micromedex DRUGDEX system are included in Supplemental Table 1.DiscussionThe present study shows that the overall prevalence ofpDDIs in this population is high at 89.3%. Our currentstudy findings are affected by the class of medicationsthat are required for this patient population due to theunavailability of alternate drugs for management of complications of cryptococcal meningitis. For example, fluconazole and cotrimoxazole accounted for 18% ofoverall pDDIs events but both of these agents are warranted in this population. The incidence rate observed inthis study is, however, still congruent with published literature on pDDIs in developing countries. Overall prevalence of pDDIs in reports from hospital settings inUganda, Ethiopia, Pakistan and Iran range from 23 to86% [19–24]. In our study, moderate and minor
Eneh et al. BMC Infectious Diseases(2020) 20:572Page 5 of 11Table 2 Most occurring potential drug-drug interaction for each level of severitySeveritya Drug 1Drug 2% pDDIoverallbLevel ofevidencecProposed effect summaryFluconazoleOndansetron3.6FairRisk of QT interval prolongationFluconazoleHaloperidol2.8FairIncreased haloperidol exposure, risk of QT reased ritonavir exposure, risk of QT intervalprolongationArtanePotassium (oral)0.8FairGastrointestinal lesionsFluconazoleAtazanavir0.8FairIncreased atazanavir exposure, risk of QT ine0.7FairRisk of QT interval 0.2FairRisk of QT interval ne0.2FairRisk of QT interval sed extrapyramidal reactions and neurolepticmalignant syndromeFluconazoleQuinine0.1FairIncreased quinine levels, risk of QT interval oxicity (QT prolongation, torsades)EfavirenzFluconazole8.6FairRisk of QT interval prolongationCodeineFluconazole4.8FairIncreased codeine yCo-trimoxazoleHaloperidol2.4FairCardiotoxicity (QT prolongation, FluconazoleMetronidazole2.3FairRisk of QT interval prolongation and arrhythmiasEfavirenzOndansetron1.3FairQT interval prolongationCodeineEfavirenz1.1FairDecreased codeine efficacyCodeineMetoclopramide1.1FairIncreased CNS ole1.1FairRisk of QT interval prolongationCiprofloxacinFluconazole1.1FairRisk of QT interval prolongationFluconazoleTramadol0.9FairIncreased tramadol exposure and increased risk ofrespiratory toxicityEfavirenzRifampin0.9FairDecreased serum efavirenz concentrationFluconazoleZidovudine4.2GoodIncreased zidovudine serum ntDecreased fluconazole serum concentrationArtaneHaloperidol1.2GoodExcessive anticholinergic y (acetaminophen driven)Co-trimoxazoleZidovudine3.6GoodIncreased zidovudine serum concentrationMinoraSeverity classification for clinical purposes per IBM Micromedex DRUGDEX database definitionsbPercent of overall pDDI for study, % reported as (n/ 4582 total pDDI events) * 100cStrength of scientific data for the interaction per IBM Micromedex DRUGDEX database; (i) excellent – clearly documented well controlled studies support theinteraction; (ii) good – studies strongly suggest that interaction exists however there are not well controlled studies; (iii) fair – available evidence is poor butclinicians suspect the interaction exists based on pharmacology or the available evidence is good for a pharmacologically similar drug; and (iv) unknown –interaction documentation is unknown
Eneh et al. BMC Infectious Diseases(2020) 20:572Page 6 of 11Fig. 1 Drugs most implicated for any potential drug-drug interaction by percentage of occurrence in overall analysis. *Percentage calculated bydividing number of interactions involving identified drug with the total number of observed pDDI events (4582 total). Note that some of theidentified drugs also interact with each otherTable 3 Comparison of recommendation from drug interaction checkers for frequently occurring antiretroviral (ARV)- associatedcontraindicated and major potential drug-drug interactionsDrug 1Drug 2Proposed effect summary – MicromedexaScientific evidence; clinicalsignificance – LiverpoolbRecommended adjustment- LiverpoolbAtazanavirFluconazoleIncreased atazanavir exposure and risk ofQT interval prolongationLow; no interaction expectedNo prior dose adjustment necessaryEfavirenzCodeineDecreased opioid efficacyVery low; potential weakinteractionNo prior dose adjustment but monitoranalgesic effectEfavirenzFluconazoleIncreased risk of QT interval prolongationModerate; no interactionexpectedNo dose adjustment necessaryEfavirenzHaloperidolDecrease in drug 2 exposure; QT intervalprolongationVery low; potential weakinteractionNo prior dose adjustment isrecommendedEfavirenzMetronidazole Increased risk of QT interval prolongationVery low; no interactionexpectedNo dose adjustment necessaryEfavirenzOndansetronIncreased risk of QT interval prolongationVery low; no interactionexpectedNo dose adjustment necessaryEfavirenzRifampinDecrease in drug 1 serum concentrationHigh; potential weak interactionNo dose adjustment recommended inpatients weighing 50 kgRitonavirFluconazoleIncreased ritonavir exposure and risk ofQT interval prolongationVery low; no interactionexpectedNo prior dose adjustment recommendedTenofovirDFAtazanavirIncrease in drug 1 exposure and decrease Moderate; do not co-administerin drug 2 exposureAvoid co-administration, if necessary,monitor for adverse effectsDecrease drug 2 serum concentrationNo dose adjustment necessaryZidovudine PyrazinamideaVery low; no interactionexpectedEffect summary from IBM Micromedex DRUGDEX systemClinical recommendations as provided in the University of Liverpool HIV drug interaction websiteb
Eneh et al. BMC Infectious Diseases(2020) 20:572interactions that may require no changes to drug regimen represented 25% of the overall pDDIs observed.A further look at studies considering only Clinically Significant Drug Interactions (CSDI), defined as drug interactions that require a dosage adjustment or arecontraindicated due to high potential for clinical adverseeffects, report lower overall prevalence. CSDI incidenceobserved in Kenya and Uganda (both in outpatient settings) range from 18.8 to 33.5% [10, 11]. In the UnitedStates and Europe, studies have shown that pDDIs mayaffect 40–65% of all hospitalized patients [25, 26].While there is a relatively high prevalence of pDDI inreporting studies, actual drug-drug interactions (aDDIs)that lead to patient harm are often reported as beinglower [8]. However, the studies that show lower rates ofaDDIs have mostly been done in high-income countrieswith reliable access to monitoring [8, 9]. While loweraDDIs can be expected in resource limited settings aswell, it is not clear to what extent. Identifying pDDIscontinues to reinforce measures to keep aDDI low inthese settings. Other DDI studies in the literature concurwith our results that identify a significant difference inlikelihood of having a pDDI for patients with highertotal number of medications, extended hospital stay, andhigh risk diagnoses [4, 7, 19, 27].The patient population in this present study is uniqueas all those included had a confirmed HIV diagnosis.Hence, the pDDI observed warrant further discussion. Incontrast to the current study, potential drug-drug interactions reported in a general referral hospital in Ugandaidentified a different set of drug pairs as the most frequently occurring interactions. Lubinga et al identifiednon-steroidal anti-inflammatory drugs (NSAIDS) incombination with oral corticosteroids; loop diureticswith ACE-inhibitors; and loop diuretics with NSAIDS asthe top three occurring potential drug interactions intheir Ugandan cohort [19]. This is different in our studypopulation where we have observed that medicationsused in the management of chronic HIV comorbidities,ARVs and medications used for acute opportunistic infections such as cryptococcal meningitis or tuberculosispresented as the most implicated pDDI drugs. Furthermore, this difference is expected due to treatment guidelines that recommend specifically avoiding the use ofNSAIDS in our very ill population with a high risk ofconcurrent renal impairment, gastrointestinal bleeding,and anemia.The most frequently occurring pDDI in this study isconsidered a major interaction between fluconazole andco-trimoxazole. These two agents are used often in patients living with HIV in sub-Saharan Africa and is alsoa preferred combination for certain disease states. Fluconazole at high doses is used for induction therapy foracute management of cryptococcal meningitis and atPage 7 of 11lower doses for consolidation therapy. With unavailability of flucytosine, which is now the recommended firstline agent for treatment of cryptococcal meningitis, highdose fluconazole remains mainstay induction and consolidation therapy in many resource limited settings. Cotrimoxazole is the preferred drug for both the treatmentand prophylaxis of pneumocystis pneumonia in patientsliving with HIV. Individually, these two medications cancause QT interval prolongation and hence a combination is presumed to increase this risk. QT interval prolongation is an electrocardiographic (ECG) abnormalitythat has the potential to cause severe arrhythmias including torsade de pointes (TdP) and ventricular fibrillation. The extent of QT interval prolongation that isexpected and further translation to TdP has not beenspecifically quantified for this drug combination butthere is pharmacological speculation that this combination increases risk [15, 28]. Often the risk of QT interval prolongation can be mitigated in high resourcesettings if the patient is monitored for cardiac abnormalities during the induction phase with high dose fluconazole. In low resource settings however, continuouscardiac monitoring is often not feasible. With little prospective studies available to offer real world translationof the relative risk of this combination, it is often usedwith no adjustment to dosage. This practice will likelycontinue unless further research becomes availablewhich suggests changes should be made.Some studies have described a higher prevalence ofQT interval prolongation in HIV positive patients whencompared to HIV negative patients [29–31]. In additionto this baseline increase, there is additional risk due tonumerous drugs that are administered to HIV infectedpatients presenting to acute care settings. Arizona Center for Education and Research on Therapeutics(AZCERT) is an evidence based classification systemthat provides additional clinical guidance to cliniciansfor evaluating QT prolonging drugs. Drugs with QTprolonging properties are classified to one of four classes- “known risk”, “possible risk”, “conditional risk” (underspecific clinical conditions) and “special risk” (in patientswith congenital Long QT syndrome) [32]. Drugs in the“known risk” category have sufficient evidence to showthat they can cause QT prolongation and are also associated with TdP even at recommended doses while drugsin the “possible risk” category could potentially causeQT interval prolongation but lack evidence of association with TdP at recommended doses. Mied et al. notedin their pharmacological model, that drugs in the“known risk” category are associated with multiplicativeeffects when combined. A phenomenon not observedwhen drugs in the other categories are combined [33].In the second cryptococcal cohort used for this sub analysis, electrocardiogram QT intervals were measured in
Eneh et al. BMC Infectious Diseases(2020) 20:57253 patients at baseline, day 7, and day 14 of therapy, because a higher dose of sertraline was administered tothese patients. The results showed that QT intervals actually decreased over time [34]. It is interesting to notethat sertraline is in the “conditional risk” category forQT prolongation. Hence, it might be prudent for clinicians to become more familiar with drugs in the “knownrisk” category or have access to tools that can easilyidentify these drugs. In our study, prevalent drugs in the“known risk” category include fluconazole, ondansetron,levofloxacin, erythromycin, ciprofloxacin, azithromycin,and haloperidol [32].Treatment of other comorbidities such as malaria andtuberculosis (TB) also contributed to the pDDIs. For instance, pDDI of hepatotoxicity was identified with standard tuberculosis medicines of rifampin, isoniazid andpyrazinamide [35]. Liver function tests are a standard tomonitor for potential toxicity from these commonly prescribed combination that is part of first-line regimensfor tuberculosis. Guideline recommends that cliniciansperform liver function tests for those with symptoms ofhepatotoxicity [36]. Furthermore, hepatotoxicity is also aconcern when isoniazid is combined with high doses ofacetaminophen ( 4 g/day) and thus this combinationshould be used cautiously [37]. Management of patientsadmitted with malaria also requires caution as there arepotential contraindicated and major interactions roartemisinin-piperaquine were the most commonly implicated anti-malarials [38]. In combinationwith efavirenz, there is potential for reduced antimalarialefficacy and hence caution is advised with thesecombinations.Other important pDDI events that were observed inthis study includes the contraindicated interaction between artane (trihexyphenidyl or benzhexol) and oralpotassium potential
Keywords: Drug-drug interactions, HIV, Suspected meningitis, Acute care, Cohort studies, DDIs Key findings The result of this analysis shows that potential drug-drug interactions, ranging from minor to contradicted interactions, in this subset of the population are signifi-cant and sometimes unavoidable. Although frequency
Prevalence¶ of Self-Reported Obesity Among U.S. Adults by State and Territory, BRFSS, 2016 Summary q No state had a prevalence of obesity less than 20%. q 3 states and the District of Columbia had a prevalence of obesity between 20% and 25%. q 22 states and Guam had a prevalence of obesity between 25% and 30%. q 20 states, Puerto Rico, and Virgin Islands had a prevalence
Fiche n 1 : La taxe de séjour en chiffres Guide pratique : Taxes de séjour 8 0 500 1000 1500 Nature n 1 Nature n 2 Nature n 3 Nature n 4 Nature n 5 Nature n 6 Nature n 7 Nature n 8 Nature n 9 Taxe au réel ou taxe forfaitaire ? Source : Fichier téléchargeable sur www.impots.gouv.fr du 29/11/2019
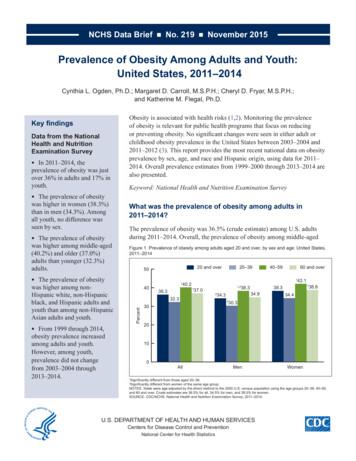
childhood obesity prevalence in the United States between 2003-2004 and 2011-2012 (3). This report provides the most recent national data on obesity prevalence by sex, age, and race and Hispanic origin, using data for 2011- 2014. Overall prevalence estimates from 1999-2000 through 2013-2014 are also presented.
prevalence proportion ratio is the ratio of the prevalence of disease in the exposed to the prevalence of disease in the unexposed. Note that the prevalence proportion ratio is mathematically identical to the risk ratio, . Microsoft PowerP
Nature and me 2 Based on research by the University of Derby's Nature Connectedness Research Group and experiences at National Trust places. Nature and me Five ways to strengthen the relationship between people and nature. Is this the key That feeling of connection with nature
The need for business to mainstream nature risk in corporate enterprise risk management 2. Provide the insights needed to develop practical roadmaps that address the most important drivers of nature loss, and build a nature-positive future, including: a. The most pressing business-related threats to nature, which require urgent individual and .
the mind's nature, based on replicable, empirical discoveries made by thou-sands of contemplatives throughout Asia. These are the phenomenological nature of consciousness, the essential nature of the mind, the ultimate nature of the mind, and the transcendent nature of consciousness that lies within the very ground of the whole of reality.
and South Cumbria, while the area with the lowest prevalence was London. The Quality and outcomes framework – prevalence, achievements and exceptions report is an annual report that focuses on 21 commonly occurring medical conditions, including asthma, hypertension, dementia and diabetes. It measures the prevalence with which